Abstract
Background
Ethiopia’s health system is overwhelmed by the growing burden of non-communicable diseases (NCDs). In this study, we assessed the availability of and readiness for NCD services and the interaction of NCD services with other essential and non-NCD services.
Methods
The analysis focused on four main NCD services: diabetes mellitus, cardiovascular diseases, chronic respiratory diseases, and cancer screening. We used data from the 2018 Ethiopian Service Availability and Readiness Assessment (SARA) survey. As defined by the World Health Organization, readiness, both general and service-specific, was measured based on the mean percentage availability of the tracer indicators, such as trained staff and guidelines, equipment, diagnostic capacity, and essential medicines and commodities needed for delivering essential health services and NCD-specific services, respectively. The survey comprised 632 nationally representative healthcare facilities, and we applied mixed-effects linear and ordered logit models to identify factors affecting NCD service availability and readiness.
Results
Only 8% of facilities provided all four NCD services. Availability varied for specific services, with cervical cancer screening being the least available service in the country: less than 10% of facilities, primarily higher-level hospitals, provided cervical cancer screening. General service readiness was a strong predictor of NCD service availability. Differences in NCD service availability and readiness between regions and facility types were significant. Increased readiness for specific NCD services was significantly associated with increased readiness for communicable disease services and interacted with the readiness for other NCD services.
Conclusion
NCD service availability has considerable regional variation and is positively associated with general and communicable disease services readiness. Readiness for specific NCD services interacted with one another. The findings suggest an integrated approach to service delivery, focussing holistically on all disease services, is needed. There also needs to be increased attention to reducing resource allocation variation between facility types and locations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
Health systems worldwide are faced with increasing burdens from noncommunicable diseases (NCDs), aggravated by underinvestment in health, shortage of skilled healthcare workers, and the COVID-19 pandemic [1]. Ethiopia, like many low-middle-income countries (LMICs), has been experiencing a significant rise in NCD-related disability and premature mortality in recent years [1,2,3,4].
Over the past three decades, NCD-related deaths have doubled and NCDs accounted for around one-third of all diseases in Ethiopia in 2019 [5], while projections suggest this figure may reach two-thirds of all deaths by 2040 [5]. Cardiovascular diseases, neoplasms, diabetes, chronic respiratory diseases, and chronic kidney diseases are the leading causes of NCD-related deaths, collectively accounting for over half of the top 15 causes of mortality in the country [6]. With nearly 30% of these deaths occurring among individuals under 50 years old, the social, economic, and familial implications are substantial [7].
To tackle the burden of NCDs and their associated consequences and resulting implications, Ethiopia has implemented a comprehensive National Strategy (2014–2016) in alignment with the World Health Organization’s (WHO’s) global framework for addressing NCDs [3]. The national strategic plan primarily focused on improving health promotion and disease prevention to reduce behavioural risk factors and strengthening the primary health care system to address NCDs [3].
To assess progress and demonstrate results, it is crucial to have information on service availability and health system readiness at country and global levels. The WHO’s Service Availability and Readiness Assessment (SARA) survey is one of such tools designed to assess the availability and readiness of health facilities to provide essential and service-specific services. The Ethiopian SARA survey assessed the availability and readiness of facilities for critical healthcare interventions, such as HIV/AIDS, tuberculosis, and NCDs [8].
As defined by WHO, a service is deemed available if a facility manages, diagnoses, treats, or prescribes a patient who is coming to the facility for disease-specific service. At the same time, general and disease-specific readiness refers to the capability of health facilities to deliver service on a specific condition. Accordingly, General Service Readiness (GSR) assesses the overall capacity of health facilities to provide essential health services, which requires the availability and readiness of basic amenities, core equipment, infection prevention measures, diagnostics, and medicines. This capacity is measured by considering tracer items, including trained staff, guidelines, equipment, diagnostic capacity, medicines and commodities that are specific to and necessary for providing services for that particular disease [8, 9]. Detailed descriptions of each indicator can be found in the method section.
Although Ethiopia’s SARA report and a few other studies descriptively assessed the NCD service availability and readiness in the last few years [6, 9,10,11,12,13,14], there is a lack of detailed empirical studies on factors affecting NCD service availability and readiness in the country. In the current study, we used novel approaches to answer three specific questions: [1] does general service readiness predict NCD service availability [2]? is a facility’s readiness to provide NCD services affected by its management and geographic location within the country, and [3] is NCD service readiness associated with the availability and readiness of non-NCD services? The study’s findings will contribute to informing national and subnational initiatives to strengthen the health system to deliver NCD services in the country. In addition, the novel analytical approach used in this study offers valuable insights to investigate health system readiness in Ethiopia and beyond.
Methods
Data source and study setting
The study is a secondary analysis of the 2018 Ethiopian SARA survey [9]. The 2018 Ethiopian survey was undertaken by the Ethiopian Public Health Institute (EPHI) with financial support from the World Bank. Based on the WHO SARA survey tool, implemented in over 20 countries across LMICs, the Ethiopian version of SARA included all facility types and rural and urban areas across the country [8].
Data were collected using a facility inventory questionnaire, which obtained information on the availability of specific items (including location and functional status) and how the facilities are prepared to provide essential health services. The survey used a nationally representative sample stratified by health facility type and managing authority. All hospitals and selected health centres, clinics, and health posts were included. The sample allocation for this survey took into account the skewed distribution of health facilities at the regional level.
The SARA survey included 31 referral hospitals, 116 general hospitals, 156 primary hospitals, 164 health centres, 19 higher clinics, 74 medium clinics, 72 lower clinics and 132 health posts. Health posts, that are not mandated to provide NCD care in the country [7, 9] were excluded from the analysis. Data were collected from October - December 2017. Computer assisted data was collected by trained health providers from the selected facilities. The information entered in the tablets by each interviewer was sent regularly to the EPHI central server by the interviewers for data management and analysis. Detailed sample size calculation and sampling technique can be found in the Ethiopian SARA report [8, 10].
Ethiopia has an estimated population of 117 million in 2021, with the majority of the population (78%) are rural residents. The burden of NCDs and their associated risk factors in Ethiopia vary according to geography and socioeconomic status [6]. Ethiopia’s health care system follows a three-tiered structure— primary, secondary, and tertiary levels of health care—with federal, regional, zone (administrative structure between region and district) and district administration, operating under a unified planning, financing, and reporting framework. The primary level of care includes primary hospitals, health centres and health posts (the lowest-level health system facility, at village level). The government plays a prominent role in delivering health services, including NCD services, especially in rural communities [10]. A detailed description of the country’s health system, including the delivery of NCD services, has been comprehensively reported in previous studies [10, 15].
Statistical analysis
Outcome measures
NCD service availability was based on a response to whether the facility offered diagnosis and management of each of the four NCDs. The responses were coded as either 1 (if the facility provided the service) or 0 (if it did not) [8, 9].
NCD service readiness was based on a dichotomous response (1 = available and 0 otherwise) for a list of five core tracer items (availability of trained staff and guidelines; equipment; diagnostic capacity; and NCD medicines and commodities) required to provide the specific service and aggregated into a mean score (Table 1 provide detailed on the tracer items). Readiness was a composite measure and was restricted to the subset of facilities that offered the service. The service readiness score for each NCD service was calculated based on the mean percentage availability of the tracer indicators for delivering NCD services.
We examined three groups of exposure variables to assess associations with NCD service availability and readiness:
-
(1)
facility characteristics including location (rural or urban), managing authority (public or others), and facility type (hospitals, higher and medium clinics, health centres, and lower clinics).
-
(2)
GSR defined as the mean percentage availability of the following services: basic amenities, basic equipment, standard precautions for infection prevention, diagnostic capacity, and essential medicines (Table 1).
-
(3)
The availability of non-NCD services (communicable disease services), measured based on a response to whether the facility offered diagnosis and management of each non-NCD service. In this study, we included five non-NCD services: maternal health, child health services, tuberculosis, malaria and prevention, care, and management of HIV/AIDS.
-
(4)
Non-NCD service readiness, which measures the facility’s capacity to provide the service. This was assessed in our study based on the availability of tracer items specific to the disease, including maternal health, child health services, tuberculosis, malaria and prevention, care, and management of HIV/AIDS [8, 9].
Table 1 provides a list of tracer items used in the WHO survey. A detailed description of how these indices were constructed and the tracer items for the specific non-NCD service—maternal health, child health services, tuberculosis, malaria and prevention, care, and management of HIV/AIDS—can be found in reports published elsewhere [8, 9]. The scores for the various indicators range from zero to 100, with 100 indicating that the facility possesses all the tracer items and zero suggesting the absence of any tracer items.
To analyse the date, first we first used descriptive statistics to summarize the availability and readiness of NCD services. We then employed multivariate models to answer the three core research questions outlined earlier.
Our multivariate analysis consisted of two broad sets of models [16,17,18]. First, we modelled the probability of NCD service availability as a function of GSR and selected facility characteristics. We included three facility characteristics, location (urban/rural), managing authority and facility type as predictors of NCD availability. The outcome variable consisted of three mutually exclusive response categories—i.e., those providing all four NCD services, those offering some (i.e., at least one but not all) NCD services and those offering none. Since the outcome variable had an ordinal nature and local conditions may influence facility service, we used a mixed-effect ordered-logit model with a random effect at a zonal level.
Subsequently, we modelled the probably of readiness for providing NCD services as a function of two key variables: readiness for communicable disease services (cross-program association) and the readiness for NCD services other than the service attributed to the disease under consideration (between program association, i.e. interaction between different NCD services). Considering the effect of having an extended list of variables on the degree of freedom of the model in a modest sample like ours, we decided to reduce the number of parameters by having just one readiness score for all five communicable diseases (instead of generating a readiness score for each of the five communicable diseases captured in our study). Hence, we combined the readiness measure for these diseases with a simple averaging of the respective readiness scores and called the resulting estimate the communicable disease service readiness score. In this study, we included the following five non-NCD services: maternal health, child health services, tuberculosis, malaria and prevention, care, and management of HIV/AIDS in our analysis.
We included readiness for NCDs to test the difference between program or reciprocal association, excluding the service being analysed as the outcome variable. For example, in the CVD readiness model, we included the combined readiness score for diabetes, chronic respiratory disease, and cancer screening services. We employed mixed-effect linear models with a random effect at a zonal level, considering the continuous nature of the outcome variables and potential area-level factors influencing the availability and readiness of services at a facility level. All models included urban-rural location, managing authority, and facility type as covariates. We applied sample weights to address survey response variations and the unequal probability of facility selection across different geographic locations. The models were estimated using STATA version 18.0.
Results
Characteristics of surveyed health facilities and general service readiness
Out of the 632 health facilities (excluding the 132 health posts), the majority (65%) were public, and 78% were in urban areas. General hospitals represented 18%, and primary hospitals, health centres and clinics each accounted for a quarter of the sample facilities (Table 2 and Appendix I).
Limited NCD services
As shown in Table 2, only 8% (6.2 10.6) of facilities provided all four essential NCD services. Availability varied for specific services, with cervical cancer screening being the least available service in the country: less than 10% of facilities, primarily higher-level hospitals, provided the service. On the other hand, chronic respiratory disease services are available in 53% [95% CI: (49.3, 57.1)] of facilities, cardiovascular disease services in 49% [95% CI: (44.8, 52.6)], and diabetes mellitus services in 37% [95% CI: (32.7, 40.2)] of facilities. None of the lower clinics and only 5% [ 95% CI: (1.3, 7.7)] of health centres provided all four NCD services.
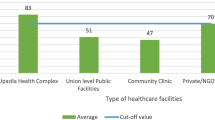
General service readiness
Nationally, all facilities combined had, on average, only half of the required GSR tracer items, 55% [95% CI (54.3, 56.7)]. GSR scores were higher in hospitals (such as referral hospitals at 89.3% [95% CI (86.5, 92.1)]) and urban facilities at 58% [95% CI 6.6, 59.4)] than in health centre at 59% [95% CI (57.6, 61.2)] and rural areas 51.5% [95% CI (49.2, 53.7)]. Referral hospitals (89.3% [95% CI (86.5, 92.1)]) and general hospitals (86.2% [95% CI (84.9, 87.5)]) lacked all the tracer items to provide basic services as their individual scores were well below 100% (See Table 2 and Appendix II). Lower clinics had the lowest general readiness of all facility types, 40.6% [95% CI (39.3, 42.0)] (See Table 2 and Appendix I).
Generally, the proportion of facilities providing services on all four NCDs was higher in more urbanized regions, such as Dire Dawa at 86% [95% CI: (85.6, 100)] and Addis Ababa at 94.5% [95% CI: (77.6, 98.60], than in other jurisdictions. NCD services were also generally more available in hospitals through primary health care units (health centres) and concentrated in facilities with high GSR scores (see Appendix II).
Table 3 describes the associations between GSR, facility type, and NCD service availability. After controlling for facility characteristics, for every 10-unit increase in GSR score, there was an increase in offering some and all NCD services by 0.11% and 0.66%, respectively and a 0.43% decrease in having no NCD service. After controlling for GSR, non-public facilities were associated with higher NCD service availability, which differs from what was observed in Table 2. The significant random effect coefficient indicates the importance of unmeasured locational factors (captured at the zonal level) on NCD service availability. The Inter-Class Correlation (ICC) 0.74 [CI (0.61 0.84) further suggests that about 75% of the variation in NCD service availability in the country can be attributed to location. At the same time, GSR and other facility characteristics contribute to the remaining balance.
Low readiness for NCD services
Table 4 presents NCD service readiness by selected facility characteristics. Accordingly, nationally, half of the facilities in the country had a readiness score of 26% or less, ranging from 46% for diabetes diagnosis and/or management (DDM) to 33% for cardiovascular disease (CVD) service and less than 27% for chronic respiratory disease (CRD) service. Similarly, half of the facilities had none of the tracer items for cervical cancer screening (CSS), and even the top 10% had just 50% of the tracer items for CSS.
Generally, referral hospitals had the highest mean readiness score (72%), followed by other hospital types and higher clinics (47%). Among the top 10% of health facilities, NCD service readiness was as high as 80% or more in referral and general hospitals but less than 40% and 20% in health centres and lower clinics, respectively. Service-specific differences were negligible within the hospital setting, except for CRD, where referral hospitals had a slight edge over other types.
The highest difference in service readiness between locations and management types was at the higher end of the distribution, particularly for cervical cancer screening. The average readiness for CCS in urban areas was about 16% compared to less than 5 in rural areas. However, up to 50% of facilities in both rural and urban areas had no cervical cancer screening. In both non-public and publicly managed facilities, readiness for CRD and CVD among the bottom 10% was about 10 and 25%, respectively, and 50% had no CSS services.
Interaction between NCD and non-NCD service readiness
Table 5 shows the associations between NCD and non-NCD service readiness. Overall, readiness for specific NCD services was significantly associated with readiness for communicable diseases [0.155, 95% CI: (0.046, 0.75)]. The readiness of DDM, CRD, and CSS services was also positively associated with communicable disease service readiness, suggesting complementary between-program effects. Similarly, within-program reciprocal effects (i.e., interaction effects of readiness for a given NCD service on other NCD service readiness) were significant for DDM, CVD and CRD.
Also, location and facility type, rather than under which management the facility is or whether it is in urban or rural areas, were significant predictors of overall NCD service readiness and readiness for specific NCD services. As suggested by the inter-class correlations—i.e., the expected correlation in service readiness between two randomly drawn facilities in the same zone—over a third of the variation in service readiness for diabetes, cervical cancer screening and overall NCD, and up to 43 and 51 per cent of the readiness variations for CVD and CRD services were attributable to differences between locations. The relatively high and significant ICC for all models suggests that including the location (i.e., zone) level random effect variable was imperative as it improved our model estimates. Appendix III shows unadjusted estimate of the associations between NCD and non-NCD service readiness.
Discussion
The burden of NCDs in Ethiopia continues to impact health outcomes and strain the healthcare system negatively. To effectively address this burden, it is crucial to integrate services across primary, secondary, and tertiary care and between different programs. Our study examined the association of NCD service availability with GSR and identified the predictors of NCD service readiness. We also examined the interactions between NCD service readiness and the availability and readiness of various non-NCD services in Ethiopia. There are three key findings from our analysis.
First, we found that GSR strongly predicts the availability of NCD services. Second, the readiness of NCD services has significant interactions with each other and the readiness of communicable disease programs such as HIV/AIDS, malaria, and tuberculosis. Third, we found that between-locality differences in NCD service availability and readiness were large and significant, and so were between facility types, especially for service readiness.
Access to care is crucial for addressing inequalities and reducing the burden of NCDs [11, 12, 19, 20]. However, our results showed that NCD services are limited in Ethiopia. While there has been some improvement compared to previous years—where availability was at 22%, 41%, 45%, and 2% in 2016—the current findings still highlight the limited availability of NCD services within the country’s health system, which is consistent with studies conducted in Ethiopia and other LMICs [11, 14, 19, 20].
Our study also found that the availability of NCD services differed across facility types, managing authorities, and geographical settings. Hospitals, public facilities, and urbanized regions generally had a higher proportion of facilities providing all four NCD services. Medium and higher-level clinics had a higher probability of delivering all four services than hospitals. Similar findings were reported in other studies conducted in Ethiopia and elsewhere, highlighting the absence of NCD services in primary healthcare facilities, public sectors, and rural settings [6, 11, 13, 14, 20, 21].
However, our analysis showed that GSR readiness strongly predicts the availability of NCD services, regardless of facility attributes. In Ethiopia, facilities had only half the required items to provide essential health services, and the shortage was not limited to lower-level facilities. This could be due to the gradual decline in the availability of resources, including fundings, required to provide NCD services in the country [14]. The national GSR reported for Ethiopia was similar to Bangladesh and Nepal for comparable periods [6, 12, 22]. GSR may, however, be a proxy for other factors, such as workforce density, which our analysis did not capture. Moreover, averages do mask the realities beneath, especially if the distributions are skewed, as we have shown to be the case in Ethiopia.
Our results showed a ‘duality gap’ (i.e., wide geographic and facility-type variations) in the Ethiopian health system as resources were more skewed toward higher facilities. Large and significant locational (in this case, zonal level) disparities in the availability and readiness of NCD services also exist, as shown by the results of the random effect coefficient. The ‘duality gap’ has important policy implications because it signifies unequal distribution of health resources between locations and care levels and requires an all-encompassing response that addresses both locational disadvantage and bias in favour of hospital-based care. The drive to address such inequalities requires focusing on the primary health care system and public and rural facilities since these facilities are more accessible to most of the population and can ensure universal health coverage [10, 11, 15, 22]. This is relevant to halt the burden of undiagnosed NCD conditions and chronic morbidity that come with a lack of timely access to services. [11, 22].
The findings suggest that an integrated approach is needed to improve the availability and readiness of NCD services. This includes optimizing resources such as medicine, guidelines, workforce training, and strong leadership for sectoral coordination and engagement with the private sector [11, 13, 21, 23, 24]. Moreover, there is a need to engage the private sector with solid leadership and sectoral coordination of programs [11, 13, 21, 23, 24], as our results suggested a strong association between facility managing authority and NCD service availability. Furthermore, where relevant, there is a need to leverage the country’s prior success in primary health care reforms, primarily in the areas of MCH, HIV and malaria, as these were driven by strong political leadership, good governance, resource commitments, effective stakeholder engagement, and the existence of a well-defined program of action [6, 10, 25,26,27,28].
Improving service availability should go hand in hand with increasing readiness, as many facilities providing NCD services had low readiness scores. A previous report from Ethiopia has shown that access to quality health services is significantly below appropriate minimum standards and the estimated population in need of those services [6]. This indicates that despite the existence of an NCD strategy and NCDs being four of Ethiopia’s top 15 causes of death, service availability and readiness for NCDs are still low [6, 14, 29]. Studies in various settings also suggested sub-optimal service readiness for NCDs [11, 12, 23]. In our research, readiness to provide DDM, CRD and CSS services strongly and positively correlated with overall service readiness for communicable diseases (HIV, malaria, and TB), signifying a strong complementary between-program effect for these services. Similarly, within-program reciprocal effects were found to be substantial for DDM, CVD and CRD. An integrated people-centred care system has the potential to generate significant health and health system benefits, leading to improvements in access and efficiency of services, reduction in personal and health system costs, and optimisation of often scarce human resources [15, 30]. However, despite the benefits, integration needs careful planning as resource scarcity and poor coordination can pose challenges and reverse gains [31, 32].
While our study utilized a novel analytical strategy to answer a complex research question, the study has limitations. First, given the cross-sectional nature of the data used for analysis, the findings reported in the study should be viewed as indicators of associations rather than pointing to a direct cause-and-effect relationship. Particularly, the interaction between the readiness of NCD services and the readiness of communicable disease programs such as HIV/AIDS, malaria, and tuberculosis may require alternative study designs. These interactions may be influenced by other factors and require a comprehensive understanding of the dynamics within the health sector. Second, the sampling frame for the SARA survey included health centers and health posts listed in the country’s master health facility list, which might be incomplete and possibly excludes health facilities, especially newer constructions and private facilities [9].
In addition, the data used for the analysis come from a pre-COVID-19 pandemic period. The pandemic, as in all other countries, disrupted and re-configured healthcare services, as is the ongoing conflict in the country, and these are not captured in our analysis. However, the results still fill a significant knowledge gap and serve as a useful benchmark in rebuilding a resilient health system in the country.
If there was any lesson to be learned from COVID-19, it was the realisation that all health systems are fragile and vulnerable to pandemics, and the weakest link mattered most. As established by the present study, NCD service availability and readiness are Ethiopia’s weakest link, and knowing the gaps, as attempted in the present study, helps focus attention on the effort to build better for future similar eventualities. In addition, the approaches we used for analysing the SARA in the present study are novel and can serve as valuable tools for future researchers using SARA surveys to investigate health system readiness in Ethiopia and beyond.
Conclusion
Despite efforts to enhance the diagnosis and management of NCDs in Ethiopia, the availability and readiness of NCD services remain limited. Furthermore, the readiness of NCD services significantly interacts with each other and with the readiness of communicable disease programs such as HIV/AIDS, malaria, and tuberculosis. Strengthening the healthcare system and integrating services across different levels and programs is essential to address the NCD burden. Additionally, addressing geographic and facility-type variations and improving general service readiness such as infrastructure, essential medicines, diagnostic and laboratory tests, are important factors in reducing disparities, achieving universal health coverage, and mitigating inequities in healthcare access.
Availability of data and materials
All relevant data contributing to the findings are within the paper and in Appendices I, II, and III. As secondary data users, we are restricted by data sharing policy and ethical clearance to share additional data. All request for the original data should be directed to the data custodian, the Ethiopian Public Health Institute.
Abbreviations
- CVD:
-
Cardiovascular disease
- CSS:
-
Cervical cancer screening
- CRD:
-
Chronic respiratory disease
- DDM:
-
Diabetes diagnosis and/or management
- GSR:
-
General Service Readiness
- LMICs:
-
Low-middle-income countries
- NCD:
-
Non-communicable disease
- SARA:
-
Service Availability and Readiness Assessment
- WHO:
-
World Health Organization
References
World Health Organization. Noncommunicable diseases. Key Facts. Geneva: World Health Organization 2021 [Available from: https://www.who.int/news-room/fact-sheets/detail/noncommunicable-diseases.
World Health Organization. Noncommunicable Diseases Progress Monitor 2020. Geneva. 2020. Licence: CC BYNC-SA 3.0 IGO.
Global Burden of Diseases (GBD) COMPARE. Analyze updated data about the world’s health levels and trends from 1990 to 2019. Interactive tool using estimates from the Global Burden of Disease (GBD) study. 2019 [ https://vizhub.healthdata.org/gbd-compare/
World Health Organization. Integrating health services. Technical series on primary health care World Health Organization; 2018.
Global Burden of Diseases (GBD) COMPARE. 2023. https://vizhub.healthdata.org/gbd-foresight/.
Federal Democratic Republic of Ethiopia, Ministry of Health. The Ethiopia Noncommunicable diseases and injuries (NCDI) Commission Report Summary. Addressing the Impact of Noncommunicable Diseases and Injuries in Ethiopia; 2018.
Vladislav Dombrovskiy A, Workneh F, Shiferaw R, Small N, Banatvala. Prevention and control of noncommunicable diseases in Ethiopia. The case for investment. In: World Health Organization, UNDP, editors. Addis Ababa2019. 2019.
World Health Organization. Service Availability and Readiness Assessment (SARA). An annual monitoring system for service delivery. Reference Manual. Version 2.2. 2015. https://www.who.int/publications/i/item/WHO-HISHSI-2014.5-Rev.1.
Ethiopian Public Health Institute, Ethiopia. Services Availability and Readiness Assessment (SARA). 2018.
Tesema AG, Abimbola S, Mulugeta A, Ajisegiri WS, Narasimhan P, Joshi R, et al. Health system capacity and readiness for delivery of integrated non-communicable disease services in primary health care: a qualitative analysis of the Ethiopian experience. PLOS Global Public Health. 2021;1(10):e0000026.
Ammoun R, Wami WM, Otieno P, Schultsz C, Kyobutungi C, Asiki G. Readiness of health facilities to deliver non-communicable diseases services in Kenya: a national cross-sectional survey. BMC Health Serv Res. 2022;22(1):985.
Ghimire U, Shrestha N, Adhikari B, Mehata S, Pokharel Y, Mishra SR. Health system’s readiness to provide cardiovascular, diabetes and chronic respiratory disease related services in Nepal: analysis using 2015 health facility survey. BMC Public Health. 2020;20(1):1163.
Mulugeta TK, Kassa DH. Readiness of the primary health care units and associated factors for the management of hypertension and type II diabetes mellitus in Sidama, Ethiopia. PeerJ. 2022;10:e13797.
Defar A, Zeleke GT, Berhanu D, Lemango ET, Bekele A, Alemu K, et al. Health system’s availability and readiness of health facilities for chronic non-communicable diseases: evidence from the Ethiopian national surveys. PLoS ONE. 2024;19(2):e0297622.
Azeb Gebresilassie Tesema. Improving the prevention and management of non-communicable diseases through primary health care in Ethiopia [Thesis]. Sydney, Australia: University of New South Wales; 2023.
Carlson A, Joshi R. Sample selection in linear panel data models with heterogeneous coefficients. J Appl Econom. 2024;39(2):237–55.
Greene WH. Econometric Analysis. 7th ed. Upper Saddle River, NJ: Prentice Hall; 2012.
Heckman J. Sample selection bias as a specification error. Econometrica. 1979;47:153–61.
Getachew T, Bekele A, Amenu K, Defar A, Teklie H, Taye G, Taddele T, Gonfa G, Getnet M, Gelibo T, Assefa Y. Service availability and readiness for major non-communicable diseases at health facilities in Ethiopia. Ethiop J Health Dev. 2017;31(1):384–90.
Bintabara D, Ngajilo D. Readiness of health facilities for the outpatient management of non-communicable diseases in a low-resource setting: an example from a facility-based cross-sectional survey in Tanzania. BMJ open. 2020;10(11):e040908.
Bintabara D, Shayo FK. Disparities in availability of services and prediction of the readiness of primary healthcare to manage diabetes in Tanzania. Prim Care Diabetes. 2021;15(2):365–71.
Biswas T, Haider MM, Gupta RD, Uddin J. Assessing the readiness of health facilities for diabetes and cardiovascular services in Bangladesh: a cross-sectional survey. BMJ open. 2018;8(10):e022817.
Moucheraud C. Service Readiness for Noncommunicable diseases was low in five countries in 2013–15. Health Aff (Millwood). 2018;37(8):1321–30.
Orji IA, Baldridge AS, Omitiran K, Guo M, Ajisegiri WS, Ojo TM, et al. Capacity and site readiness for hypertension control program implementation in the Federal Capital Territory of Nigeria: a cross-sectional study. BMC Health Serv Res. 2021;21(1):322.
Croke K. The origins of Ethiopia’s primary health care expansion: the politics of state building and health system strengthening. Health Policy Plan. 2020;35(10):1318–27.
Assefa Y, Hill PS, Gilks CF, Admassu M, Tesfaye D, Van Damme W. Primary health care contributions to universal health coverage, Ethiopia. Bull World Health Organ. 2020;98(12):894–A905.
Federal Democratic Republic of Ethiopia, Ministry of Health. Health sector transformation plan, 2015/16 - 2019/20. 2015. https://faolex.fao.org/docs/pdf/eth208347.pdf.
Pamela A, Juma C, Mapa-tassou, Shukri F, Mohamed, Beatrice L, Matanje Mwagomba C, Ndinda M, Oluwasanu, et al. Multi-sectoral action in non-communicable disease prevention policy development in five African countries. BMC Public Health. 2018;18(1):953.
Girum T, Mesfin D, Bedewi J, Shewangizaw M. The Burden of Noncommunicable diseases in Ethiopia, 2000–2016: analysis of evidence from global burden of Disease Study 2016 and Global Health estimates 2016. Int J Chronic Dis. 2020;2020:3679528.
World Health Organization. Framework on integrated, people-centred health services: report by the Secretariat. Sixty-Ninth World Health Assembly; 2016.
Olukemi Adeyemi M, Lyons T, Njim J, Okebe J, Birungi K, Nana, et al. Integration of non-communicable disease and HIV/AIDS management: a review of healthcare policies and plans in East Africa. BMJ Global Health. 2021;6(5):e004669.
Tesema AG, Peiris D, Joshi R, Abimbola S, Fentaye FW, Teklu AM, et al. Exploring complementary and competitive relations between non-communicable disease services and other health extension programme services in Ethiopia: a multilevel analysis. BMJ Global Health. 2022;7(6):e009025.
Acknowledgements
This work benefitted from an incentive grant from the World health Organisation (WHO) as part of the WHO Global Noncommunicable Disease (NCD) Platform for Young Researchers Programme to AGT (Grant Reg 2022/1249356). AGT would like to thank Associate Professor Yohannes Kinfu for guidance on data analysis. All authors would also like to thank the Ethiopian Public Health Institute, Ministry of Health, Ethiopia for providing the survey data.
Funding
AGT received incentive grant from the World health Organization (WHO) as part of the WHO Global Noncommunicable Disease (NCD) Platform for Young Researchers Programme.
Author information
Authors and Affiliations
Contributions
AGT, DP, RJ and SA contributed to the conception of the study. AGT, AHM, contributed to data curation. AGT, conducted formal analysis and visualization. AGT and DP contributed to data interpretation. Writing—original draft preparation: AGT. Writing—review and editing: AGT, DP, RJ, SA, AHM, DB and TC. All authors provided critical intellectual input and revised the final draft manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study has ethics approval from the University of New South Wales (UNSW) Human Research Ethics Committee (HC210066), Sydney, Australia, to conduct a secondary data analysis of the SARA data.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tesema, A.G., Joshi, R., Abimbola, S. et al. Readiness for non-communicable disease service delivery in Ethiopia: an empirical analysis. BMC Health Serv Res 24, 1021 (2024). https://doi.org/10.1186/s12913-024-11455-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-024-11455-5