Abstract
Background
The PI*S variant is one of the most prevalent mutations within alpha-1 antitrypsin deficiency (AATD). The risk of developing AATD-related lung disease in individuals with the PI*SS genotype is poorly defined despite its substantial prevalence. Our study aimed to characterize this genotype and its risk for lung disease and compare it with the PI*ZZ and PI*SZ genotypes using data from the European Alpha-1 antitrypsin Deficiency Research Collaboration international registry.
Method
Demographic, clinical, functional, and quality of life (QoL) parameters were assessed to compare the PI*SS characteristics with the PI*SZ and PI*ZZ controls. A propensity score with 1:3 nearest-neighbour matching was performed for the most important confounding variables.
Results
The study included 1007 individuals, with PI*SS (n = 56; 5.6%), PI*ZZ (n = 578; 57.4%) and PI*SZ (n = 373; 37.0%). The PI*SS population consisted of 58.9% men, with a mean age of 59.2 years and a mean FEV1(% predicted) of 83.4%. Compared to PI*ZZ individuals they had less frequent lung disease (71.4% vs. 82.2%, p = 0.037), COPD (41.4% vs. 60%, p = 0.002), and emphysema (23.2% vs. 51.9%, p < 0.001) and better preserved lung function, fewer exacerbations, lower level of dyspnoea, and better QoL. In contrast, no significant differences were found in the prevalence of lung diseases between PI*SS and PI*SZ, or lung function parameters, exacerbations, dyspnoea, or QoL.
Conclusions
We found that, as expected, the risk of lung disease associated with the PI*SS genotype is significantly lower compared with PI*ZZ, but does not differ from that observed in PI*SZ individuals, despite having higher serum AAT levels.
Trial registration
www.clinicaltrials.gov (ID: NCT04180319).
Similar content being viewed by others
Introduction
Alpha-1 antitrypsin deficiency (AATD) is one of the most common genetic disorders in adults and is characterized by reduced levels of circulating alpha-1 antitrypsin (AAT), attributed to mutations within the SERPINA1 gene [1]. More than 100 deficient variants have been described, being Proteinase inhibitor (PI)*S (Glu264Val) and PI*Z (Glu342Lys) the most prevalent [2]. The PI*S variant is correlated with a moderate deficiency of the protein, as it expresses 50–60% of AAT, while PI*Z is responsible for a severe deficiency, expressing 10–20% of the protein [3,4,5].
The most frequent clinical manifestation of AATD is pulmonary emphysema [1, 6]. The risk for developing AATD-related emphysema is well established for the PI*ZZ genotype, and an increased risk has been demonstrated for PI*SZ, particularly in smokers [7, 8]. However, it remains unclear for other genotypes, such as PI*SS. As the protein serum levels in PI*SS individuals are not below the considered protective threshold [5], the risk for pulmonary disease is believed to be low in this genotype [6]. Furthermore, PI*S is a non-polymerizing variant, with measurements of circulating polymer concentrations (with chemotactic pathogenic effects) being low in these patients [9]. However, the potential risk of lung disease associated with the PI*SS genotype may be of concern since the number of carriers of this genotype is substantial. De Serres, et al. [10]. estimated a total of 4,017,900 individuals worldwide with the PI*SS genotype, with the greatest prevalence being found in Central and Western Europe with 1,460,725 individuals, followed by 746,066 in South America and 625,651 in North Africa [10]. However, information on the burden of disease associated with the PI*SS genotype is scarce [11].
Our study aimed to characterize the PI*SS genotype and its risk for developing lung disease and compare it with the PI*ZZ and PI*SZ genotypes, using the European Alpha-1 antitrypsin Deficiency Research Collaboration (EARCO) international registry [12], which includes a large sample of individuals with the different deficient phenotypes recruited in countries in Europe and America [13].
Method
Study design
The EARCO registry is an international, observational, multicentre study including individuals with AATD, as detailed in the EARCO protocol [12] and registered at www.clinicaltrials.gov (ID: NCT04180319). Regarding personal data protection, the EARCO registry protocol is under the General Data Protection Regulation 2016/679 of the European Parliament and of the European Council of April 27, 2016. The EARCO database is securely hosted on the EARCO website (www.earco.org). The study protocol received central ethics approval by the Research Ethics Committee of the Vall d’Hebron University Hospital of Barcelona, Spain (PR(AG)480/2018) and was subsequently approved by all participating centres. All participants provided written informed consent and the study was conducted in accordance with the Declaration of Helsinki. The results of the baseline data of the EARCO study have recently been reported [13, 14].
The objective of the current study was to investigate the risk of lung disease associated with the PI*SS genotype by comparing the clinical characteristics and the severity of lung disease (namely, emphysema, COPD, chronic bronchitis, asthma and bronchiectasis) in subjects with the PI*SS genotype with those with the PI*SZ or PI*ZZ genotypes.
Population
This report analyses baseline data from patients included in EARCO from February 1st, 2020, to March 1st, 2023. Patients with the PI*SS genotype were designated as the study group, while those with the PI*SZ and PI*ZZ genotypes constituted the control groups. Patients with other genotypes, those currently under augmentation therapy (AT), and those with missing information related to the genotype or AT status were excluded from the analysis.
Measurements
We analysed the demographic data, proteinase inhibitor genotype, comorbidities, lung function, respiratory symptoms, presence of respiratory disease (including emphysema, COPD, chronic bronchitis, asthma and/or bronchiectasis) and their exacerbations. It is important to note that in the EARCO database, researchers are required to specify the type of lung disease if present, selecting from the following options: emphysema, COPD, chronic bronchitis, asthma, bronchiectasis, lung cancer or other. If “other” is chosen, researchers must provide additional details, ensuring that all types of lung disease are clearly identified and documented. We also assessed the quality of life measured by the modified medical research council (mMRC) scale, the chronic obstructive pulmonary disease (COPD) Assessment Test (CAT) specific questionnaire [15], the EuroQoL (EQ) index questionnaire [16], the EQ-Visual analogue scale (VAS), and physical activity measured by the mean time walked per day [17, 18], and the treatment administered. The severity of COPD was also measured by the body mass index, obstruction, dyspnoea and exacerbations (BODEx) index [19].
Statistical analysis
Qualitative variables were described with absolute frequencies and percentages. The description of quantitative variables was performed using the mean and standard deviation (SD). The Kolmogorov–Smirnov test was used to assess the normality of distributions.
First, unmatched patients with the PI*SS genotype were compared with PI*ZZ and PI*SZ individuals. In the case of quantitative variables, Mann-Whitney tests were carried out. The Chi-squared test (Fisher test for frequencies < 5) was used for the comparison of categorical variables.
A propensity score matching (PSM) method was used to compare the characteristics of PI*SS with the controls, accounting for confounding variables. A 1:3 nearest-neighbour matching was performed with age, sex, pack-years, and centre as confounders, without replacement. A calliper width of 0.5 was considered at matching. Proper adjustment was assessed with standardized mean differences (SMD) in the matched population, whilst covariate imbalance was defined with an SMD threshold > 0.2.
A generalized linear model was used to evaluate the odds of Carbon monoxide transfer coefficient (KCO)(%) and forced expiratory volume in one second (FEV1)(%) being below 80% in the PI*SS group compared to PI*ZZ and PI*SZ genotypes. Generalized estimating equations were used to estimate the parameters of the generalized linear models, considering a binomial distribution and accounting for the effect raised by the clustering of patients from the same centre. A multivariable analysis was also performed, adjusting for the number of total exacerbations in the last year, and the existence of previous pneumonia. In all cases, a p < 0.05 was considered statistically significant. The statistical software RStudio (V2.5.1) was used for the analysis.
Results
Study population
The EARCO registry included 1453 individuals at the time of the analysis. A total of 446 patients were excluded for one or more of the following reasons: absence of genotype information (n = 30), genotype ineligible for the study (n = 107); or patients under AT or missing AT status (n = 361). The study population included 1007 individuals, with PI*SS (n = 56; 5.6%), PI*ZZ (n = 578; 57.4%) and PI*SZ (n = 373; 37.0%).
Characteristics of the PI*SS population
Thirty-three (58.9%) participants were men, with a mean age of 59.2 (±13.9) years and a mean AAT level of 81 (±23.9) mg/dl. There was a predominance of former smokers (67.9%) with a mean consumption of 34.8 (±30.7) pack-years. Up to 71.4% had lung disease, COPD being the most frequent (41.1%), with a mean FEV1(%) of 83.4% (±29.9%). The mean mMRC and CAT scores were 1.69 (±0.9) and 6.5 (±7.1), respectively and the mean BODEx index was 1.22 (±1.8). The remaining characteristics are shown in Table 1.
Comparison between PI*SS and PI*ZZ. Unmatched and matched analysis
Patients in the PI*SS group were significantly older than those with PI*ZZ (59.2±13.9 vs. 54.0±14.4 years; p = 0.012), were less frequently never smokers (23.2% vs. 51.4%; p < 0.001) and had a higher smoking consumption (34.8±30.7 vs. 14.6±12.9 pack years; p < 0.001). However, PI*SS individuals less frequently had emphysema (23.2% vs. 42.8%; p = 0.005), were of an older age at symptom onset (49.6±19.4 vs. 43±15.7 years; p = 0.010) and had an older age at diagnosis of the deficiency (54.4±16.6 vs. 42.5±18 years; p < 0.001) (Table 1).
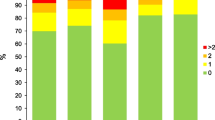
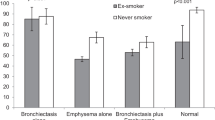
After matching, the characteristics of the PI*SS and PI*ZZ individuals were well balanced (Fig. 1). The matched analysis revealed similar results with a lower disease burden in individuals with PI*SS, with significant differences in lung disease (71.4% vs. 82.2%, p = 0.037), COPD (41.4% vs. 60%, p = 0.002) and emphysema (23.2% vs. 51.9%, p < 0.001) (Fig. 2). PI*SS individuals had an older age at diagnosis (54.4±16.6 vs. 44.6±16.7 years-old; p = 0.006). Lung function parameters were significantly better preserved in PI*SS subjects (Fig. 3), and they had less frequent exacerbations, a lower level of dyspnoea, a better BODEx index and better quality of life measured with the EQ-index, the VAS and CAT (Table 1).
Dot plot displaying standardized mean differences in baseline characteristics between ZZ and SS patients, before (N = 468) and after (N = 185) propensity score matching
Footnote: To match the two cohorts, we used a 1:3 nearest-neighbour matching with age, sex, pack-years and center, without replacement
PI*SS individuals showed a significantly lower probability of having an impaired KCO(%) (i.e. below 80% predicted) compared to PI*ZZ individuals in both the unmatched and matched cohorts and also after additional adjusting for the number of exacerbations in the last year and previous pneumonia (multivariable analysis: odds ratio [OR] 0.29, 95% confidence interval [CI]: 0.14 to 0.57; p < 0.001) (Table 2). In the analysis of FEV1(%), the results were similar, with an increased risk of impairment for individuals with PI*ZZ (Table 2).
Comparison between PI*SS and PI*SZ. Unmatched and matched analysis
In the unmatched analysis, patients in the PI*SS group were older than those with PI*SZ (59.2±13.9 vs. 52.2±16.2 years; p = 0.002) and were less frequently never smokers (23.2% vs. 46.8%; p = 0.002). PI*SS subjects more frequently had lung disease (71.4% vs.- 53.9%; p = 0.014), particularly COPD (41.1% vs- 22.6%; p = 0.003) and chronic bronchitis (7.1% vs.- 1.6%; p = 0.030). Regarding lung function, only FEV1/FVC significantly differed, with lower values for PI*SS (0.67±0.17 vs. 0.73±0.16; p = 0.008). Individuals with the PI*SS genotype were more symptomatic with worse mMRC and BODEx scores (Table 3).
The matched analysis of PI*SS and PI*SZ individuals did not reveal significant differences in lung disease, including COPD, emphysema, bronchiectasis, and asthma (Fig. 2; Table 3). Neither were there significant differences in the age at diagnosis, the Charlson comorbidity index, lung function (Fig. 3), exacerbations, dyspnoea, quality of life indices, or physical activity. As expected, AAT levels were significantly higher in PI*SS compared to PI*SZ subjects (81±23.9 mg/dL vs. 54.3±17 mg/dL; p < 0.001). Figure 4 illustrates the SMD in baseline characteristics between PI*SS and PI*SZ subjects before and after propensity score matching.
Dot plot displaying standardized mean differences in baseline characteristics between SZ and SS patients, before (N = 468) and after (N = 224) propensity score matching
Footnote: To match the two cohorts, we used a 1:3 nearest-neighbour matching with age, sex, pack-years and center, without replacement
Furthermore, no significant differences were found between the groups in the probability of presenting impaired KCO(%) or FEV1(%) in the matched cohort, both before and after adjusting for the additional variables of previous exacerbations and pneumonia (Table 4).
Discussion
The results of our study demonstrate a decreased risk of emphysema and other lung diseases, as well as better lung function and quality of life in PI*SS individuals compared to PI*ZZ subjects in the matched population. However, to our knowledge, no direct comparisons of the risk of lung disease between PI*SS and PI*SZ have been published. Our results indicate that although there were significant differences in serum AAT levels between the PI*SS and PI*SZ genotypes, there were no significant differences in clinical manifestations, i.e. the prevalence of emphysema, COPD, asthma, bronchiectasis, or differences in lung function or quality of life, after careful matching for confounders.
The S allele (Glu264Val) is one of the most frequent variants related to AATD, causing a 40% decrease in circulating AAT protein, with mean serum levels in homozygous PI*SS subjects of 0.82 g/L (95% CI 0.73 to 1.00 g/L) [5]. In addition, the plasma neutrophil elastase inhibitory capacity of PI*SS subjects is approximately half that observed in normal PI*MM individuals, and exposure of the purified S protein to increasing oxidant burdens, as in smokers, resulted in a dose-dependent reduction in the ability of the molecule to inhibit neutrophil elastase [20]. Taken together, these findings suggest that carriers of the PI*SS genotype may be at increased risk of lung disease, particularly if they smoke. On the other hand, AAT serum levels in PI*SS subjects are usually above the considered protective threshold of 0.5 g/L, and the S protein polymerizes very slowly, resulting in negligible hepatic accumulation and circulating polymer concentrations, leading PI*S to be considered as a non-polymerizing variant [4, 9, 21], thereby suggesting a very low (or non-existent) risk of lung disease in the majority of PI*SS individuals. Clarification of the risk of lung disease associated with the PI*SS genotype would require large epidemiological studies, but there is very limited information regarding the clinical characteristics of PI*SS individuals and their risk of lung disease, particularly compared to the most frequent severe deficient genotypes PI*ZZ and PI*SZ.
For the present study we used data from the EARCO international registry, an initiative of the European Respiratory Society, aimed at collecting prospective information about patients with AATD of different deficient genotypes [12]. The EARCO registry provides a unique opportunity to investigate the characteristics of PI*SS individuals and their associated risk for lung disease. The S allele is very common in the Iberian Peninsula, with a prevalence of between 10 and 18% and is particularly frequent in Madeira Island (Portugal), with a prevalence of 18%. It is also frequent in Angola (18.8%) and Namibia (14.7%), probably related to populations of Iberian heritage [2, 4, 10].
Despite the estimated worldwide prevalence of 4,017,900 individuals with the PI*SS genotype, with the greatest prevalence in Central and Western Europe (460,725 individuals) [10], the risk of developing pulmonary disease associated with this genotype is still unclear, as most studies have focused on carriers of the PI*SZ genotype and some individuals with the PI*SS have only occasionally been described [11]. As an example, a meta-analysis on the risk of COPD due to the PI*S allele, found that the OR for COPD in PI*SZ individuals increased by 3.26 compared to normal PI*MM individuals, mainly in active and former smokers. However, there were not enough cases to summarize the risk of COPD in PI*SS homozygotes, nor was the average lung function in this genotype described due to lack of data [7]. Almost 20 years later, publications including PI*SS individuals remain very scarce.
As previously mentioned, our study found no significant differences in clinical manifestations between PI*SS and PI*SZ genotypes. Interestingly, the main lung function parameters analysed (FEV1(%) and KCO(%)) were not significantly different between PI*SS and PI*SZ individuals after matching, but in both cases they were better preserved compared to PI*ZZ subjects. Similarly, the risk of having an impaired FEV1(%) and/or KCO(%) did not significantly differ between PI*SS and PI*SZ genotypes, either before or after accounting for previous episodes of pneumonia and exacerbations. These results suggest that the antielastase protection provided by the two S alleles may be equivalent to the SZ combination; nevertheless, larger prospective studies are needed to confirm this observation.
Our findings raise important questions about the management of PI*SS individuals. Since the PI*SZ genotype increases the risk of emphysema in smokers compared to the “normal” PI*MM population [7, 8], if PI*SS individuals seem to have the same risk, counselling to quit smoking should be similarly intense for both genotypes. Furthermore, the clinical and functional monitoring of PI*SS patients who smoke should be equivalent to that carried out in PI*SZ patients.
Therapeutic considerations can also be raised, since, in selected cases, carriers of the PI*SZ genotype may be candidates for replacement therapy, as expressed in the Summary of Product Characteristics of the different approved ATs and in some guidelines [22,23,24]. In fact, recent data from the Spanish registry showed that 8.2% of registered PI*SZ individuals were receiving AT [25]. Again, if the risk for lung disease associated with PI*SS is not significantly different from that of PI*SZ, it may also be considered that some selected individuals with the PI*SS genotype could benefit from AT [22, 23]. However, similar to PI*SZ, there is no evidence about the efficacy of AT in this population and the great majority (if not all) of subjects with the PI*SS genotype have serum levels above those considered to be protective [5, 6]. In any case, if our results showing a similar risk of lung disease for PI*SS and PI*SZ are confirmed in larger series, this could justify the inclusion of PI*SS subjects in clinical trials of other future preventive treatments under development, such as oral or inhaled elastase inhibitors. It should also encourage debate as to whether there is a universal protective AAT level, and if so where it lies.
The S allele has also been associated with a higher prevalence and increased severity of asthma. Data from the Spanish registry, one of the largest reported samples of PI*SZ individuals, showed that the prevalence of asthma was significantly higher for PI*SZ compared to PI*ZZ subjects [25]. Recent studies have also observed that carriers of the S allele may have more frequent and severe asthma exacerbations [26, 27]. However, our study did not find any significant difference in the prevalence of asthma among the three groups. In fact, the prevalence of neither asthma nor bronchiectasis showed significant differences among the PI*SS, PI*SZ and PI*ZZ genotypes after matching. In any case, our data cannot rule out a possible influence of the S allele on the clinical manifestations, severity or exacerbations of asthma.
Our study has some limitations: firstly, despite careful matching for risk factors we cannot rule out the possibility of other confounders that were not considered. Secondly, there may be some selection bias derived from the potential tendency to register in EARCO the most affected PI*SS individuals, who are the those most frequently diagnosed, but this bias may also apply for the PI*SZ and PI*ZZ individuals. Thirdly, we could not compare PI*SS with a matched cohort of normal PI*MM individuals and, therefore, we can only speculate about an increased risk of lung disease in the PI*SS versus the normal population based on an indirect comparison through the similar risk observed with the PI*SZ genotype. Fourthly, it should be noted that patients in the group characterized by the PI*SS genotype represent only 5.6% of the entire deficient population analysed. Finally, we do not yet have prospective follow-up data that could provide insights into the risk of exacerbations and lung function decline associated with the PI*SS genotype. Future larger studies and/or the future analysis of prospective EARCO data may provide more information about the evolution of these subjects. Conversely, this is the largest study characterizing individuals with the PI*SS genotype and the comparison of these subjects not only with PI*ZZ, but perhaps more importantly, with participants with the PI*SZ genotype, a known risk factor for lung disease in smokers [7, 8] and using propensity score matching and a multivariate analysis of risk factors.
Conclusion
The results of our study suggest that subjects with the PI*SS genotype have a significantly lower risk of lung disease compared with the PI*ZZ genotype, but after careful matching accounting for the most important known confounders we did not find evidence for any significant difference in the risk of lung disease between the PI*SS and PI*SZ genotypes. Since the PI*SZ genotype is considered a genetic risk factor for the development of lung disease in smokers, careful attention and strong anti-smoking counselling should also be given to PI*SS subjects that smoke.
Data availability
No datasets were generated or analysed during the current study.
Abbreviations
- AAT:
-
Alpha-1 antitrypsin
- AATD:
-
Alpha-1 antitrypsin deficiency
- BODEx:
-
Body mass index, obstruction, dyspnoea, and exacerbations index
- CAT:
-
Chronic obstructive pulmonary disease (COPD) Assessment Test
- COPD:
-
Chronic Obstructive Pulmonary Disease
- EARCO:
-
European Alpha-1 antitrypsin Deficiency Research Collaboration
- EQ:
-
Euro-Quality of life index questionnaire
- FEV1:
-
Forced expiratory volume in one second
- FVC:
-
Forced vital capacity
- KCO:
-
Carbon monoxide transfer coefficient
- mMRC:
-
Modified Medical Research Council
- PI:
-
Proteinase inhibitor
- QoL:
-
Quality of life
- PSM:
-
Propensity score matching
- SD:
-
Standard deviation
- SMD:
-
Standardized mean differences
- VAS:
-
Visual analogue scale
References
Strnad P, McElvaney NG, Lomas DA. Alpha1-Antitrypsin Deficiency. N Engl J Med. Apr 2020;9(15):1443–55.
Blanco I, de Serres FJ, Fernandez-Bustillo E, Lara B, Miravitlles M. Estimated numbers and prevalence of PI*S and PI*Z alleles of alpha1-antitrypsin deficiency in European countries. Eur Respir J. 2006;27:77–84.
Elliott PR, Stein PE, Bilton D, Carrell RW, Lomas DA. Structural explanation for the deficiency of S alpha 1-antitrypsin. Nat Struct Biol. 1996;3:910–1.
Seixas S, Marques PI. Known mutations at the cause of alpha 1-antitrypsin deficiency an updated overview of SERPINA I variation spectrum. Appl Clin Genet. 2021;14:173–94.
Ferrarotti I, Thun GA, Zorzetto M, Ottaviani S, Imboden M, Schindler C, et al. Serum levels and genotype distribution of alpha1-antitrypsin in the general population. Thorax. 2012;67:669–74.
Miravitlles M, Dirksen A, Ferrarotti I, Koblizek V, Lange P, Mahadeva R, et al. European respiratory Society Statement: diagnosis and treatment of pulmonary disease in alpha-1 antitrypsin deficiency. Eur Respir J. 2017;50:1700610.
Dahl M, Hersh CP, Ly NP, Berkey CS, Silverman EK, Nordestgaard BG. The protease inhibitor PI*S allele and COPD: a meta-analysis. Eur Respir J. 2005;26:67–76.
McElvaney GN, Sandhaus RA, Miravitlles M, Turino GM, Seersholm N, Wencker M, et al. Clinical considerations in individuals with Alpha-1 antitrypsin PI*SZ genotype. Eur Respir J. 2020;55:pii1902410.
Nuñez A, Belmonte I, Miranda E, Barrecheguren M, Farago G, Loeb E, et al. Association between circulating alpha-1 antitrypsin polymers and lung and liver disease. Respir Res. 2021;22:244.
De Serres F, Blanco I. Prevalence of α1-antitrypsin deficiency alleles PI*S and PI*Z worldwide and effective screening for each of the five phenotypic classes PI*MS, PI*MZ, PI*SS, PI*SZ, and PI*ZZ: a comprehensive review. Ther Adv Respir Dis. 2012;6(5):277–95.
Miravitlles M, Herepath M, Priyendu A, Sharma S, Vilchez T, Vit O, et al. Disease burden associated with alpha-1 antitrypsin deficiency: systematic and structured literature reviews. Eur Respir Rev. 2022;31(163):210262.
Greulich T, Altraja A, Barrecheguren M, Bals R, Chlumsky J, Chorostowska-Wynimko J, et al. Protocol for the EARCO Registry: a pan-european observational study in patients with α1-antitrypsin deficiency. ERJ Open Res. 2020;6:00181–2019.
Miravitlles M, Turner AM, Torres-Duran M, Tanash H, Rodríguez-García C, López-Campos JL, et al. Clinical and functional characteristics of individuals with alpha-1 antitrypsin deficiency: EARCO international registry. Respir Res. 2022;23(1):352.
Miravitlles M, Turner AM, Torres-Duran M, Tanash H, Rodríguez-García C, López-Campos JL, et al. Characteristics of individuals with alpha-1 antitrypsin deficiency from Northern and Southern European countries: EARCO international registry. Eur Respir J. 2023;61(3):2201949.
Jones PW, Harding G, Berry P, Wilkund I, Chen WH, Kline-Leidy N. Development and first validation of the COPD Assessment Test. Eur Respir J. 2009;34:648–54.
EuroQoL Group. EuroQol: a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208.
Greenwood JL, Joy EA, Stanford JB. The physical activity vital sign: a primary care tool to guide counseling for obesity. J Phys Act Health. 2010;7(5):571–6.
Ramon MA, Esquinas C, Barrecheguren M, Pleguezuelos E, Molina J, Quintano JA, et al. Self-reported daily walking time in COPD: relationship with relevant clinical and functional characteristics. Int J Chron Obstruct Pulmon Dis. 2017;12:1173–81.
Soler-Cataluña JJ, Martínez-García MA, Sánchez LS, Tordera MP, Sánchez PR. Severe exacerbations and BODE index: two independent risk factors for death in male COPD patients. Respir Med. 2009;103(5):692–9.
Ogushi F, Hubbard RC, Fells GA, Casolaro MA, Curiel DT, Brantly ML, et al. Evaluation of the S-type of Alpha-1 antitrypsin as an in vivo and in vitro inhibitor of neutrophil elastase. Am Rev Respir Dis. 1988;137:364–70.
Tan L, Dickens JA, Demeo DL, Miranda E, Perez J, Rashid ST, et al. Circulating polymers in α1-antitrypsin deficiency. Eur Respir J. 2014;43:1501–4.
Miravitlles M, Anzueto A, Barrecheguren M. Nine controversial questions about augmentation therapy for alpha-1 antitrypsin deficiency: a viewpoint. Eur Respir Rev. 2023;32(170):230170.
Tonelli AR, Brantly ML. Augmentation therapy in alpha-1 antitrypsin deficiency: advances and controversies. Ther Adv Respir Dis. 2010;4:289–312.
Attaway A, Majumdar U, Sandhaus RA, Nowacki AS, Stoller JK. An analysis of the degree of concordance among international guidelines regarding alpha-1 antitrypsin deficiency. Int J Chron Obstruct Pulmon Dis. 2019;14:2089–101.
Torres-Durán M, López-Campos JL, Rodríguez-Hermosa JL, Esquinas C, Martínez-González C, Hernández-Pérez JM, et al. Demographic and clinical characteristics of patients with α1-antitrypsin deficiency genotypes PI*ZZ and PI*SZ in the Spanish registry of EARCO. ERJ Open Res. 2022;8:00213–2022.
Martín-González E, Hernández-Pérez JM, Pérez JAP, Pérez JAP, Pérez-García J, Herrera-Luis E et al. Alpha-1 antitrypsin deficiency and PI*S and PI*Z SERPINA1 variants are associated with asthma exacerbations. Pulmonology 2023:S2531-0437(23)00091 – 0.
Hernández-Pérez JM, Martín-González E, González-Carracedo MA. Alpha-1 Antitrypsin Deficiency and SERPINA1 variants could play a role in Asthma exacerbations. Arch Bronconeumol. 2023;59(7):416–7.
Acknowledgements
The authors would like to thank the patients who participated in this study and the EARCO study investigators (listed below). We wish to acknowledge Elise Heuvelin and Valerija Arsovski from the ERS office (Lausanne, Switzerland) for her support in the management of EARCO, and Helena Miquel (Bioclever, Barcelona, Spain) for her support in EARCO data monitoring. List of EARCO study investigators: Mariano Fernandez-Acquier, Andrés L. Echazarreta (Argentina), Georg-Christian Funk, Karen Schmid-Scherzer (Austria), Wim Janssens, Silvia Pérez-Bogerd (Belgium), Kenneth Chapman (Canada), Leidy Prada (Colombia), Ana Hecomovic (Croatia), Eva Bartosovska, (Czech Republic), Alan Altraja, Jaanus Martti (Estonia), Eric Y.E. Derom, Maeva Zysman, Jean-François Mornex, Martine Reynaud-Gaubert (France), Timm Greulich, Felix JF Herth, Franziska Trudzinski, Rembert Koczulla, Matthias Welsner (Germany), Gerry McElvaney (Ireland), Angelo G. Corsico, Ilaria Ferrarotti, Simone Scarlata, Mario Malerba, Luciano Corda (Italy), Jan Stolk, Emily F van’t Wout (Netherlands), Joanna Chorowstoska-Wyminko (Poland), Catarina Guimaraes, Maria Sucena, Ana Caldas, Raquel Marçoa, Isabel Ruivo dos Santos, Bebiana Conde, Maria Joana Reis Amado Maia Da Silva, Rita Boaventura, Cristina Santos, Gabriela Santos, Filipa Costa, Joana Gomes, Teresa Martin, Sonia Isabel Silva Guerra (Portugal), Ruxandra Ulmeanu (Romania), María Torres-Duran, Marc Miravitlles, Miriam Barrecheguren, Juan Luis Rodriguez-Hermosa, Myriam Calle-Rubio, José María Hernández-Pérez, José Luis López-Campos, Francisco Casas-Maldonado, Ana Bustamante, Carlota Rodriguez-García, Marta García-Clemente, Cruz González, Eva Tabernero, Lourdes Lázaro, Virginia Almadana, Mar Fernández-Nieto, Francisco Javier Michel de la Rosa, Carlos Martínez-Rivera, Layla Diab, María Isabel Parra, Nuria Rodríguez-Lázaro, Susana Martínez, Rosanel Amaro, Ramon-Antonio Tubio (Spain), Hanan Tanash, Eeva Piitulainen (Sweden), Christian F Clarenbach (Switzerland), Serap Argun Baris, Dilek Karadogan, Sebahat Genç, Ouksel Hakima (Turkey), Alice M Turner, Beatriz Lara, David G Parr, Charlotte Bolton, John Hurst, Ravi Mahadeva, Nicholas Hopkinson (United Kingdom). EARCO Steering committee: Christian F Clarenbach and Marc Miravitlles (Co-chairs), David G Parr, Catarina Guimaraes, Hanan Tanash, Karen O’Hara, Marion Wilkens, José Luis López-Campos, Alice M. Turner, Jens-Ulrik Stæhr Jensen, Maria Torres-Duran, Angelo Corsico.
Funding
The International EARCO registry is funded by unrestricted grants of Grifols, CSL Behring, Kamada, pH Pharma and Takeda to the European Respiratory Society (ERS).
Author information
Authors and Affiliations
Contributions
TM, MM, CE, CG and MS conceptualization, methodology and investigation; TM writing of the manuscript; MM review and editing. CE performed the statistical analysis. All authors participated in the design and acquisition of data. All authors read, performed a critical revision and approved the final manuscript and agree to be accountable for all aspects of the work. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol received central ethics approval by the research ethics committee of the Vall d’Hebron University Hospital of Barcelona, Spain (PR(AG)480/2018) and was subsequently approved by all participating centres. All participants provided written informed consent.
Consent for publication
Not applicable.
Competing interests
Teresa Martín has received speaker fees from AstraZeneca, CSL Behring, and GlaxoSmithKline, consulting fees from GlaxoSmithKline, and support for attending meetings from AstraZeneca, Bial, Boehringer Ingelheim, CSL Behring, Novartis and Medinfar. Catarina Guimarães has received speaker fees from CSL Behring. Cristina Esquinas has received speaker fees from CSL Behring. María Torres-Durán has received either speaker and consulting fees from CSL Behring and Grifols, and support for attending meetings from CSL Behring, Grifols, Chiesi and FAES Farma. Alice M Turner has received either grants or speaker fees from AstraZeneca, GlaxoSmithKline, Boehringer Ingelheim, Chiesi, CSL Behring, Takeda, Vertex and Grifols Biotherapeutics. Hanan Tanash has received speaker fees from AstraZeneca, GlaxoSmithKline, Boehringer Ingelheim, Chiesi and Grifols. Carlota Rodríguez-García has received speaker fees from AstraZeneca, GlaxoSmithKline, Grifols, Chiesi, and CSL Behring, expert testimony for Chiesi, support for attending meetings from Chiesi and Grifols. Angelo Corsico has received speaker fees and honoraria for participation on advisory board from CSL Behring, and honoraria for manuscript writing from Grifols. José Luis López-Campos has received honoraria during the last 3 years for lecturing, scientific advice, participation in clinical studies or writing for publications for (alphabetical order): AstraZeneca, Bial, Boehringer Ingelheim, Chiesi, CSL Behring, Faes, Gebro Pharma, GlaxoSmithKline, Grifols, Megalabs and Menarini. José María Hernández-Pérez has received consulting fees from Grifols and CSL Behring, speaker fees from AstraZeneca, Bial, CSL Behring, FAES laboratory, GlaxoSmithKline, and Grifols, support for attending meetings from Grifols and CSL Behring, and honoraria for participation on advisory board from Grifols. Maria Sucena has received consulting fees from Bial, CSL Behring and Grifols, speaker fees from AstraZeneca, Bial, Boehringer Ingelheim, CSL Behring, Grifols and Novartis, support for attending meetings from Bial, CSL Behring, DarSaúde, Gasoxmed, Grifols, Medinfar and VitalAire, honoraria for participation on advisory board from Bial and CSL Behring. Marc Miravitlles has received speaker fees from AstraZeneca, Boehringer Ingelheim, Kamada, Chiesi, Cipla, Menarini, Rovi, Bial, Sandoz, Takeda, Zambon, CSL Behring, Specialty Therapeutics, Grifols and Novartis, consulting fees from AstraZeneca, Boehringer Ingelheim, Chiesi, GlaxoSmithKline, Bial, Gebro Pharma, Kamada, CSL Behring, Laboratorios Esteve, Ferrer, Mereo Biopharma, Verona Pharma, TEVA, Spin Therapeutics, pH Pharma, Novartis, Sanofi and Grifols and research grants from Grifols. The remaining authors report no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Martín, T., Guimarães, C., Esquinas, C. et al. Risk of lung disease in the PI*SS genotype of alpha-1 antitrypsin: an EARCO research project. Respir Res 25, 260 (2024). https://doi.org/10.1186/s12931-024-02879-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12931-024-02879-y