Abstract
Background
The indiscriminate use of antimicrobials is considered a major contributing factor to the increase in antimicrobial resistance. Community pharmacies are the main source of access to antimicrobials, and pharmacists are in a strategic position to promote rational use of these medicines. Therefore, it is important to know dispensing service quality.
Objective
To evaluate the behavior of pharmacists in dispensing antimicrobials in community pharmacies in northeast Brazil.
Methods
This cross-sectional pilot study was conducted from August to October 2021 in a private community pharmacy chain in Sergipe. Dispensing was evaluated using the simulated patient (SP) technique. Two SP asked the pharmacists for the antimicrobials (case clinic 1: upper respiratory infection; case clinic 2: urinary tract infection) and recorded the service through audio. Dispensing practices were independently analyzed by two researchers based on the tools available in the literature. Data were presented using descriptive statistics.
Results
A total of 54 simulated patient visits were conducted. Based on the 12 steps recommended by the research team for good dispensing, pharmacists asked an average of 1 (±1.17) question for upper respiratory infections and 0.3 (±0.54) for urinary tract infections, as well as provided counseling (mean number of recommendations, 2.6 (±1.44) and 4.5 (±2.35), respectively). As for communication skills, pharmacists had a regular score (3.07 ± 0.34). Furthermore, there was no significant difference in the number of steps and counseling recommendations by pharmacists in dispensing clinical cases 1 and 2 (p = 0.0674).
Conclusion
The quality of antimicrobial dispensing was evaluated as suboptimal, requiring improvements in practice and multifaceted strategies to promote continuing education of these professionals. In addition, awareness actions for the population must be implemented to promote the rational use of antimicrobials and reduce microbial resistance.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Since their discovery, antimicrobials have contributed significantly to the reduction in morbidity and mortality associated with bacterial infections [1]. However, the global increase in their consumption is accompanied by antimicrobial resistance, which is considered one of the main threats to global health [2, 3]. According to the World Health Organization (WHO), approximately 35% of human infections are resistant to available antimicrobials. These data are even more alarming in low- and middle-income countries, with a resistance rate of up to 90% due to factors such as intense infectious disease burdens, regulatory enforcement, and limited essential resources for the diagnosis of diseases [4,5,6]. In addition, in these countries, inappropriate use of these medicines accounts for approximately 6 million deaths annually, with most cases being preventable [7].
Furthermore, approximately 93% of access to antimicrobials comes from community pharmacies, owing to their market penetration and geographic distribution [8]. Thus, community pharmacists are well-positioned to counsel the population [9]. Among the primary services provided by pharmacists, dispensing is highlighted as it serves the largest number of patients [10]. This clinical service guarantees the provision of medicines and other health products through analysis of the technical and legal aspects of the prescription (if applicable), assessment of individual health needs, and provision of interventions in the medication use process, including pharmaceutical counseling and practice documentation [11,12,13].
In Brazil, people have access to medicines through private community pharmacies and/or public pharmacies of the Unified Health System (SUS). In both cases, antimicrobials can only obtain through the prescription of a professional qualified to prescribe and dispensed by pharmacists or under their supervision [7, 8, 14]. Although there are regulations regarding the sale of antimicrobials, enforcement of and compliance with these measures is considered an old issue and difficult to operationalize in view of economic, cultural, information, education, and inspection factors [15, 16].
A recently published systematic review showed that drug dispensing has a positive impact on the clinical, humanistic, and economic outcomes of patients treated in community pharmacies [17]. Similarly, a narrative review indicated a significant improvement in the rational and appropriate use of antimicrobials after dispensing [18]. However, studies conducted in low- and middle-income countries have highlighted that antimicrobial dispensing practices are usually deficient [19]. In addition, most studies have investigated the sales of antimicrobials without prescription, with little emphasis on interventions provided during the service [20, 21]. Such studies may be improved by providing interventions that may be carried out during the dispensing process to reduce the indiscriminate use of antimicrobials and the rates of antimicrobial resistance.
Different methods have been used to assess antimicrobial dispensing practices in community pharmacies [18, 22, 23]. Among them, simulated patients (SPs) are commonly used as they can provide a methodical way of observing the behavior of pharmacists in actual practice [24]. This method helps in the formulation of educational strategies that address deficiencies in practice that will improve behavior and optimize services. Despite this, only a few studies in Brazil have used this method, and none have investigated the dispensing of antimicrobials [25,26,27,28]. Thus, this study aimed to evaluate the dispensing practices for antimicrobials in community pharmacies in northeast Brazil.
Methods
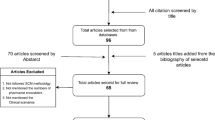
Study design
A cross-sectional pilot study was conducted from August to October 2021, using a simulated patient methodology. The study was reported in accordance with the ‘STROBE Statement—Checklist of items that should be included in reports of cross-sectional studies’ [29] and CRiSP Statement—Checklist for reporting research using simulated patient methodology [30].
Study location and population
This study was conducted in a chain of private community pharmacies in Sergipe, Brazil. The study included pharmacists of both sexes aged over 21 years who worked in community pharmacies and who voluntarily agreed to participate. Pharmacists who could risk the anonymity of the SPs were excluded, that is, pharmacists who knew the simulated patients or those who suspected they were being evaluated (to avoid potential sources of bias). In this study, convenience sampling was performed; therefore, the sample size was not calculated, and pharmacists were selected according to their availability during the simulated visit.
Simulated patients
Simulated patient method
The antimicrobial dispensing practices of the pharmacists were evaluated using SPs. In this method, SPs are specifically trained to simulate elaborate clinical cases identical to a genuine patient. This approach has been described in the literature as an effective method for obtaining objective and reliable data on pharmacists’ dispensing practices in a discrete manner [31,32,33,34].
The participating pharmacies invited their team of pharmacists to participate in the study to learn about the processes carried out by these professionals. Meetings were held between the research team and pharmacists, who were informed that their consultations would be audio-recorded and that the quality of drug dispensing would be evaluated. They were not informed when the simulated visits would occur, who the patients would be, or which clinical cases would be involved. The pilot test started 3 months after collecting data from the participants, and the actual simulated visits occurred 6 months after the pilot test.
The participants were also informed that the data obtained would be analyzed confidentially. Concurrently, the terms of consent were explained to the pharmacists who voluntarily agreed to participate in the study. Sociodemographic characteristics, such as age, sex, undergraduate institution (public or private), time since graduation, postgraduate studies, and time working in a community pharmacy, were collected. After 6 months, simulated visits were carried out for a pilot test and later official visits to participating pharmacies.
The visits followed a schedule agreed upon by the researchers, who determined the pharmacies to be visited and the itinerary to be followed. The dispensing was performed by the pharmacist present at the time of the simulated visit.
Training of SPs
The researchers selected two pharmacy students as SPs, and each was assigned to perform a clinical case to ensure consistency in the simulations (Additional file 1: Appendix A and B). The SPs were trained in a 2-hour workshop, which involved the following steps: presentation of the study objectives, scenario review, standardized scenario study, and instructions on behavior during the simulated visits. A pilot test was conducted with three pharmacists who did not participate in the study to check the functionality of the scenarios and assessment form and to standardize the behavior of SPs [31, 32]. A pre-test of the scenarios and assessment form was carried out by the SPs visiting a pharmacist who did not participate in the study.
Scenarios
Researchers have developed two scenarios through meetings based on SP studies and protocols/recommendations for the treatment of clinical conditions [34,35,36]. Two pharmacists with drug dispensing experience reviewed the clinical cases, and two physicians verified whether the cases represented common clinical scenarios. In the first clinical case, one SP used an antibiotic suspension for upper respiratory tract infection (URTI). In the second clinical case, another SP used antibiotics for urinary tract infection (UTI). These scenarios were developed to reflect the concerns of SPs with different needs. By signing a confidentiality agreement, the physicians who participated in the study voluntarily provided their prescriptions. The SPs were trained to act in a passive manner, only responding to questions from the dispensing pharmacist when asked about the situation. The SPs were instructed not to speak and to wait for counseling spontaneously; if the pharmacists did not provide counseling, the SP asked: “how to use this medication?” (Additional file 1: Appendix A). In addition, for clinical case 2, the simulated patient was instructed to ask the pharmacist: “I have taken antibiotics before and it gave me diarrhea; can this medication also cause diarrhea?” and “I take contraceptive pills; is there a problem?” (Additional file 1: Appendix B).
The SPs visited the pharmacies at various times between April and October 2021. They were instructed to seek care from a pharmacist, and, after the end of dispensing, they were instructed not to buy the medicine. Visits were audio-recorded on a mobile phone.
Evaluation of dispensing practices
Immediately after the visit, each SP evaluated the pharmacists’ communication skills using the instrument developed by Berger et al. [37]; the communication was translated and validated into Brazilian Portuguese by Mesquita et al. [26]. This instrument contains 23 structured items that assessed pharmaceutical counseling and communication skills. For this study, only 13 items assessing communication skills were used to evaluate the simulated visits. These items were answered using a 5-point Likert scale (1-poor, 2-poor, 3-fair, 4-good, 5-excellent). Both SPs received training on how to apply the instrument and performed three pilot tests for calibration. Furthermore, the SPs noted whether the pharmacist provided spontaneous counseling. If the pharmacist actively provided counseling without questions being asked, it was recorded as spontaneous counseling. If the pharmacist provided counseling only after the patient asked questions, it was recorded as nonspontaneous counseling.
To evaluate drug dispensing, the researchers reviewed the scenarios based on the clinical evidence for each clinical case and on the algorithm developed by Rocha et al. [38]. This algorithm presents the clinical reasoning involved in the drug dispensing process, as well as the main questions and counseling that can be provided during this practice. Therefore, the behavior expected of pharmacists in each case was reviewed, discussed, and agreed upon by the researchers according to this algorithm and relevant clinical protocols [34, 36]. From this discussion, 12 steps and 16 counseling recommendations were proposed by the research team for qualified dispensing (three counseling recommendations of the algorithm were not used because they did not apply to clinical cases). Two researchers independently analyzed the audio clips in a pre-formatted Excel spreadsheet. Discrepancies were resolved using a third rater.
Statistical analysis
Data were tabulated and processed in spreadsheets created using Microsoft Excel and BioStat 5.3 softwares for Windows. The normality of continuous variables was verified using the Shapiro-Wilk test. The difference between clinical cases 1 and 2 of the SP with respect to the number of dispensing steps (questions and counseling) and communication skills was evaluated using the Wilcoxon signed-rank test.
To analyze the association between the factors (sex, age, training time, training institution, graduate studies, time working in the private community pharmacy chain) and the number of steps and counseling recommendations in dispensing, the Chi-square test was used. Cramer’s V was used to measure the strength of the association. This test was performed using a statistical software (http://vassarstats.net/newcs.html). The following values were used as a reference: Cramer’s V ≤ 0.2, weak association; 0.2 < Cramer’s V ≤ 0.6, moderate association; and Cramer’s V > 0.6, strong association. For all analyses, the confidence interval was 95%, and the differences were considered statistically significant at p ≤ 0.05.
Ethical considerations
This study was approved by the Ethics Committee in Research Involving Human Beings of the Federal University of Sergipe – CEP/UFS under CAAE 15827719.4.0000.5546 (Register Number 3, 698, 806). All methods were performed in accordance with relevant guidelines and regulations. In addition, prior to data collection, participants were asked to sign the Free and Informed Consent Term e all research participants were informed about the objectives and voluntary nature of the study.
Results
General characteristics of the study participants
Twenty-seven community pharmacists participated in the study, and 54 visits were conducted; the pharmacists were identified with a badge and a specific uniform. The participants’ main characteristics are listed in Table 1. The average age of the pharmacists was 27.9 ± 4.4 years, the average training time was 3.5 ± 3.1 years, and only seven had (25.9%) completed postgraduate studies in the clinic.
The dispensing steps performed by pharmacists during simulated visits are described in Table 2. With regard to the 12 steps recommended by the research team for qualified dispensing, pharmacists performed 1 step on average (minimum:0 | maximum:6) for clinical case 1 and 0.29 step (minimum:0 | maximum:2) for clinical case 2. In clinical case 1, three (11.11%) pharmacists sought to understand the SP’s other health needs, and one (3.70%) questioned whether the SP had undergone a diagnostic test for COVID-19. In clinical case 2, there were no additional questions regarding SP.
Pharmaceutical counseling provided during the simulated visits to clinical cases 1 and 2 is shown in Table 3. The average number of counseling recommendations per simulated visit was 2.6 ± 1.4 for clinical case 1 and 4.5 ± 2.3 for clinical case 2. For clinical case 1, pharmacists provided spontaneous counseling in only six (31.0%) simulated visits, and only three (11.1%) pharmacists provided counseling on how to prepare the suspension. For clinical case 2, the pharmacists provided spontaneous counseling in only two (7.4%) simulated visits.
There was no significant difference between the number of steps and counseling recommendations followed by pharmacists in dispensing for clinical cases 1 and 2 (Z = 1.829; p = 0.067). In addition, the number of steps and counseling recommendations followed during dispensing of medications for clinical cases 1 and 2 was not significantly associated with sex (χ2 = 0.652; p = 0.722; Cramer’s V = 0.155), age (χ2 = 5.444; p = 0.244; Cramer’s V = 0.317), training time (χ2 = 8.593; p = 0.19; Cramer’s V = 0.398), training institution (χ2 = 2.716; p = 0.257; Cramer’s V = 0.317), graduate degree (χ2 = 2.419; p = 0.298; Cramer’s V = 0.299), or time spent working in the private community pharmacy chain (χ2 = 5.251; p = 0.262; Cramer’s V = 0.311). In four (14.8%) visits, pharmacists advised on the importance of correct use and adherence to antimicrobial treatment due to antimicrobial resistance.
The results for the communication skills are presented in Table 4. The pharmacists only dedicated enough time on 15 (55.5%) visits (approximately 5 min well-spent) to patient care. During six (22.2%) visits, pharmacists provided written counseling. No pharmacist provided counseling on what to do in case of doubt.
Discussion
This study investigated the practices of pharmacists regarding the dispensing of antimicrobials in community pharmacies in Sergipe, Brazil, showing deficiencies in the dispensing process, such as asking sufficient questions to assess the SPs’ needs and, consequently, providing appropriate recommendations. Similarly, other studies have reported that most pharmacists dispensed antimicrobials without asking about the previous use of the requested medication, allergy history, or associated symptoms [39, 40]. The literature indicates that several factors can contribute to this scenario, such as the characteristics of the SP’s case, pharmacists’ lack of time or knowledge, and intrinsic patient factors [22, 34, 37, 41]. Obtaining information during dispensing is essential for decision making and adequate counseling [38]. Therefore, it is important that strategies are developed so that pharmacists can adopt well-defined work processes.
Most pharmacists provided a limited amount of counseling for both clinical cases, which could compromise the patients’ proper use of antimicrobials. Pharmaceutical counseling is an essential component of dispensing, even though there are factors that may influence its quantity and quality [38]. Pharmacist training may be one such factor, as suggested by a study in Republika Srpska, Bosnia, and Herzegovina, in which training initiatives reduced the rate of antimicrobial dispensing without a prescription in community pharmacies from 58 to 18.5% [42, 43]. This finding is similar to that of other studies showing that pharmacist training initiatives reduce inappropriate antimicrobial dispensing and should be continued. But there are also contrary study results in the international literature, showing that interventions are not always successful [44,45,46]. Thus, the adoption of multifaceted strategies to improve dispensing practices is key to promoting rational use of antimicrobials.
In general, SPs in clinical case 2 (UTI) received more instructions than SPs in clinical case 1 (URTI). This can be explained by the scenario itself, in which the patient in clinical case 2 exhibited a more active behavior. The study by Alaqeel and Abanmy [39] supports this finding, wherein they observed a referral rate of 3%, which improved to 43% when SPs requested additional information. This attitude is consistent with the literature, which reports an association between a patient’s active behavior and the provision of more information [47, 48]. Additionally, patients should be encouraged to take an active role in developing their autonomy and self-care and, consequently, their co-responsibility for their health [49, 50]. Thus, pharmacist-patient communication should be stimulated.
In this study, a limited spontaneous counseling rate was observed in both the clinical cases. In contrast, a study carried out in Slovakia found higher rates of spontaneous counseling (55.6%) of visits [51]. The literature shows that counseling rates are influenced by factors such as the complexity of the clinical case, time limitations, intense flow of people, knowledge of the pharmacist, and attitude of patients [48, 52]. A study conducted in Asia highlighted that inadequate clinical experience and insufficient knowledge of antimicrobials are the main factors for deficient antimicrobial dispensing [52]. However, without counseling, the interaction between the pharmacist and patient is reduced to a commercial transaction [51]. Thus, a proactive attitude should be encouraged among pharmacists to improve the quality of their practice.
The pharmacists’ communication skills were generally evaluated as regular. These data are superior to those of a previous study conducted in Sergipe, which showed that pharmacists had low scores for these skills [26]. Communication skills contribute to the establishment of a pharmacist-patient therapeutic relationship, which is necessary for the provision of quality health care [53]. Furthermore, such skills, added to the quality of pharmaceutical counseling provided to patients, have the potential to increase user loyalty to pharmacies [54]. Thus, improving competence can be a strategy for improving the quality of care.
Therefore, several factors can be identified as causing deficiencies in pharmacist dispensing practices. For instance, their academic training may be deficient in defined work processes, thus hindering efficient dispensing. Studies have indicated that the absence of systematized and reproducible work processes in dispensing results in inconsistent pharmaceutical interventions in clinical practice [55, 56]. Therefore, it is necessary to develop training strategies to ensure that pharmacists follow the best standards of patient care.
Moreover, a high number of patients to use community pharmacies as a first resource for obtaining medicines and correlates, may compromise the quality of dispensing of medicines, because pharmacists may feel pressured to provide a fast service that can serve a greater number of people without the provision of quality pharmaceutical counseling. In addition, studies report that patients often distort the role of the pharmacist and do not view community pharmacies as health units, with their view of the pharmacy as a provider of rapid care [57,58,59].
Limitations
Although repeated training was carried out to ensure consistency between the SPs’ performance and to increase the internal validity of the collected data, it is still possible that some interpersonal differences have occurred, especially regarding the subjective items of communication skills. In addition, a real patient has the tendency to communicate freely about his/her pathology; therefore, the results measured by this method may differ in real situations. Furthermore, the application of the consent form and convenience sampling adopted in this study may have caused a selection bias. Thus, the small number of participants in this study may have affected the results, suggesting caution when generalizing these results.
Conclusion
This study shows that antimicrobial dispensing practices in community pharmacies are insufficient. Most pharmacists did not ask questions to assess the health needs of the SPs. The counseling rate was low, and pharmacists provided more counseling upon request for information. In general, the pharmacists’ communication skills were considered fair. Policymakers, pharmacy managers, and pharmacists must create strategies to improve antimicrobial dispensing practices. Therefore, patient education and continuing professional education be implemented to promote the rational use of antimicrobials.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- COVID-19:
-
Coronavirus Disease 2019
- SP:
-
Simulated Patient
- URTI:
-
Upper Respiratory Tract Infection
- UTI:
-
Urinary Tract Infection
- WHO:
-
World Health Organization
References
World Health Organization (WHO). Antimicrobial resistance: global report on surveillance. 2014. https://apps.who.int/iris/handle/10665/112642. Accessed 11 Jun 2020.
Schmiege D, Evers M, Kistemann T, Falkenberg T. What drives antibiotic use in the community? A systematic review of determinants in the human outpatient sector. Int J Hyg Environ Health. 2020;226:113497. https://doi.org/10.1016/j.ijheh.2020.113497.
World Health Organization (WHO). Report on surveillance of antibiotic consumption: 2016-2018 early implementation. 2018. https://www.who.int/publications/i/item/who-report-on-surveillance-of-antibiotic-consumption. Accessed 2 Feb 2022.
World Health Organization (WHO). Assessing non-prescription and inappropriate use of antibiotics: report on survey. 2020. https://apps.who.int/iris/bitstream/handle/10665/312306/9789289054089-eng.pdf?sequence=1&isAllowed=y. Accessed 2 Nov 2022.
Almeida Santimano NM, Foxcroft DR. Poor health knowledge and behaviour is a risk for the spread of antibiotic resistance: survey of higher secondary school students in Goa, India. Perspect Public Health. 2017;137:109–13.
Salim AMA, Elgizoli B. Exploring the reasons why pharmacists dispense antibiotics without prescriptions in Khartoum state, Sudan. Int J Pharm Pract. 2017;25:59–65.
Torres NF, Chibi B, Middleton LE, Solomon VP, Mashamba-Thompson TP. Evidence of factors influencing self-medication with antibiotics in low and middle-income countries: a systematic scoping review. Public Health. 2019;168:92–101. https://doi.org/10.1016/j.puhe.2018.11.018.
Chang J, Ye D, Lv B, Jiang M, Zhu S, Yan K, et al. Sale of antibiotics without a prescription at community pharmacies in urban China: a multicentre cross-sectional survey. J Antimicrob Chemother. 2017. https://doi.org/10.1093/jac/dkw519.
Department of Health and Social Care (DHSC) United Kingdom. 5-year action plan for antimicrobial resistance 2019 to 2024: Department of Health and Social Care; 2019. https://www.gov.uk/government/publications/uk-5-year-action-plan-for-antimicrobialresistance-2019-to-2024. Accessed 21 Jan 2022.
Patel M, Campbell M, Moslem M, Spriggel P, Warholak T. Identifying drug therapy problems through patient consultation at community pharmacies: A quality improvement project. J Patient Saf. 2020;16:19–23. https://doi.org/10.1097/PTS.0000000000000228.
Brasil. Portaria No 3.916, de 30 de outubro de 1998. Ministério da Saúde 1998. https://bvsms.saude.gov.br/bvs/saudelegis/gm/1998/prt39. Accessed 7 Fev 2022.
Hernández A, Garcia-Delgado P, Garcia-Cardenas V, Ocaña A, Labrador E, Orera ML, et al. Characterization of patients’ requests and pharmacists’ professional practice in oropharyngeal condition in Spain. Int J Clin Pharm. 2015;37:300–9. https://doi.org/10.1007/s11096-014-0053-4.
National Health Service (NHS) United Kingdom. NHS community pharmacy services – a summary: Psnc; 2013. http://psnc.org.uk/wp-content/uploads/2013/08/CPCF-summary-July-2013.pdf
Brazil. Ministry of Health/Brazilian Health Regulatory Agency (Anvisa). Resolution Rdc No. 471, February 23, 2021. Provides for the criteria for the prescription, dispensing, control, packaging and labeling of medicines based on substances classified as antimicrobials for prescription use, alone or in combination, listed in Normative Instruction specific. Brasília:MS. 2021. Available at: https://www.in.gov.br/web/dou/-/resolucao-rdc-n-471-de-23-de-fevereiro-de-2021-304923190. Accessed 2 Aug 2022.
Sampaio PD, Sancho LG, Lago RF. Implementação da nova regulamentação para prescrição e dispensação de antimicrobianos: possibilidades e desafios. Cad Saúde Coletiva. 2018;26:15–22.
Del Fiol FD, Bergamaschi CD, De Andrade IP Jr, Lopes LC, Silva MT, Barberato-Filho S. Consumption trends of antibiotics in Brazil during the COVID-19 pandemic. Front Pharmacol. 2022;13:844818.
Pizetta B, Raggi LG, Rocha KSS, Cerqueira-Santos S, de Lyra-Jr DP, dos Santos Júnior GA. Does drug dispensing improve the health outcomes of patients attending community pharmacies? A systematic review. BMC Health Serv Res. 2021;21:764. https://doi.org/10.1186/s12913-021-06770-0.
Sakeena MHF, Bennett AA, McLachlan AJ. Enhancing pharmacists’ role in developing countries to overcome the challenge of antimicrobial resistance: a narrative review. Antimicrob Resist Infect Control. 2018;7:63. https://doi.org/10.1186/s13756-018-0351-z.
Belachew SA, Hall L, Selvey LA. Non-prescription dispensing of antibiotic agents among community drug retail outlets in sub-Saharan African countries: a systematic review and meta-analysis. Antimicrob Resist Infect Control. 2021;10:13. https://doi.org/10.1186/s13756-020-00880-w.
Batista AD, Rodrigues DA, Figueiras A, Zapata-Cachafeiro M, Roque F, Herdeiro MT. Antibiotic dispensation without a prescription worldwide: A systematic review. Antibiotics (Basel). 2020:9. https://doi.org/10.3390/antibiotics9110786.
Chang J, Xu S, Zhu S, Li Z, Yu J, Zhang Y, et al. Assessment of non-prescription antibiotic dispensing at community pharmacies in China with simulated clients: a mixed cross-sectional and longitudinal study. Lancet Infect Dis. 2019;19:1345–54. https://doi.org/10.1016/S1473-3099(19)30324-X.
Shi L, Chang J, Liu X, Zhai P, Hu S, Li P, et al. Dispensing antibiotics without a prescription for acute cough associated with common cold at community pharmacies in Shenyang, northeastern China: A cross-sectional study. Antibiotics (Basel). 2020:9. https://doi.org/10.3390/antibiotics9040163.
Torres NF, Solomon VP, Middleton LE. “Antibiotics heal all diseases”; the factors influencing the pratices of self-medication with antibiotics in Maputo City, Mozambique. J Public Health. 2021. https://doi.org/10.1007/s10389-020-01416-7.
De Almeida Neto AC, Benrimoj SI, Kavanagh DJ, Boakes RA. Novel educational training program for community pharmacists. Am J Pharm Educ. 2000;64:302–7.
Obreli-Neto PR, Pereira LRL, Guidoni CM, de Baldoni AO, Marusic S, de Lyra-Júnior DP, et al. Use of simulated patients to evaluate combined oral contraceptive dispensing practices of community pharmacists. PLoS One. 2013;8:e79875. https://doi.org/10.1371/journal.pone.0079875.
Mesquita AR, de Oliveira Sá DAB, Santos APAL, de Almeida NA, Lyra DP. Assessment of pharmacist’s recommendation of non-prescription medicines in Brazil: a simulated patient study. Int J Clin Pharm. 2013;35:647–55. https://doi.org/10.1007/s11096-013-9787.
Santos AP, Mesquita AR, Oliveira KS, Lyra DP Jr. Assessment of community pharmacists’ counselling skills on headache management by using the simulated patient approach: a pilot study. Pharm Pract. 2013;11:3–7.
Da Rocha CE, Bispo ML, dos Santos ACO, Mesquita AR, Brito GC, de Lyra DP. Assessment of community pharmacists’ counseling practices with simulated patients who have minor illness. J Soc Simul Healthc. 2015;10:227–38.
von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. PLoS Med. 2007;4:e296.
Amaratunge S, Harrison M, Clifford R, Seubert L, Page A, Bond C. Developing a checklist for reporting research using simulated patient methodology (CRiSP): a consensus study. Int J Pharm Pract. 2021;29:218–27.
Chong WW, Aslani P, Chen T. Adherence to antidepressant medications: An evaluation of community pharmacists counseling practices. Patient Prefer Adherence. 2013;813. https://doi.org/10.2147/PPA.S48486.
Schneider CR, Gudka S, Fleischer L, Clifford RM. The use of a written assessment checklist for the provision of emergency contraception via community pharmacies: a simulated patient study. Pharm Pract. 2013;11:127–31. https://doi.org/10.4321/S1886-36552013000300001.
Björnsdottir I, Granas AG, Bradley A, Norris P. A systematic review of the use of simulated patient methodology in pharmacy practice research from 2006 to 2016. Int J Pharm Pract. 2020;28:13–25.
Kalra MG, Higgins KE, Perez ED. Common questions about streptococcal pharyngitis. Am Fam Physician. 2016;94:24–31 http://www.ncbi.nlm.nih.gov/pubmed/27386721.
Mesquita AR, Santos EA, Porto JG, Barros IMC, Lyra DP. Translation in brazilian portuguese and content validation of the instrument “Avaliação do Processo de Atendimento Farmacêutico”. Lat Am J Pharm. 2012;31:1422–9.
de Rossi P, Cimerman S, Truzzi JC, da Cunha CA, Mattar R, Martino MDV, et al. Joint report of SBI (Brazilian Society of Infectious Diseases), FEBRASGO (Brazilian Federation of Gynecology and Obstetrics Associations), SBU (Brazilian Society of Urology) and SBPC/ML (Brazilian Society of Clinical Pathology/laboratory medicine): recomm. Braz J Infect Dis. 2020;24:110–9. https://doi.org/10.1016/j.bjid.2020.04.002.
Berger K, Eickhoff C, Schulz M. Counselling quality in community pharmacies: implementation of the pseudo customer methodology in Germany. J Clin Pharm Ther. 2005;30:45–57. https://doi.org/10.1111/j.1365-2710.2004.00611.x.
Rocha KSS, Cerqueira Santos S, Boaventura TC, Santos Júnior GA, Araújo DCSA, Silvestre CC, et al. Development and content validation of an instrument to support pharmaceutical counselling for dispensing of prescribed medicines. J Eval Clin Pract. 2020;26:134–41. https://doi.org/10.1111/jep.13102.
Alaqeel S, Abanmy NO. Counselling practices in community pharmacies in Riyadh, Saudi Arabia: a cross-sectional study. BMC Health Serv Res. 2015;15:557. https://doi.org/10.1186/s12913-015-1220-6.
Bin Abdulhak AA, Al Tannir MA, Almansor MA, Almohaya MS, Onazi AS, Marei MA, et al. Non prescribed sale of antibiotics in Riyadh, Saudi Arabia: A cross sectional study. BMC Public Health. 2011;11:538. https://doi.org/10.1186/1471-2458-11-538.
Paravattil B, Kheir N, Yousif A. Utilization of simulated patients to assess diabetes and asthma counseling practices among community pharmacists in Qatar. Int J Clin Pharm. 2017;39:759–68.2.
Marković-Peković V, Grubiša N. Self-medication with antibiotics in the republic of Srpska community pharmacies: pharmacy staff behavior. Pharmacoepidemiol Drug Saf. 2012;21:1130–3. https://doi.org/10.1002/pds.3218.
Markovic-Pekovic V, Grubiša N, Burger J, Bojanić L, Godman B. Initiatives to reduce nonprescription sales and dispensing of antibiotics: findings and implications. J Res Pharm Pract. 2017;6:120. https://doi.org/10.4103/jrpp.JRPP_17_12.
Puumalainen II, Peura SH, Kansanaho HM, Benrimoj CSI, Airaksinen MSA. Progress in patient counselling practices in Finnish community pharmacies. Int J Pharm Pract. 2010;13:149–56.
Langer B, Kieper M, Laube S, Schramm J, Weber S, Werwath A. Assessment of counselling for acute diarrhoea in north-eastern German pharmacies—A follow-up study using the simulated patient methodology. J Pharm Pharmacol. 2018;9:257–69.
Collins JC, Schneider CR, Naughtin CL, Wilson F, de Almeida Neto AC, Moles RJ. Mystery shopping and coaching as a form of audit and feedback to improve community pharmacy management of non-prescription medicine requests: an intervention study. BMJ Open. 2017;7:e019462.2.
Maes KA, Hersberger KE, Lampert ML. Pharmaceutical interventions on prescribed medicines in community pharmacies: focus on patient-reported problems. Int J Clin Pharm. 2018;40:335–40. https://doi.org/10.1007/s11096-018-0595-y.
Seiberth S, Bauer D, Schönermarck U, Mannell H, Stief C, Hasford J, et al. Implementation of a renal pharmacist consultant service — information sharing in paper versus digital form. J Clin Pharm Ther. 2021;46:838–45. https://doi.org/10.1111/jcpt.13371.
Arrieta VI. Autonomies in interaction: dimensions of patient autonomy and non-adherence to treatment. Front Psychol. 2019:10. https://doi.org/10.3389/fpsyg.2019.01857.
Håkansson Eklund J, Holmström IK, Kumlin T, Kaminsky E, Skoglund K, Höglander J, et al. “Same same or different?” A review of reviews of person-centered and patient-centered care. Patient Educ Couns. 2019;102:3–11. https://doi.org/10.1016/j.pec.2018.08.029.
Mináriková D, Fazekaš T, Minárik P, Jurišová E. Assessment of patient counselling on the common cold treatment at Slovak community pharmacies using mystery shopping. Saudi Pharm J. 2019;27:574–83. https://doi.org/10.1016/j.jsps.2019.02.005.
Zawahir S, Lekamwasam S, Aslani P. Community pharmacy staff’s response to symptoms of common infections: a pseudo-patient study. Antimicrob Resist Infect Control. 2019;8:60. https://doi.org/10.1186/s13756-019-0510-x.
Mesquita AR, Lyra DP, Brito GC, Balisa-Rocha BJ, Aguiar PM, de Almeida Neto AC. Developing communication skills in pharmacy: A systematic review of the use of simulated patient methods. Patient Educ Couns. 2010;78:143–8. https://doi.org/10.1016/j.pec.2009.07.012.
Patrícia Antunes L, Gomes JJ, Cavaco AM. How pharmacist–patient communication determines pharmacy loyalty? Modeling relevant factors. Res Soc Adm Pharm. 2015;11:560–70. https://doi.org/10.1016/j.sapharm.2014.11.003.
Cerqueira-Santos S, Rocha KSS, Araújo DCSA, Santos Júnior GA, Menezes PWS, Sanchez JM, et al. Which factors may influence the implementation of drug dispensing in community pharmacies? A qualitative study. J Eval Clin Pract. 2022. https://doi.org/10.1111/jep.13731.
Mobarak DM, Al-Tabakha MM, Hasan S. Assessing hormonal contraceptive dispensing and counseling provided by community pharmacists in the United Arab Emirates: a simulated patient study. Pharm Pract (Granada). 2019;17:1465.2.
Dosea AS, Brito GC, Santos LMC, Marques TC, Balisa-Rocha B, Pimentel D, et al. Establishment, implementation, and consolidation of clinical pharmacy services in community pharmacies. Qual Health Res. 2017;27:363–73.
Eades CE, Ferguson JS, O’Carroll RE. Public health in community pharmacy: A systematic review of pharmacist and consumer views. BMC Public Health. 2011;11:582.
Hindi AMK, Schafheutle EI, Jacobs S. Patient and public perspectives of community pharmacies in the United Kingdom: A systematic review. Health Expect. 2018;21:409–28.
Acknowledgements
Thanks to the community pharmacies and pharmacists who accepted to be part of the study and the study partners, and physicians who provided the prescriptions for the execution of the simulated patient.
Funding
This study was financed in part by the “Coordenação de Aperfeiçoamento de Pessoal de Nível Superior – Brasil (CAPES) - Finance Code 001”. The funder had no role in the design of the study; collection, analysis, and interpretation of data; or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
EVS, SCS, KSSR, and DPLJ made substantial contributions to the conception and design of this study. EVS, LJSCV, SNPS, and ROSS performed the acquisition, analysis, and interpretation of data. EVS and LJSCV drafted the manuscript. KSSR, SCS, and DPLJ reviewed and made important contributions to the structure and content of the manuscript. All authors have accepted the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee in Research Involving Human Beings of the Federal University of Sergipe – CEP/UFS under CAAE 15827719.4.0000.5546 and opinion number 3,698,806. All methods were performed in accordance with relevant guidelines and regulations. In addition, all research participants were informed about the objectives and voluntary nature of the study prior to data collection and were asked to sign the Free and Informed Consent Terms.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Appendix A.
Case 01 of Simulated /Patient. Appendix B. Case 02 of Simulated Patient.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
de Souza, E.V., Vieira, L.J.S.C., dos Santos, S.N.P. et al. Evaluation of pharmacist’s practices regarding the antimicrobials dispensing: a simulated patient study. BMC Health Serv Res 22, 1576 (2022). https://doi.org/10.1186/s12913-022-08853-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12913-022-08853-y