Abstract
Background
Short-term exposure to ambient nitrogen dioxide (NO2) is associated with adverse respiratory and cardiovascular outcomes. Supplementation of omega-3 polyunsaturated fatty acids (PUFA) has shown protection against exposure to fine particulate matter. This study aims to investigate whether habitual omega-3 PUFA intake differentially modify the associations between respiratory and cardiovascular responses and short-term exposure to ambient NO2.
Methods
Sixty-two healthy participants were enrolled into low or high omega-3 groups based on their habitual omega-3 PUFA intake. Each participant was repeatedly assessed for lung function, blood lipids, markers of coagulation and fibrinolysis, vascular function, and heart rate variability (HRV) in up to five sessions, each separated by at least 7 days. This study was carried out in the Research Triangle area of North Carolina, USA between October 2016 and September 2019. Daily ambient NO2 concentrations were obtained from an area air quality monitoring station on the day of outcome assessment (Lag0), 4 days prior (Lag1-4), as well as 5-day moving average (5dMA). The associations between short-term exposure to NO2 and the measured indices were evaluated using linear mixed-effects models stratified by omega-3 levels and adjusted by covariates including relative humidity and temperature.
Results
The average concentration of ambient NO2 during the study periods was 5.3±3.8 ppb which was below the National Ambient Air Quality Standards (NAAQS). In the high omega-3 group, an interquartile range (IQR) increase in short-term NO2 concentrations was significantly associated with increased lung function [e.g. 1.2% (95%CI: 0.2%, 2.2%) in FVC at lag1, 2.6% (95%CI: 0.4%, 4.8%) in FEV1 at 5dMA], decreased blood lipids [e.g. -2.6% (95%CI: -4.4%, -0.9%) in total cholesterol at lag2, -3.1% (95%CI: -6.1%, 0.0%) in HDL at 5dMA, and -3.1% (95%CI: -5.5%, -0.7%) in LDL at lag2], improved vascular function [e.g. 8.9% (95%CI: 0.6%, 17.2%) increase in FMD and 43.1% (95%CI: -79.8%, -6.3%) decrease in endothelin-1 at 5dMA], and changed HRV parameters [e.g. -7.2% (95%CI: -13.6%, -0.8%) in HFn and 13.4% (95%CI: 0.2%, 28.3%) in LF/HF ratio at lag3]. In the low omega-3 group, an IQR increase in ambient NO2 was associated with elevations in coagulation markers (von Willebrand Factor, D-dimer) and a decrease in HRV (very-low frequency); however, null associations were observed between short-term NO2 exposure and changes in lung function, blood lipids, and vascular function.
Conclusions
The results in this study imply that dietary omega-3 PUFA consumption may offer respiratory and vascular benefits in response to short-term exposure of healthy adults to NO2 levels below the NAAQS.
Trial registration
ClinicalTrials.gov (NCT02921048).
Similar content being viewed by others

Background
Respiratory diseases such as chronic obstructive pulmonary disease (COPD), lower respiratory infections, and lung cancers, and cardiovascular diseases such as ischemic heart disease and stroke, are worldwide leading causes of death [1]. Exposure to ambient air pollution has been associated with increased risk of respiratory and cardiovascular diseases and it is estimated to be responsible for 4.51 million deaths worldwide in 2019 [2].
Nitrogen dioxide (NO2) is a criteria air pollutant and formed from fossil fuel combustion in vehicular sources, power plants, and wildfires [3, 4]. Man-made sources in the U.S. are estimated to release approximately 12.3 million tons of nitrogen oxides (including NO2) in 2014 [5]. Short-term exposure to elevated concentrations of NO2 can cause airway irritation, exacerbate asthma and COPD, and increase hospital admissions due to respiratory or cardiovascular conditions [6, 7]. Although the implementation of the Clean Air Act has reduced ambient NO2 concentrations in the U.S., human exposure to NO2, especially at concentrations below the National Ambient Air Quality Standards (NAAQS) (1-hour: 100 ppb; annual: 53 ppb), is still associated with adverse health outcomes. For example, significant associations were observed between short-term or long-term exposure to ambient NO2 and all-cause cardiovascular and respiratory mortality [8,9,10,11,12]. Such adverse health impacts warrant further investigation of potential interventional approaches to mitigate the health effects of ambient NO2 exposure.
Dietary supplementation with fish oil from marine sources has been proposed as a potential intervention against the health effects of particulate matter [13]. Fish oil is rich in omega-3 polyunsaturated fatty acids (omega-3 PUFA), including eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA). EPA and DHA contain 5 and 6 carbon-carbon double bonds, respectively, and precursor for the synthesis of a class of lipid metabolites called specialized pro-resolving mediators (SPM) that orchestrate resolution of inflammation and a return to homeostasis [14, 15]. NO2 is a free radical species known to cause health effects through oxidative stress and inflammation [3]. Thus, the biochemical properties of omega-3 PUFA may offer protection against NO2 toxicity by direct reaction or by counteracting its pro-inflammatory effects. Previous studies have shown that omega-3 PUFA supplementation may lower the risk of cardiac dysrhythmia, inflammation, coagulopathy, endothelial dysfunction, and dyslipidemia induced by exposure to fine particulate matter (PM2.5) [16,17,18]. However, few have specifically investigated the respiratory and cardiovascular benefits of omega-3 PUFA against exposure to NO2 [11, 19]. To the best of our knowledge, this study is the first to investigate health benefits of omega-3 PUFA-rich diet against short-term exposure to ambient NO2 at concentrations below the NAAQS.
In the present study, healthy adult participants were enrolled based on their habitual omega-3 PUFA intake and stratified into low and high omega-3 PUFA groups. Focusing on lung function and subclinical cardiovascular parameters, this study aimed to investigate whether habitual dietary intake of omega-3 PUFA differentially modifies the associations between respiratory and cardiovascular responses and short-term exposure to ambient NO2.
Methods
Study participants and design
The study was conducted at the U.S. Environmental Protection Agency’s Human Studies Facility (HSF) in Chapel Hill, North Carolina, USA between October 2016 and September 2019, and all participants were residents of the Research Triangle area near HSF. Eligible participants meeting the following criteria were recruited: 25 – 55 years old; BMI between 19 and 35; having no history of respiratory or cardiovascular disease; non-smoker for at least one year; not taking β-adrenergic receptor blockers or anti-inflammatory drugs. Participants meeting at least one of the following criteria were enrolled into low or high omega-3 groups: (1) habitual dietary EPA + DHA intake ≤ 0.5 g/week (low) or ≥ 3.0 g/week (high) for at least six months based on a validated dietary questionnaire [20]; (2) red blood cell membrane omega-3 index ≤ 4.0% (low) or ≥ 5.5% (high) obtained from finger prick (OmegaQuant, Sioux Falls, SD). A total of 62 participants were enrolled into low (28) and high (34) omega-3 groups.
As shown in Additional Fig. 1, each participant had up to 5 study sessions separated by at least 7 days. Each session consisted of 2 consecutive days. On the first day, each participant was outfitted with a Holter monitor and recorded for 30 min while resting. On the second day, venous blood samples were collected, and spirometry, branchial artery ultrasound (BAU), 30-min Holter recordings were measured. All outcome measurements were conducted, and blood samples collected nearly same time of the day. Written informed consent was given by all participants prior to enrollment. The study was registered at ClinicalTrials.gov (NCT02921048) and approved by the Institutional Review Board of the University of North Carolina at Chapel Hill and the U.S. Environment Protection Agency.
Exposure assessment
Hourly concentrations of ambient NO2 were obtained from the Millbrook air monitoring station close to the HSF. Twenty four-hour average concentrations of NO2 were calculated from the hourly pollutant data between 9 AM and 8 AM, with a valid day defined as having at least 18 hourly measurements over the 24-h period. Concentrations were assigned to each visit session (the day of blood sample collection as lag0), as well as to 4 days prior (lag1–lag4), and 5-day moving average (5dMA). Twenty four-hour averages of temperature and relative humidity were collected from the same monitoring station.
Outcome assessment
Spirometry measurement
Spirometry was measured by a 10.2-L dry seal digital spirometer interfaced to a computer (SensorMedics Model 1022, SensorMedics, Palm Springs, CA). At least three sets of qualified data were obtained and the largest value was selected for forced vital capacity (FVC) and forced expiratory volume at the end of the first second (FEV1) as per American Thoracic Society guidelines [21].
Venous blood samples
A portion of whole blood samples was sent for lipid analysis (LabCorp, Burlington, NC). The other portion of blood samples was separated for plasma and stored at -80 ℃ prior to biomarker analysis. Commercially available multi-array plates were used to quantify levels of von Willebrand factor (vWF), tissue plasminogen activator (tPA), and D-dimer (MesoScale, Rockville, MD). Endothelin-1 was tested using an ELISA kit purchased from Peninsula Laboratories International (San Carlos, CA). All experiments were performed per manufacturers’ instructions.
Brachial artery ultrasound
Endothelial function was assessed by BAU using an Acuson Sequoia ultrasound machine (Siemens Healthcare, Malvern, PA) as described previously [17]. Briefly, resting blood pressure and baseline images of the right branchial artery at end diastole were captured. Flow–mediated dilation (FMD) was measured during reactive hyperemia induced by inflating a pneumatic tourniquet applied distal to the antecubital fossa to a suprasystolic pressure for 5 min. Hyperemic images were recorded for 90 s following cuff deflation. Brachial artery diameter (BAD) at baseline (BADb) and at maximum dilation (BADhyp) was measured using a customized software that utilizes edge-detection technology (Vascular Research Tools, Medical Imaging Applications, Coralville, IA).
Holter monitoring
HRV and repolarization parameters were measured using the last 5 min of Holter recording. Briefly, participants reclined in a dark room for 30 min and Holter were recorded using a H12+ 12-Lead ECG Recorder (Mortara, Milwaukee, WI). Assessed time-domain measurements include standard deviation of normal-to-normal (SDNN) and root-mean square of successive differences (rMSSD). Measured frequency-domain measurements include very-low frequency (VLF), normalized low frequency (LFn), normalized high frequency (HFn), and low-to-high frequency ratio (LF/HF).
Covariates
Participant sociodemographic characteristics were obtained via a standardized interview by medical staff at the baseline visit. The collected information included age (years, continuous), sex (male or female), race/ethnicity (Caucasian, African-American, Asian, or others), marital status (single, married, separated, or divorced), and educational attainment (graduate degree, college degree, high school/trade school or lower). Besides, height (m, continuous) and weight (kg, continuous) were measured at baseline to calculate the body mass index (BMI) by BMI = weight / height2.
Statistical analysis
A “gamm4” package in R (version 3.6.2) was employed to perform statistical analysis. Generalized linear mixed models with random participant effects were employed to analyze the association between short-term exposure to NO2 and the health parameters. Each visit of the participants was treated as a single data point. The dependent variables were log-transformed to improve normality in the residuals except for FEV1, FVC, FEV1/FVC, FMD, BADb, BADhyp, ET-1, LFn, and HFn. The statistical model was adjusted for age, sex, race, BMI, long-term and seasonal trends, day of the week, temperature, and relative humidity. The long-term and seasonal trends were controlled for by a penalized spline of time with eight degrees of freedom (df) per year. Temperature (lag0-1 for high temperatures and lag0-4 for low temperatures) and relative humidity (lag0-4) were incorporated as penalized splines with the df selected by the Generalized Cross Validation criterion. Linear terms of NO2 were included in the model separately to assess the immediate (lag0), delayed (lag1 to lag4), or cumulative (5dMA) effects. Between-group differences were assessed using a product term of omega-3 groups and air pollutant concentrations. The results were interpreted as percent change from the mean of the measured outcome per interquartile range (IQR) increase of NO2. Sensitivity analyses were conducted after excluding outcome outliers (defined as those lower than 1st Quartile-3×IQR and those higher than 3rd Quartile+3×IQR), using a 2-pollutant model with further adjustment for either PM2.5 or O3 concentrations obtained from the same air monitoring station, or adding additional covariates related with marital status and educational attainment. Statistical significance was set at a two-sided p < 0.05 for the air pollution effects and a two-sided p < 0.1 for the interaction with the two groups.
Results
Descriptive statistics
Twenty-eight participants in the low and 34 in the high omega-3 groups completed a total of 301 study sessions. Between the two groups, no statistical difference was observed in age, race / ethnicity, sex, smoking history, BMI, and systolic or diastolic blood pressure. The mean omega-3 index of the high omega-3 group was significantly higher than that of the low group (6.8% vs. 4.0%, p < 0.05) (Table 1). Descriptive statistics of all the outcome variables are summarized in Additional Table 1. During the study period, daily NO2 concentrations ranged from 0.8 to 24.2 ppb with a mean of 5.3 and an interquartile range (IQR) of 3.8 ppb. Temperature and relative humidity ranged from -8.6 to 31.1 °C, and 30 to 100%, respectively (Table 2). NO2 concentrations were weakly or moderately correlated with PM2.5, O3, or meteorological measurements. The correlations between PM2.5 and O3 concentrations and meteorological measurements were also considered weak or moderate (Additional Table 2).
Overview of findings
As summarized in Table 3, in the low omega-3 group, lung function and most cardiovascular markers were either not affected by an IQR increase in short-term NO2 concentrations or altered in an adverse direction. In contrast, in the high omega-3 group, significant associations were observed between short-term exposure to NO2 and increased lung function, decreased blood lipids, and increased vascular function. The magnitude and direction of the associations in the two groups varied by endpoints and exposure lags. We only report outcomes with significant percent change (with 95% CI) per an IQR increase of ambient NO2 concentration and significant interaction results (pinteraction) in the following sections. All detailed results for each outcome variable are available in the Additional materials.
Lung function
No significant association between short-term exposure to NO2 concentrations and lung function was observed in the low omega-3 group. In contrast, in the high omega-3 group, an IQR increase in NO2 concentration was associated with statistically significant increases in FVC at lag0 [0.9% (0, 1.8%)], lag1 [1.2% (0.2%, 2.2%)], lag2 [1.0% (0.02%, 1.9%)], and 5dMA [2.1% (0.5%, 3.7%)] (Fig. 1 A), and with an increase in FEV1 at 5dMA [2.6% (0.5%, 4.8%)] (Fig. 1B). We did not detect significant associations in FEV1/FVC ratio; and no between-group differences were observed for any of the three lung function parameters (Table 3).
Effects of omega-3 PUFA on lung function in response to short-term exposure to ambient NO2. Effect estimates (95% CI) in FVC (A) and FEV1 (B) were calculated relative to an IQR increase in NO2 concentrations at lag 0 to 4 days, as well as 5-day moving average in the low and high omega-3 groups. * p < 0.05 for significant association within a group. FVC: force vital capacity, FEV1: forced expiratory volume at the end of the first second, IQR: interquartile range
Blood lipids
In the low omega-3 group, an IQR increase in NO2 concentrations was not associated with changes in blood lipids. However, in the high omega-3 group, NO2 exposure was significantly associated with reductions in total cholesterol at lag2 [-2.6% (-4.4%, -0.9%)], LDL at lag2 [-3.1% (-5.5%, -0.7%)], and HDL at lag1 [-2.4% (-4.4%, -0.3%)], lag2 [-2.0% (-3.8%, -0.1%)], and 5dMA [-3.1% (-6.1%, -0.01%)]. We did not observe significant between-group differences (Fig. 2, Additional Table 4).
Effects of omega-3 PUFA on blood lipids in response to short-term exposure to ambient NO2. Effect estimates (95% CI) in total cholesterol (A), HDL (B), and LDL (C) were calculated relative to an IQR increase in NO2 concentrations at lag 0 to 4 days, as well as 5-day moving average in the low and high omega-3 groups. * p < 0.05 for significant association within a group. HDL: high-density lipoprotein, IQR: interquartile range, LDL: low-density lipoprotein
Coagulation and fibrinolysis
In the low omega-3 group, short-term NO2 exposure was associated with increases in D-dimer [11.0% (0.2%, 23.0%)] and vWF [5.4% (0.7%, 10.3%)] at lag0. In the high omega-3 group, NO2 exposure was associated with an increase in vWF levels at lag1 [6.7% (2.0%, 11.7%)], lag3 [4.7% (0.0, 9.6%), pinteraction = 0.026], and 5dMA [7.9% (1.0%, 15.4%)] (Fig. 3). No other significant associations or between-group differences were observed (Additional Table 5).
Effects of omega-3 PUFA on coagulation and fibrinolysis markers in response to short-term exposure to ambient NO2. Effect estimates (95% CI) in vWF (A) and D-dimer (B) were calculated relative to an IQR increase in NO2 concentrations at lag 0 to 4 days, as well as 5-day moving average in the low and high omega-3 groups. * p < 0.05 for significant association within a group. # pinteraction < 0.1 and ## pinteraction < 0.05 for significant differences in the effect estimates between groups. IQR: interquartile range, vWF: von Willebrand factor
Vascular function
Short-term NO2 exposure was significantly associated with increases in FMD at lag1 [5.7% (0.1%, 11.2%)], lag2 [5.7% (0.8%, 10.6%), pinteraction = 0.044], and 5dMA [8.9% (0.6%, 17.2%)] in the high omega-3 group, while no significant association was observed in the low group. Significant associations were observed between NO2 exposure and decreased ET-1 levels at lag3 [-25.6% (-50.0%, -1.2%)], lag4 [-22.9% (-45.9%, -0.01%)], and 5dMA [-43.1% (-79.8%, -6.3%)] in the high omega-3 group as well as at 5dMA [-54.2% (-93.2%, -15.2%)] in the low group (Fig. 4). We did not observe any other NO2 – associated changes in either group (Additional Table 6).
Effects of omega-3 PUFA on endothelial function markers in response to short-term exposure to ambient NO2. Effect estimates (95% CI) in FMD (A) and ED-1 (B) were calculated relative to an IQR increase in NO2 concentrations at lag 0 to 4 days, as well as 5-day moving average in the low and high omega-3 groups. * p < 0.05 for significant association within a group. # pinteraction < 0.1 and ## pinteraction < 0.05 for significant differences in the effect estimates between groups. ED-1: endothelin 1, FMD: flow-mediated dilation, IQR: interquartile range
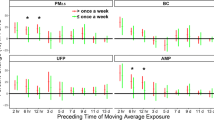
Heart rate variability
In the low omega-3 group, short-term NO2 exposure was significantly associated with decreased VLF at lag0 [-21.5% (-34.8%, -5.6%)]. In contrast NO2 exposure was associated with decreased HFn [-7.2% (-13.6%, - 0.8%)] and increased LF/HF ratio [13.4% (0.2%, 28.3%)] at lag3 in the high omega-3 group (Fig. 5). No other significant associations or between-group differences were observed in HRV parameters (Additional Table 7).
Effects of omega-3 PUFA on HRV markers in response to short-term exposure to ambient NO2. Effect estimates (95% CI) in HFn (A), LF/HF (B), and VLF (C) were calculated relative to an IQR increase in NO2 concentrations at lag 0 to 4 days, as well as 5-day moving average in the low and high omega-3 groups. p < 0.05 for significant association within a group. HFn: normalized high frequency, IQR: interquartile range, LF/HF: low-to-high frequency ratio, VLF: very low frequency
Sensitivity analysis
The associations between short-term exposure to NO2 and the biomarkers were robust in the two-air pollutant model after adjustment for simultaneous exposure to PM2.5 or ozone (Additional Table 8). In addition, the results remained stable after excluding outliers of the endpoints indicating that the statistically significant associations were not driven by them (Additional Table 9). Finally, we included marital status and education level as covariates in the statistical model and the overall results did not change, indicating that these socioeconomic proxies did not confound the overall findings (Additional Table 10).
Discussion
In this panel study, we investigated the modulative effects of omega-3 PUFA on the association between respiratory and cardiovascular effects and exposure to ambient NO2 in healthy participants. We observed that short-term exposure to ambient NO2 was associated with increased lung function and endothelial function, and lowered blood lipids among participants with high omega-3 PUFA levels.
NO2 is a gaseous and oxidant pollutant and inhalational exposure to ambient NO2 can induce oxidative stress and pulmonary inflammation [19, 22]. Omega-3 PUFA from marine sources may block oxidative damage to cells by acting as a target for reaction with NO2 [14], and increased availability of EPA and DHA may lead to higher levels of SPMs to promote resolution of inflammation caused by NO2 exposure. One randomized trial reported that fish oil supplementation reduced oxidative stress caused by short-term exposure to environmental oxidants including ozone and NO2 among young healthy participants [19]. Another cohort study found a beneficial effect of Mediterranean diet, rich in marine fish, against cardiovascular risk related to long-term exposure to NO2, although no clear role for omega-3 PUFA [11]. To our knowledge, the present study is the first to specifically investigate the modulating effects of dietary omega-3 PUFA on the association between respiratory and cardiovascular parameters and NO2 exposure in healthy adults.
In this study, exposure to low-level ambient NO2 was not associated with lung function changes among participants with low omega-3 PUFA. Although epidemiological evidence shows a possible link between ambient NO2 exposure and adverse respiratory effects [6, 23,24,25], null associations were observed between NO2 exposure and lung function reductions in human exposure studies [22]. For example, chamber studies reported that short-term exposure to 0.5-2.0 ppm NO2 did not induce any significant changes in lung function among healthy subjects [26, 27]. It is worth reiterating that the ambient NO2 concentration in the present study is much lower than the tested chamber levels as well as the current NAAQS and is therefore not expected to induce a significant respiratory response.
Paradoxically, NO2 exposure in this study was associated with significant increases in FVC and FEV1 among participants with high omega-3 PUFA levels. One possible explanation may be found in the reactivity of NO2 with the electron-rich centers in unsaturated fatty acids, such as EPA and DHA [28]. Rich in oxidizable carbon-carbon double bonds, EPA and DHA can react with NO2 to generate nitroalkene derivative, nitro EPA (NO2-EPA) and nitro DHA (NO2-DHA) [28]. These nitroalkenes can further decay or possibly be metabolized via a reaction facilitated by reductants such as ascorbate to release the gasotransmitter nitric oxide (NO), a potent receptor-mediated stimulus that acts through a specific signaling pathway to promote the relaxation of smooth muscle cells [29,30,31]. It is therefore tempting to speculate that the improvements in vascular and lung function associated with NO2 exposure are underlain by vasodilatory and bronchodilatory changes in smooth muscle tone, respectively, that are mediated by an increased availability of NO in the tissues of the participants with high omega-3 in this study.
In addition to increased FMD, decreased plasma ET-1 were observed in the high omega-3 group in association with NO2 exposure. While FMD reflects dilation of the brachial artery caused by NO released from endothelial cells in response to shear-stress, ET-1 is a potent endogenous vasoconstrictor that is inhibited by NO [32,33,34]. Short-term exposure to NO2 is not known to be associated with endothelial dysfunction or vascular constriction [35]; however, as suggested earlier, NO2-EPA and NO2-DHA could be formed when NO2 reacts with omega-3 PUFA creating a releasable source of NO that may have resulted in the observed improvement in endothelial function in the high omega-3 group [28,29,30]. Studies to validate the apparent beneficial effects of NO2 in subjects with high omega-3 and to investigate the mechanistic basis are warranted.
Significant changes in blood lipids were also only observed in the high omega-3 group, indicating that high omega-3 PUFA intake may lower blood cholesterol levels in response to NO2 exposure. In a manner analogous to the reaction with fatty acids, the reaction of NO2 on cholesterol can lead to formation of cholesteryl nitrite [36]. It is possible that the presence of omega-3 PUFA may promote the nitration reaction leading to decreased levels of both the “good” (HDL) and the “bad” (total cholesterol and LDL) cholesterols. Among the blood coagulation markers studied, vWF binds to factor VIII and promotes platelet adhesion to injured vasculature while D-dimer is a product of the fibrin degradation process [37]. The NO2-associated elevation in vWF and D-dimer levels at lag0 in the low omega-3 group indicate acute coagulation and fibrinolysis in response to NO2 exposure. However, the lag1 and cumulative (5dMA) impacts of ambient NO2 on vWF found in the high omega-3 group suggest that the oxidation of omega-3 PUFA by NO2 could be a double-edged sword as it could counteract the acute toxicity of NO2, but also lead to activation of pro-thrombotic pathways.
HFn is an index of heart rate variability that reflects parasympathetic activity specifically correlating heart rate variations related to the respiratory cycle [38]. Similarly, the LF/HF ratio measures the “sympatho-vagal balance” with a high LF/HF ratio indicating sympathetic dominance [38]. Low VLF power is associated with several adverse health outcomes including arrhythmic death and high levels of inflammation [38]. A cohort study showed that each 10 µg/m3 (approximately 5 ppb) increment in the average yearly NO2 concentration was associated with decreases in SDNN, LFn, and LF/HF ratio in elderly women [39]. In a controlled exposure study, NO2 at 500 ppb increased HFn 1-hour post-exposure in young healthy participants [26]. In the present study, we observed that in the low omega-3 group, NO2 was associated with a decrease in VLF; while in the high group, NO2 was associated with a significant reduction in HFn and elevation in LF/HF ratio. These results suggest that high omega-3 PUFA may modulate baroreflex and parasympathetic activities in response to NO2 exposure.
To our knowledge, this study is the first to suggest health benefits of omega-3 PUFA-rich diet against short-term exposure to low-level ambient NO2. In addition, in this study, we evaluated respiratory and cardiovascular effects of NO2 exposure using multiple lags of exposure as well as a cumulative effect of NO2 using a 5-day moving average. Although we only measured omega-3 index at the enrollment phase and did not monitor omega-3 index throughout the study period, dietary intake of EPA+DHA for each participant was recorded at each study session using a 24-hour dietary recall methodology, and the results indicate that the omega-3 PUFA intake levels maintained for both low and high omega-3 groups throughout the study (Lukens MK, Kerri L, Tong H, Hao C, Shen W: A comparison of Omega-3 Fatty Acids Intakes from Three Dietary Screening Tools, unpublished).
This study also has some limitations. First, although this observational study was a longitudinal design, it employed a relatively small sample size, thus caution is advised establishing causal inference of the findings. Second, this study used central air monitors rather than personal monitors for air pollution data, which could possibly introduce non-differential exposure misclassification and bias the effects towards the null. Third, we only recruited healthy participants, and it is likely that additional and larger effects could be observed among more susceptible subgroups. Fourth, it is also possible that volatile organic compounds could be confounding factors since they are highly correlated with NO2 production. In addition, some of the significant findings could be by chance as the significant association was only reported at 1 lag day.
Conclusions
This panel study suggests that participants with low intake of dietary omega-3 PUFA showed minimal respiratory effects in response to short-term exposure to ambient NO2 at concentrations below the NAAQS. In contrast, associations between improved pulmonary and vascular function and reduced blood lipid levels, and NO2 exposure were observed among participants with relatively high omega-3 PUFA. These findings suggest that increased dietary intake of omega-3 PUFA may offer health benefits against the impacts of short-term NO2 exposure in healthy adults.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BAU:
-
branchial artery ultrasound
- CI:
-
confidence interval
- DHA:
-
docosahexaenoic acid
- ET-1:
-
endothelin-1
- EPA:
-
eicosapentaenoic acid
- FEV1:
-
forced expiratory volume at the end of the first second
- FMD:
-
flow – mediated dilation
- FVC:
-
forced vital capacity
- HDL:
-
high-density lipoproteins
- HFn:
-
normalized high frequency
- HRV:
-
heart rate variability
- LDL:
-
low-density lipoproteins
- LFn:
-
normalized low frequency
- LF/HF:
-
low to high frequency ratio
- NAAQS:
-
National Ambient Air Quality Standards
- NO2 :
-
nitrogen dioxide
- PUFA:
-
polyunsaturated fatty acids
- RMSSD:
-
root mean square of successive differences
- SD:
-
standard deviation
- SDNN:
-
standard deviation of normal-to-normal beats interval
- tPA:
-
tissue plasminogen activator
- VLF:
-
very-low frequency
- vWF:
-
von Willebrand factor
References
The top 10 causes of death [https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death]
Collaborators GBDRF: Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet 2020, 396(10258):1223–1249.
Debbie J. Jarvis GA, Marie-Eve Heroux, Regula Rapp, Frank J. Kelly: Nitrogen dioxide. In: WHO Guidelines for Indoor Air Quality: Selected Pollutants. Geneva: World Health Organization; 2010.
Chen H, Samet JM, Bromberg PA, Tong H: Cardiovascular health impacts of wildfire smoke exposure. Part Fibre Toxicol 2021, 18(1):2.
2014 National Emissions Inventory, Version 2, technical support document [https://www.epa.gov/sites/production/files/2018-07/documents/nei2014v2_tsd_05jul2018.pdf]
Sinharay R, Gong J, Barratt B, Ohman-Strickland P, Ernst S, Kelly FJ, Zhang JJ, Collins P, Cullinan P, Chung KF: Respiratory and cardiovascular responses to walking down a traffic-polluted road compared with walking in a traffic-free area in participants aged 60 years and older with chronic lung or heart disease and age-matched healthy controls: a randomised, crossover study. Lancet 2018, 391(10118):339–349.
Mills IC, Atkinson RW, Anderson HR, Maynard RL, Strachan DP: Distinguishing the associations between daily mortality and hospital admissions and nitrogen dioxide from those of particulate matter: a systematic review and meta-analysis. BMJ Open 2016, 6(7):e010751.
Orellano P, Reynoso J, Quaranta N, Bardach A, Ciapponi A: Short-term exposure to particulate matter (PM10 and PM2.5), nitrogen dioxide (NO2), and ozone (O3) and all-cause and cause-specific mortality: Systematic review and meta-analysis. Environ Int 2020, 142:105876.
Meng X, Liu C, Chen R, Sera F, Vicedo-Cabrera AM, Milojevic A, Guo Y, Tong S, Coelho M, Saldiva PHN et al: Short term associations of ambient nitrogen dioxide with daily total, cardiovascular, and respiratory mortality: multilocation analysis in 398 cities. BMJ 2021, 372:n534.
Atkinson RW, Butland BK, Anderson HR, Maynard RL: Long-term Concentrations of Nitrogen Dioxide and Mortality: A Meta-analysis of Cohort Studies. Epidemiology 2018, 29(4):460–472.
Lim CC, Hayes RB, Ahn J, Shao Y, Silverman DT, Jones RR, Thurston GD: Mediterranean Diet and the Association Between Air Pollution and Cardiovascular Disease Mortality Risk. Circulation 2019, 139(15):1766–1775.
Eum KD, Kazemiparkouhi F, Wang B, Manjourides J, Pun V, Pavlu V, Suh H: Long-term NO2 exposures and cause-specific mortality in American older adults. Environ Int 2019, 124:10–15.
Tong H: Dietary and pharmacological intervention to mitigate the cardiopulmonary effects of air pollution toxicity. Biochim Biophys Acta 2016, 1860(12):2891–2898.
Albert BB, Cameron-Smith D, Hofman PL, Cutfield WS: Oxidation of marine omega-3 supplements and human health. Biomed Res Int 2013, 2013:464921.
Serhan CN, Levy BD: Resolvins in inflammation: emergence of the pro-resolving superfamily of mediators. J Clin Invest 2018, 128(7):2657–2669.
Romieu I, Tellez-Rojo MM, Lazo M, Manzano-Patino A, Cortez-Lugo M, Julien P, Belanger MC, Hernandez-Avila M, Holguin F: Omega-3 fatty acid prevents heart rate variability reductions associated with particulate matter. Am J Respir Crit Care Med 2005, 172(12):1534–1540.
Tong H, Rappold AG, Caughey M, Hinderliter AL, Bassett M, Montilla T, Case MW, Berntsen J, Bromberg PA, Cascio WE et al: Dietary Supplementation with Olive Oil or Fish Oil and Vascular Effects of Concentrated Ambient Particulate Matter Exposure in Human Volunteers. Environ Health Perspect 2015, 123(11):1173–1179.
Lin Z, Chen R, Jiang Y, Xia Y, Niu Y, Wang C, Liu C, Chen C, Ge Y, Wang W et al: Cardiovascular Benefits of Fish-Oil Supplementation Against Fine Particulate Air Pollution in China. J Am Coll Cardiol 2019, 73(16):2076–2085.
Jiang Y, Wang C, Lin Z, Niu Y, Xia Y, Liu C, Chen C, Ge Y, Wang W, Yin G et al: Alleviated systemic oxidative stress effects of combined atmospheric oxidant capacity by fish oil supplementation: A randomized, double-blinded, placebo-controlled trial. Ecotoxicol Environ Saf 2019, 184:109598.
Shen W, Weaver AM, Salazar C, Samet JM, Diaz-Sanchez D, Tong H: Validation of a Dietary Questionnaire to Screen Omega-3 Fatty Acids Levels in Healthy Adults. Nutrients 2019, 11(7).
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, Crapo R, Enright P, van der Grinten CP, Gustafsson P et al: Standardisation of spirometry. Eur Respir J 2005, 26(2):319–338.
Hesterberg TW, Bunn WB, McClellan RO, Hamade AK, Long CM, Valberg PA: Critical review of the human data on short-term nitrogen dioxide (NO2) exposures: evidence for NO2 no-effect levels. Crit Rev Toxicol 2009, 39(9):743–781.
Dijkema MBA, van Strien RT, van der Zee SC, Mallant SF, Fischer P, Hoek G, Brunekreef B, Gehring U: Spatial variation in nitrogen dioxide concentrations and cardiopulmonary hospital admissions. Environ Res 2016, 151:721–727.
Hou D, Ge Y, Chen C, Tan Q, Chen R, Yang Y, Li L, Wang J, Ye M, Li C et al: Associations of long-term exposure to ambient fine particulate matter and nitrogen dioxide with lung function: A cross-sectional study in China. Environ Int 2020, 144:105977.
Jiang Y, Niu Y, Xia Y, Liu C, Lin Z, Wang W, Ge Y, Lei X, Wang C, Cai J et al: Effects of personal nitrogen dioxide exposure on airway inflammation and lung function. Environ Res 2019, 177:108620.
Huang YC, Rappold AG, Graff DW, Ghio AJ, Devlin RB: Synergistic effects of exposure to concentrated ambient fine pollution particles and nitrogen dioxide in humans. Inhal Toxicol 2012, 24(12):790–797.
Frampton MW, Morrow PE, Cox C, Gibb FR, Speers DM, Utell MJ: Effects of nitrogen dioxide exposure on pulmonary function and airway reactivity in normal humans. Am Rev Respir Dis 1991, 143(3):522–527.
Melo T, Montero-Bullon JF, Domingues P, Domingues MR: Discovery of bioactive nitrated lipids and nitro-lipid-protein adducts using mass spectrometry-based approaches. Redox Biol 2019, 23:101106.
Freeman BA, Baker PR, Schopfer FJ, Woodcock SR, Napolitano A, d’Ischia M: Nitro-fatty acid formation and signaling. J Biol Chem 2008, 283(23):15515–15519.
Lima ES, Bonini MG, Augusto O, Barbeiro HV, Souza HP, Abdalla DS: Nitrated lipids decompose to nitric oxide and lipid radicals and cause vasorelaxation. Free Radic Biol Med 2005, 39(4):532–539.
Ricciardolo FL: Multiple roles of nitric oxide in the airways. Thorax 2003, 58(2):175–182.
Raitakari OT, Celermajer DS: Flow-mediated dilatation. Br J Clin Pharmacol 2000, 50(5):397–404.
Kowalczyk A, Kleniewska P, Kolodziejczyk M, Skibska B, Goraca A: The role of endothelin-1 and endothelin receptor antagonists in inflammatory response and sepsis. Arch Immunol Ther Exp (Warsz) 2015, 63(1):41–52.
Bourque SL, Davidge ST, Adams MA: The interaction between endothelin-1 and nitric oxide in the vasculature: new perspectives. Am J Physiol Regul Integr Comp Physiol 2011, 300(6):R1288-1295.
Langrish JP, Lundback M, Barath S, Soderberg S, Mills NL, Newby DE, Sandstrom T, Blomberg A: Exposure to nitrogen dioxide is not associated with vascular dysfunction in man. Inhal Toxicol 2010, 22(3):192–198.
Kobayashi T, Kubota K: The reaction of nitrogen dioxide with lung surface components: The reaction with cholesterol. Chemosphere 1980, 9(12):777–784.
Chapin JC, Hajjar KA: Fibrinolysis and the control of blood coagulation. Blood Rev 2015, 29(1):17–24.
Shaffer F, Ginsberg JP: An Overview of Heart Rate Variability Metrics and Norms. Front Public Health 2017, 5:258.
Felber Dietrich D, Gemperli A, Gaspoz JM, Schindler C, Liu LJ, Gold DR, Schwartz J, Rochat T, Barthelemy JC, Pons M et al: Differences in heart rate variability associated with long-term exposure to NO2. Environ Health Perspect 2008, 116(10):1357–1361.
Acknowledgements
The authors would like to acknowledge Drs. Steven Prince and Phillip Bromberg for their critical review and valuable suggestions. We thank Tracey Montilla, Julie Wood, Martin Case, Lisa Dailey, Joleen Soukup, and Shirley Harder for their excellent technical support. We thank the recruitment service from MPF Federal. This project was supported in part by an appointment to the Research Participation Program at the U.S. Environmental Protection Agency administered by the Oak Ridge Institute for Science and Education through an interagency agreement between the U.S. Department of Energy and EPA.
Disclaimer
The research described in this article has been reviewed by the Center for Environmental Public Health and Environmental Assessment, EPA and approved for publication. The contents of this article should not be construed to represent agency policy, nor does mention of trade names or commercial products constitute endorsement or recommendation for use.
Funding
This work was supported by the U.S. Environmental Protection Agency Intramural Research Program.
Author information
Authors and Affiliations
Contributions
HC, SZ, and HT had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis, including and especially any adverse effects. HC and SZ drafted the manuscript; All authors have substantial contributions to the conception or the design of the work. All authors contributed to the acquisition analysis and interpretation of data; revising critically and final approval of the version; and agreement to be accountable for all aspects of the work.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of the University of North Carolina at Chapel Hill and the U.S. Environment Protection Agency. Informed consent was obtained from each participant prior to the enrollment of the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Additional Figure 1 and Table 1-10.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chen, H., Zhang, S., Shen, W. et al. The influence of dietary intake of omega-3 polyunsaturated fatty acids on the association between short-term exposure to ambient nitrogen dioxide and respiratory and cardiovascular outcomes among healthy adults. Environ Health 20, 123 (2021). https://doi.org/10.1186/s12940-021-00809-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12940-021-00809-9