Abstract
Background
Cardiovascular disease is the major cause of morbidity and mortality, particularly in type 2 diabetes mellitus (T2DM). Novel markers of insulin resistance and progression of atherosclerosis include the triglycerides and glucose index (TyG index), the triglycerides and body mass index (Tyg-BMI) and the metabolic score for insulin resistance (METS-IR). Establishing independent risk factors for in-hospital death and major adverse cardiac and cerebrovascular events (MACCE) in patients with myocardial infarction (MI) remains critical. The aim of the study was to assess the risk of in-hospital death and MACCE within 12 months after ST-segment elevation myocardial infarction (STEMI) and non-ST-segment elevation myocardial infarction (NSTEMI) in patients with and without T2DM based on TyG index, Tyg-BMI and METS-IR.
Methods
Retrospective analysis included 1706 patients with STEMI and NSTEMI hospitalized between 2013 and 2021. We analyzed prognostic value of TyG index, Tyg-BMI and METS-IR for in-hospital death and MACCE as its components (death from any cause, MI, stroke, revascularization) within 12 months after STEMI or NSTEMI in patients with and without T2DM.
Results
Of 1706 patients, 58 in-hospital deaths were reported (29 patients [4.3%] in the group with T2DM and 29 patients [2.8%] in the group without T2DM; p = 0.1). MACCE occurred in 18.9% of the total study population (25.8% in the group with T2DM and 14.4% in the group without T2DM; p < 0.001). TyG index, Tyg-BMI and METS-IR were significantly higher in the group of patients with T2DM compared to those without T2DM (p < 0.001). Long-term MACCE were more prevalent in patients with T2DM (p < 0.001). The area under the ROC curve (AUC-ROC) for the prediction of in-hospital death and the TyG index was 0.69 (p < 0.001). The ROC curve for predicting in-hospital death based on METS-IR was 0.682 (p < 0.001). The AUC-ROC values for MACCE prediction based on the TyG index and METS-IR were 0.582 (p < 0.001) and 0.57 (p < 0.001), respectively.
Conclusions
TyG index was an independent risk factor for in-hospital death in patients with STEMI or NSTEMI. TyG index, TyG-BMI and METS-IR were not independent risk factors for MACCE at 12 month follow-up. TyG index and METS-IR have low predictive value in predicting MACCE within 12 months after STEMI and NSTEMI.
Similar content being viewed by others
Introduction
Cardiovascular complications are a major cause of morbidity and mortality, particularly in type 2 diabetes mellitus (T2DM) [1]. Myocardial infarction (MI), results from myocardial ischemia due to a disproportion between myocardial oxygen supply and demand [2]. Atherosclerosis is the most common cause of MI. Risk factors for coronary artery atherosclerosis and its progression have been identified, which allowed the implementation of preventive and therapeutic measures to reduce its prevalence and improve prognosis [3]. Major adverse cardiovascular and cerebrovascular events (MACCE) are still the cause of frequent hospitalizations and death, particularly in developing countries [4]. Patients with T2DM are at high or even very high risk of cardiovascular disease (CVD). The occurrence of further cardiovascular incidents in this group of patients is much more common than in the general population [5]. Therefore, improvement in risk assessment of in-hospital death and MACCE defined as death from any cause, MI, stroke and repeat revascularization during long-term follow-up for the general population and T2DM population has significant implications in managing patients with MI.
Many studies have confirmed the impact of insulin resistance and lipid and glucose metabolism dysregulation on the progression of coronary artery disease (CAD). Studies have demonstrated that insulin resistance, which is the main pathogenetic mechanism in the development of T2DM, is a factor influencing the progression of macrovascular complications in this group of patients and a factor in the development of CVD in patients without T2DM [3, 6,7,8]. Many methods have been developed to estimate insulin resistance. The most commonly used being the Homeostasis Model Insulin-Resistance Assessment (HOMA-IR). The distribution of HOMA-IR varies according to demographic characteristics of patients, such as age, gender and race, which makes it difficult to estimate the optimal cut-off point [9].
Therefore, the search continues for simpler and reliable indicators that could estimate insulin resistance and the associated progression of atherosclerosis without using insulin assays. TyG index (triglycerides and glucose index), Tyg-BMI (triglycerides and body mass index) and METS-IR (metabolic score for insulin resistance), are indices that incorporate basic laboratory parameters, such as fasting serum glucose, triglycerides, HDL-cholesterol, and anthropometric measurements, including weight and height [3, 6]. These formulas seem to be reliable indices of insulin resistance and independent predictors of atherosclerosis progression in the general population and T2DM patients [3, 6, 7]. Estimating reliable indicators of in-hospital death and MACCE in patients after acute coronary syndrome (ACS) remains a critical issue.
We set out to investigate prognostic values of TyG index, Tyg-BMI and METS-IR for the occurrence of in-hospital death and MACCE within 12 months after ST-segment elevation myocardial infarction (STEMI) or non-ST-segment elevation myocardial infarction (NSTEMI).
Materials and methods
The study conforms to the Declaration of Helsinki. Informed consent for data analysis was obtained from the patients according to the Polish law on patients rights regarding data registration. Approval for analyzing recorded data was waived by the local bioethics committee on human research given the retrospective nature of the study.
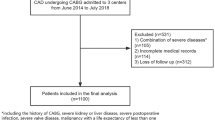
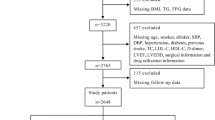
This retrospective analysis included 1706 patients hospitalized for STEMI and NSTEMI between 2013 and 2021. Detailed anthropometric data were routinely collected from patients during hospitalization. Additionally, biochemical tests and percutaneous coronary intervention (PCI) were performed.
The study population was divided into two groups:
-
Group 1—patients with T2DM (n = 680)
-
Group 2- patients without T2DM (n = 1026).
The inclusion criterion was STEMI or NSTEMI in patients who underwent coronary angiography. STEMI was diagnosed when clinical symptoms of myocardial ischemia were accompanied by an increase in cardiac troponin levels (myocardial necrosis marker) at least one value above the 99th percentile upper reference limit with ST-segment changes in the electrocardiogram (ECG) (i.e., ST-segment elevation at the J point in V2 and V3 leads of ≥ 2 mm in men aged ≥ 40 years and of ≥ 2.5 mm in men < 40 years of age and of ≥ 1.5 mm in women and/or ST-segment elevation of ≥ 1 mm in ≥ 2 contiguous electrocardiographic leads or the presence of a new left bundle branch block [10].
In turn, NSTEMI was diagnosed when clinical symptoms of myocardial ischemia were accompanied by an increase in cardiac troponin levels with at least one value above the 99th percentile upper reference limit without persistent ST-segment elevation on ECG and the presence of ST-segment depression of ≥ 0.5 mm or the presence of a negative T-wave or reversal of previously negative T-waves to positive [2, 11].
The exclusion criteria were eligibility for coronary artery bypass grafting (CABG) after coronary angiography, patients with type 1 diabetes mellitus and diabetes mellitus of other etiologies.
Clinical, laboratory, echocardiographic, and angiographic parameters were collected from 1,706 patients on admission. On day the second of hospitalization, venous fasting blood samples were routinely collected and analyzed for total blood count (TBC), total cholesterol, LDL cholesterol (LDL-C), HDL cholesterol (HDL-C), triglycerides (TG) and glucose (fasting plasma glucose; FPG).
Coronary angiography and PCI were performed according to the standard guidelines. During coronary angiography, infarct-related coronary artery was identified and hemodynamically significant atherosclerotic lesions in other coronary arteries were assessed. Atherosclerotic lesions narrowing the coronary artery lumen by at least 70% were considered hemodynamically significant.
Based on the results of laboratory tests and anthropometric measurements, the following indices were calculated:
-
TyG index = ln [TG (mg/dl) x FPG (mg/dl)/2] [12]
-
TyG-BMI = TyG index x BMI (kg/m2) [13]
-
METS-IR = {ln [2 x FPG (mg/dl) + TG (mg/dl)] x BMI (kg/m2)}/ln [HDL-C (mg/dl)] [14]
We analyzed the prevalence of in-hospital death and MACCE (death from any cause, MI, stroke, revascularization) during the 12 months after STEMI and NSTEMI.
Statistical analysis
Statistical analysis was performed using the STATISTICA 13.0 PL software (Tibco Software Inc, Palo Albo, CA, USA). Statistical significance was set at a p-value below 0.05. No data imputation was performed.
All tests were two-tailed. Nominal and ordinal data were expressed as percentages, while interval data as mean values ± standard deviation (SD). The distribution of variables was evaluated by the Shapiro–Wilk test. For comparison of data, the Student’s t test was used. Categorical variables were compared using χ2 test with correction for Yates’ continuity.
The influence of the factors on the prevalence of complications and death (in-hospital and long-term follow-up) was examined using logistic regression with the calculation of odds ratios (ORs). The cut-off values for TyG index, TyG-BMI, and METS-IR predicting in-hospital mortality and MACCE were determined using ROC curve analyses with the calculation of sensitivity and specificity for these values.
Results
The study evaluated 1706 patients with STEMI and NSTEMI, including 680 with T2DM (39.8%) and 1026 without T2DM (60.2%). Coronary angiography was performed in all patients. In this group, a detailed description of the procedure was recorded in 1299 patients. In the remaining patients, PCI was performed but the data are missing. In the group of 1299 patients, 1293 patients underwent PCI. No significant atherosclerotic lesions that required coronary stent implantation were found in the remaining six patients. In 1706 patients, TyG index, Tyg-BMI and METS-IR indexes were assessed. The presence of MACCE was assessed within 12 months after acute coronary syndrome (ACS).
Baseline clinical characteristics group are given in Table 1. Patients with T2DM presented with more comorbidities and previously diagnosed CAD was more prevalent. The mean duration of T2DM was 8 ± 4 years.
Table 2 shows laboratory characteristics used to assess the indices (TyG index, Tyg-BMI and METS-IR). Patients with T2DM had worse results of most laboratory tests, except for total cholesterol and LDL-cholesterol, which were lower in this group of patients.
Angiographic characteristics are presented in Table 3. Patients with T2DM had a higher prevalence of multivessel coronary artery disease (MVD) compared to those without T2DM. However, left anterior descending artery (LAD) was less frequently the infarct-related artery. Given the problems in identifying culprit vessels in NSTEMI patients, caution should be exercised when interpreting the data.
Table 4 shows the data on insulin resistance surrogates (TyG index, Tyg-BMI, METS-IR). Patients with T2DM had higher surrogate indices of insulin resistance (p < 0.001). Table 5 shows in-hospital and long-term prognosis. The rate in-hospital death was similar in the two groups. MACCE was more prevalent in patients with T2DM during 12 month follow-up (p < 0.001). Independent predictors of in-hospital death are presented in Table 6 and include age, female sex, decreased left ventricular ejection fraction, prior stroke, elevated TyG index, elevated creatinine levels and white blood count (WBC) and multivessel CAD.
Fasting glucose concentration and the glucose concentration on admission are not independent factors of in-hospital deaths. Independent predictors of MACCE during 12-month follow-up are given Table 7—these include age, decreased left ventricular ejection fraction, prior CAD, FPG, WBC, and cholesterol-LDL.
Figure 1 shows ROC analysis of the TyG index in predicting in-hospital death [AUC 0.69 (95% CI 0.62–0.76); p < 0.001 for the cut-off point 9.36 (sensitivity = 0.6, specificity = 0.71)]. There was no prognostic value of TyG-BMI in predicting in-hospital death (Fig. 2)
Figure 3 shows prognostic value of METS-IR in predicting in-hospital death [AUC 0.68 (95% CI 0.61–0.75); p < 0.001 for the cut-off point 2.46 (sensitivity = 0.71, specificity = 0.6)]. Figure 4 shows prognostic value of the TyG index in predicting MACCE [AUC 0.58 (95% CI 0.55–0.62); p < 0.001 for the cut-off point 8.78 (sensitivity = 0.7, specificity = 0.41)]. There was no predictive value of TyG-BMI for MACCE (Figs. 5). Figure 6 shows prognostic value of METS-IR in predicting MACCE [AUC 0.57 (95% CI 0.53–0.61); p < 0.001 for the cut-off point 2.47 (sensitivity = 0.52, specificity = 0.72)].
Discussion
Our study is the first to use all three indices (TyG index, TyG-BMI and METS-IR) to estimate the risk of in-hospital death and long-term MACCE in patients with and without T2DM after STEMI or NSTEMI. This single-center retrospective study showed that an increase in the TyG index was an independent risk factor for in-hospital death in patients with STEMI and NSTEMI. None of the three indices were an independent risk factor for MACCE during 12 month follow-up. TyG index and METS-IR indices had low predictive value in predicting the occurrence of MACCE within 12 months after STEMI and NSTEMI. TyG-BMI had no predicting value for in-hospital death or MACCE.
Analyzing the groups of patients with and without T2DM, we showed that patients with MI and T2DM had a significantly worse prognosis due to a higher prevalence of MACCE and its components including death, MI, or repeat revascularization, which is in line with most studies [15,16,17,18]. The three indices (TyG index, TyG-BMI, METS-IR) were used as surrogates for insulin resistance, which can be an indirect indicator of the metabolic syndrome. The TyG index was shown to predict metabolic syndrome better than the HOMA-IR [19]. Chenge et al. showed that TyG-BMI and METS-IR were independent risk factors for hypertension, had a good predictive value for the prevalence of hypertension, and TyG-BMI was superior to METS-IR in this respect [20]. In their study on patients with T2DM, Han et al. showed a positive correlation between TyG index, TyG-BMI, METS-IR and TG/HDL-cholesterol and hyperuricemia. Of the four surrogates of insulin resistance, TG/HDL-c was the best marker for identifying hyperuricemia in patients with T2DM [21]. It is known that insulin resistance influences not only metabolic disorders, such as dyslipidemia, obesity, and disorders of carbohydrate metabolism but also atherosclerosis and the progression of CVD [22]. Therefore, we attempted to use surrogate markers of insulin resistance that are easy to calculate for prognostic purposes for in-hospital death and MACCE in patients after STEMI or NSTEMI.
Our results are in agreement with those of Gou et al. who showed that the TyG index and TG/HDL-Cholesterol were significant predictors of in-hospital mortality in non-diabetic acute MI patients [23]. In our study, multivariate logistic regression showed that TyG index was an independent risk factor for in-hospital death in patients with STEMI and NSTEMI. Per one unit increment in the TyG index, the risk of in-hospital death increased 2.5-fold. In-hospital death was also assessed by Liao et al. in a group of patients hospitalized in an intensive care unit (ICU). Patients were hospitalized for various conditions (not only due to MI). Liao et al. showed that the TyG index was strongly associated with increased mortality from any cause in patients in the ICU. Therefore, it may be useful for identifying critically ill patients at high risk of death [24]. Another study found that a higher TyG index was associated with a higher risk of in-hospital mortality in patients with ischemic stroke [25]. It seems that the TyG index is a good predictor of in-hospital death not only in the group of post-myocardial infarction patients (as we showed) but also in those with severe general condition due to other diseases.
The TyG index was also assessed as a predictor of MACCE in a group of 1,092 STEMI patients who underwent PCI. The prevalence of MACCE and mortality from any cause at 30 days, 6 months and 1 year after PCI was higher in STEMI patients with TyG index levels in the highest quartile. The area under the curve (AUC) of the TyG index predicting the occurrence of MACCE in STEMI patients after PCI was 0.685 (95% CI 0.610–0.761; p = 0.001) [26]. In our study, TyG index prognostic value for MACCE was 0.582 (95% CI 0.546–0.619; p < 0.001). Although the results were comparable, the predictive value was low for using these indices for prognostic purposes.
METS-IR was evaluated in patients with ischemic cardiomyopathy (ICM) and T2DM. The index was predictive of the occurrence of MACE, regardless of known cardiovascular risk factors. These results suggest that METS-IR may be a useful marker for MACE risk stratification in patients with ICM and T2DM [27]. Our results pertaining to METS-IR are similar to those obtained by Drwiła-Stec et al. In their study, MACE and all-cause mortality at 1-year follow-up occurred in 7.9% of patients in the STEMI group and 10.9% in the NSTEMI group. Neither of the indexes (METS-IR and TyG-BMI) was a predictor of MACE in the STEMI or NSTEMI groups [28]. It seems that currently METS-IR cannot be considered a good predictor of MACCE after MI.
We demonstrated that METS-IR could potentially be used as a prognostic factor for in-hospital death. However, the sensitivity (70%) and specificity (60%) were insufficient and the predictive value was low. Therefore, further studies are warranted to consider the METS-IR index an important predictor of in-hospital death.
We are the first to assess TyG-BMI for predicting in-hospital death and MACCE. We showed that TyG-BMI was not suitable for the predicting in-hospital death or long-term MACCE. Studies confirmed that TyG-BMI is significantly associated with the severity of CAD and is an independent risk factor for multivessel CAD [3]. Zhang et al. found that TyG index, TyG-BMI, TG/HDL-Cholesterol and METS-IR could be valuable predictors of CAD severity. Of the four indices above, METS-IR had the highest predictive value for CAD severity, followed by TyG-BMI [3]. Apart from our study, Cheng et al. also evaluated TyG-BMI as a predictor of MACCE in patients undergoing PCI [29]. Higher TyG-BMI was proportional to the increased prevalence of MACCE in female and elderly patients. However, including TyG-BMI did not improve risk prediction over traditional risk factors in elderly or female patients [29].
Although the above-mentioned indices have been effective in estimating insulin resistance, some of them do not seem to have prognostic significance for in-hospital death and long-term MACCE. Only the TyG index was identified as an independent risk factor for in-hospital death in patients with STEMI and NSTEMI. Confirmation of this finding in subsequent clinical studies may lead to the integration of TyG index assessment upon hospital admission and the adoption of therapeutic approaches different from those used thus far (potentially SGLT-2 inhibitors or GLP-1 receptor agonists or amylin hold promise in patient with ACS) [30,31,32]. Considering the use of cardioprotective drugs, such as SGLT-2 inhibitors or GLP-1 receptor agonists, in patients with and without diabetes, it is valuable to evaluate their impact on the TyG index and potential benefits in reducing in-hospital mortality and MACCE after STEMI and NSTEMI [30, 31]. Given the study period we were unable to analyze the effects of SGLT-2 inhibitors or GLP-1 receptor agonists in our population.
The main strength of this study includes a large sample size. The study is the first to use all three novel markers of insulin resistance and progression of atherosclerosis (TyG index, TyG-BMI and METS-IR) at once to estimate prognosis after AMI. Nevertheless, this study should be viewed in light of its limitations. First, this is single-center, retrospective and an observational study, thus the results could indicate association but not causation. Therefore, the results of our study should be confirmed in a multicenter, prospective study. In addition, the study was conducted between 2013 and 2021, during which SGLT-2 inhibitors or GLP-1 receptor agonists were not reimbursed and rarely used. These drugs potentially might have influenced the results of prognostic value of the novel biomarkers.
Conclusions
In conclusion, of the insulin resistance surrogates evaluated in the study, only TyG index was an independent risk factor for in-hospital death in patients with STEMI or NSTEMI. None of the insulin resistance surrogates were an independent risk factor for MACCE during the 12-month follow-up. TyG index and METS-IR have a low predictive value for predicting MACCE within 12 months after STEMI or NSTEMI.
References
Viigimaa M, Sachinidis A, Toumpourleka M, Koutsampasopoulos K, Alliksoo S, Titma T. Macrovascular complications of type 2 diabetes mellitus. Curr Vasc Pharmacol. 2020;18(2):110–6. https://doi.org/10.2174/1570161117666190405165151.
Pollack CV, Amin A, Wang T, Deitelzweig S, Cohen M, Slattery D, Fanikos J, DiLascia C, Tuder R, Kaatz S. Contemporary NSTEMI management: the role of the hospitalist. Hosp Pract. 2020;48(1):1–11. https://doi.org/10.1080/21548331.2020.1701329.
Zhang Y, Wang R, Fu X, Song H. Non-insulin-based insulin resistance indexes in predicting severity for coronary artery disease. Diabetol Metab Syndr. 2022;14(1):191. https://doi.org/10.1186/s13098-022-00967-x.
Hawranek M, Gąsior M, Nożyński J, Poloński L. Causes of mortality in patients with myocardial infarction in the reperfusion. Folia Cardiol. 2004;11(4):239–45.
Strain WD, Paldánius PM. Diabetes, cardiovascular disease and the microcirculation. Cardiovasc Diabetol. 2018;17(1):57. https://doi.org/10.1186/s12933-018-0703-2.
Park K, Ahn CW, Lee SB, Kang S, Nam JS, Lee BK, Kim JH, Park JS. Elevated TyG index predicts progression of coronary artery calcification. Diabetes Care. 2019;42(8):1569–73. https://doi.org/10.2337/dc18-1920.
Zhang Y, Liu C, Xu Y, Wang Y, Dai F, Hu H, Jiang T, Lu Y, Zhang Q. The management correlation between metabolic index, cardiovascular health, and diabetes combined with cardiovascular disease. Front Endocrinol. 2023;27(13):1036146. https://doi.org/10.3389/fendo.2022.1036146.
Gazzaruso C, Solerte SB, De Amici E, Mancini M, Pujia A, Fratino P, Giustina A, Garzaniti A. Association of the metabolic syndrome and insulin resistance with silent myocardial ischemia in patients with type 2 diabetes mellitus. Am J Cardiol. 2006;97(2):236–9. https://doi.org/10.1016/j.amjcard.2005.07.133.
Tahapary DL, Pratisthita LB, Fitri NA, Marcella C, Wafa S, Kurniawan F, Rizka A, Tarigan TJE, Harbuwono DS, Purnamasari D, Soewondo P. Challenges in the diagnosis of insulin resistance: focusing on the role of HOMA-IR and Tryglyceride/glucose index. Diabetes Metab Syndr. 2022;16(8):102581. https://doi.org/10.1016/j.dsx.2022.102581.
Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli-Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, Hindricks G, Kastrati A, Lenzen MJ, Prescott E, Roffi M, Valgimigli M, Varenhorst C, Vranckx P, Widimský P. ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology. Eur Heart J. 2017;39(2):119–77. https://doi.org/10.1093/eurheartj/ehx393.
Roffi M, Patrono C, Collet JP, Mueller C, Valgimigli M, Andreotti F, Bax JJ, Borger MA, Brotons C, Chew DP, Gencer B, Hasenfuss G, Kjeldsen K, Lancellotti P, Landmesser U, Mehilli J, Mukherjee D, Storey RF. ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation: task force for the management of acute coronary syndromes in patients presenting without persistent ST-segment elevation of the European society of cardiology. Eur Heart J. 2016;37(3):267–315. https://doi.org/10.1093/eurheartj/ehv320.
Simental-Mendía LE, Rodríguez-Morán M, Guerrero-Romero F. The product of fasting glucose and triglycerides as surrogate for identifying insulin resistance in apparently healthy subjects. Metab Syndr Relat Disord. 2008;6(4):299–304. https://doi.org/10.1089/met.2008.0034.
Er LK, Wu S, Chou HH, Hsu LA, Teng MS, Sun YC, Ko YL. Triglyceride glucose-body mass index is a simple and clinically useful surrogate marker for insulin resistance in nondiabetic individuals. PLoS ONE. 2016;11(3): e0149731. https://doi.org/10.1371/journal.pone.0149731.
Bello-Chavolla OY, Almeda-Valdes P, Gomez-Velasco D, Viveros-Ruiz T, Cruz-Bautista I, Romo-Romo A, Sánchez-Lázaro D, Meza-Oviedo D, Vargas-Vázquez A, Campos OA, Sevilla-González MDR, Martagón AJ, Hernández LM, Mehta R, Caballeros-Barragán CR, Aguilar-Salinas CA. METS-IR, a novel score to evaluate insulin sensitivity, is predictive of visceral adiposity and incident type 2 diabetes. Eur J Endocrinol. 2018;178(5):533–44. https://doi.org/10.1530/EJE-17-0883.
Cosentino N, Bonomi A, Campodonico J, Veglia F, De Ferrari GM, Genovese S, Marenzi G. Can the in-hospital mortality gap between STEMI patients with and without diabetes mellitus be reduced? The cardio-renal hypothesis. Nutr Metab Cardiovasc Dis. 2021;31(5):1516–20. https://doi.org/10.1016/j.numecd.2021.02.003.
Karayiannides S, Norhammar A, Frøbert O, James SK, Lagerqvist B, Lundman P. Prognosis in patients with diabetes mellitus and STEMI undergoing primary PCI. J Am Coll Cardiol. 2018;72(12):1427–8. https://doi.org/10.1016/j.jacc.2018.06.061.
Baviera M, Genovese S, Colacioppo P, Cosentino N, Foresta A, Tettamanti M, Fortino I, Roncaglioni MC, Marenzi G. Diabetes mellitus duration and mortality in patients hospitalized with acute myocardial infarction. Cardiovasc Diabetol. 2022;21(1):223. https://doi.org/10.1186/s12933-022-01655-w.PMID:36309742;PMCID:PMC9618227.
Foraker RE, Guha A, Chang H, O’Brien EC, Bower JK, Crouser ED, Rosamond WD, Raman SV. Survival after MI in a community cohort study: contribution of comorbidities in NSTEMI. Glob Heart. 2018;13(1):13–8. https://doi.org/10.1016/j.gheart.2018.01.002.
Mirr M, Skrypnik D, Bogdański P, Owecki M. Newly proposed insulin resistance indexes called TyG-NC and TyG-NHtR show efficacy in diagnosing the metabolic syndrome. J Endocrinol Invest. 2021;44(12):2831–43. https://doi.org/10.1007/s40618-021-01608-2.
Cheng W, Kong F, Chen S. Comparison of the predictive value of four insulin resistance surrogates for the prevalence of hypertension: a population-based study. Diabetol Metab Syndr. 2022;14(1):137. https://doi.org/10.1186/s13098-022-00907-9.PMID:36163185;PMCID:PMC9511744.
Han R, Zhang Y, Jiang X. Relationship between four non-insulin-based indexes of insulin resistance and serum uric acid in patients with type 2 diabetes: a cross-sectional study. Diabetes Metab Syndr Obes. 2022;9(15):1461–71. https://doi.org/10.2147/DMSO.S362248.
Hill MA, Yang Y, Zhang L, Sun Z, Jia G, Parrish AR, Sowers JR. Insulin resistance, cardiovascular stifening and cardiovascular disease. Metabolism. 2021;119: 154766.
Guo J, Ji Z, Carvalho A, Qian L, Ji J, Jiang Y, Liu G, Ma G, Yao Y. The triglycerides-glucose index and the triglycerides to high-density lipoprotein cholesterol ratio are both effective predictors of in-hospital death in non-diabetic patients with AMI. PeerJ. 2022;21(10): e14346. https://doi.org/10.7717/peerj.14346.
Liao Y, Zhang R, Shi S, Zhao Y, He Y, Liao L, Lin X, Guo Q, Wang Y, Chen L, Li W, Li S, Chen K, Fang Y. Triglyceride-glucose index linked to all-cause mortality in critically ill patients: a cohort of 3026 patients. Cardiovasc Diabetol. 2022;21(1):128. https://doi.org/10.1186/s12933-022-01563-z.
Miao M, Bi Y, Hao L, Bao A, Sun Y, Du H, Song L, You S, Zhong C. Triglyceride-glucose index and short-term functional outcome and in-hospital mortality in patients with ischemic stroke. Nutr Metab Cardiovasc Dis. 2023;33(2):399–407. https://doi.org/10.1016/j.numecd.2022.11.004.
Luo E, Wang D, Yan G, Qiao Y, Liu B, Hou J, Tang C. High triglyceride-glucose index is associated with poor prognosis in patients with acute ST-elevation myocardial infarction after percutaneous coronary intervention. Cardiovasc Diabetol. 2019;18(1):150. https://doi.org/10.1186/s12933-019-0957-3.
Zhang X, Liu F, Li W, Zhang J, Zhang T, Yu X, Luo J, Zhao Q, Zhang J, Fang B, Yang Y, Li X. Metabolic score for insulin resistance (METS-IR) predicts adverse cardiovascular events in patients with type 2 diabetes and ischemic cardiomyopathy. Diabetes Metab Syndr Obes. 2023;5(16):1283–95. https://doi.org/10.2147/DMSO.S404878.PMID:37179787;PMCID:PMC10167964.
Drwiła-Stec D, Rostoff P, Gajos G, Nessler J, Konduracka E. Predictive value of metabolic score for insulin resistance and triglyceride glucose-BMI among patients with acute myocardial infarction in 1-year follow-up. Coron Artery Dis. 2023. https://doi.org/10.1097/MCA.0000000000001242.
Cheng Y, Fang Z, Zhang X, Wen Y, Lu J, He S, Xu B. Association between triglyceride glucose-body mass index and cardiovascular outcomes in patients undergoing percutaneous coronary intervention: a retrospective study. Cardiovasc Diabetol. 2023;22(1):75. https://doi.org/10.1186/s12933-023-01794-8.PMID:36997935;PMCID:PMC10064664.
Lopaschuk GD, Verma S. Mechanisms of cardiovascular benefits of sodium glucose co-transporter 2 (SGLT2) inhibitors: a state-of-the-art review. JACC Basic Transl Sci. 2020;5(6):632–44. https://doi.org/10.1016/j.jacbts.2020.02.004.PMID:32613148;PMCID:PMC7315190.
Andrikou E, Tsioufis C, Andrikou I, Leontsinis I, Tousoulis D, Papanas N. GLP-1 receptor agonists and cardiovascular outcome trials: an update. Hellenic J Cardiol. 2019;60(6):347–51. https://doi.org/10.1016/j.hjc.2018.11.008.
Grover A, Sharma K, Gautam S, Gautam S, Gulati M, Singh SK. Diabetes and its complications: therapies. Anticipated Aspired Curr Diabetes Rev. 2021;17(4):397–420. https://doi.org/10.2174/1573399816666201103144231.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conceptualization: D.R., B.H. and K.S.; Data curation: D.R., M.W., T.S., D.S., A.N.W., S.R. Formal analysis: D.R., B.H., M.G., T.S.; Investigation: A.N.W., B.H.; Methodology: D.R., M.W., B.H., M.G., T.S.; Project administration, D.R., M.W.; Prepared figures: S.R., D.S., T.S.; Supervision: B.H., M.G. and K.S.; Writing – original draft: D.R.; Writing – review & editing, B.H, M.W., M.G., K.S., D.S.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study conforms to the Declaration of Helsinki. Informed consent for data analysis was obtained from the patients according to the Polish law on patients rights regarding data registration. Approval for analyzing recorded data was waived by the local bioethics committee on human research given the retrospective nature of the study.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Rokicka, D., Hudzik, B., Wróbel, M. et al. The prognostic impact of insulin resistance surrogates in patients with acute myocardial infarction with and without type 2 diabetes. Cardiovasc Diabetol 23, 147 (2024). https://doi.org/10.1186/s12933-024-02240-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-024-02240-z