Abstract
Background
Nurses are increasingly demanded to achieve gold-standards of care with fewer resources. Dealing effectively with stress experienced in their daily-work-life is thus crucial. This study is based on the Demands-Resources-and-Individual-Effects (DRIVE) Nurses Model and applied the person-centred approach with a twofold objective: 1. to identify patterns of coping strategies (Problem-Focused; Seek-Advice; Self-Blame; Wishful-Thinking; Escape/Avoidance) adopted by nurses to deal with perceived stress; 2. to explore potential differences in perceived Demands (Effort), Resources (Rewards, Job-Control, Social-Support), and Psychopathological Symptoms (Anxiety, Phobic-Anxiety, Obsessive–Compulsive, Somatization, Depression, Interpersonal-Sensitivity, Hostility, Psychoticism, Paranoid-Ideation) according to the emerged patterns.
Method
This cross-sectional study was reported by using the STROBE Checklist. Overall, 265 nursing professionals completed self-report measures. Non-hierarchical k-means-cluster-analysis was employed to derive patterns of coping. MANOVAs were used to test differences in Demands, Resources, and Psychopathological Symptoms according to the emerged patterns.
Results
Three stable and meaningful patterns of coping were identified and labelled as Active/Solution-Oriented, Dysregulated/Emotion-focused, and Passive/Disengaged. Nurses belonging to Dysregulated/Emotion-focused group emerged to be at higher risk (higher effort/psychopathological suffering; lower resources) – followed by Passive/Disengaged group – in comparison with nurses belonging to Active/Solution-Oriented group.
Conclusion
Fostering nurses’ awareness of their latent coping patterns and supporting active approaches/emotional regulation strategies for stress management should represent a key goal when defining interventions promoting nurses’ health within/beyond the healthcare settings.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.In the last decades, there has been a growing concern about the need to promote health and safety in the healthcare sectors worldwide [1, 2], with tailored attention given to nursing professionals [3, 4]. Nurses are, indeed, on the front line within the wards, and they are recognized to be at higher risk of perceiving noteworthy levels of stress [5, 6] and feeling emotionally exhausted than other healthcare professionals [7, 8]. Several studies have, therefore, targeted this population to develop research, programs/interventions promoting their psychological and occupational health [9,10,11].
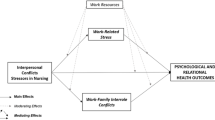
In this direction, a tailored and statistically valid model has been developed to assess stress-and-health processes among nurses, namely the Demands-Resources and Individual Effects (DRIVE) Nurses Model [12,13,14]. The model allows researchers and practitioners to account for the effects of a wide range of risks and protective factors (e.g., Demands/Resources), and it gives pivotal attention to the role of Individual Characteristics, such as coping strategies, in influencing nurses’ psychophysical health [12,13,14].
In line with the abovementioned research trend, which emphasizes workers’ subjectivity, research has started to adopt a “person-centred approach” increasingly [15], namely a conceptual framework entailing the adoption of specific statistical methods (e.g., cluster analyses) to identify individuals with similar patterns and, accordingly, to develop targeted support interventions [16]. This approach has been widely used in occupational health research [e.g., 17–20] and it has also been adopted to identify individuals with similar patterns of coping strategies to deal with stress [21,22,23,24]. Indeed—in real life—people can perceive events differently and resort to more than one coping strategy to deal with situations. Accordingly – nowadays – it is more and more clear that research and interventions need to account for individual differences and nuances.
Therefore, the present study proposed a research application of the DRIVE-Nurses Model [12,13,14] and adopted the person-centred approach [15,16,17,18,19,20,21,22,23,24] to go in-depth into stress-and-health processes among nursing professionals by exploring nurses’ subjectivity. Specifically, the study aimed to first identify specific groups of nurses who could be distinguished according to unique patterns of coping strategies adopted to deal with perceived stress and, therefore, to explore potential differences among nurses belonging to the different groups in terms of perceived occupational and psychological health.
Theoretical background
The DRIVE-nurses model
The DRIVE-Nurses Model [12,13,14] integrates the most renowned transactional and multidimensional perspectives to investigate stress and health processes among nurses by accounting for the effects of the interplay among a wide set of risks and protective factors, namely Demands, Resources, and Individual Characteristics. However, it primarily emphasises the need to understand the complex role played by Individual Characteristics in influencing nurses' stress processes and wellbeing. The potential benefits of adopting the abovementioned approach are numerous. Firstly, in real-life situations, nurses are exposed simultaneously to multiple stressors, and they can also possess different resources to deal with them [25,26,27,28,29,30]. Accordingly, research needs to consider the interplay among multiple factors to account for such complexity. Secondly, even when exposed to the same sources of pressure nurses may perceive and assess them differently/and act accordingly, so they may report varied and distinguished health outcomes. Therefore, a thorough investigation into nurses’ individual differences (i.e., coping strategies) is needed to promote their wellbeing effectively. Thirdly, since many sources of pressure specifically related to nursing—which is by nature a very risk-prone profession [7, 12, 31,32,33]—cannot be displaced (e.g., high workload, performing night shifts, dealing with illness/death), the alternative of developing interventions supporting/enhancing nurses’ individual resources rather than working on contextual factors is promising for promoting nurses’ wellbeing within and beyond the healthcare settings.
Coping research
Coping is defined as the thoughts and behaviours mobilized by individuals to manage internal and external stressful situations [34, 35]. Coping responses have been widely studied in the literature, they have been labelled in different ways, and assessed by using diverse measurement tools [36,37,38,39,40,41,42]. However, despite the specificities, there is a rather great consensus on adopting broad categories—derived from theory and research – to label coping strategies. The first – and more adopted – coping taxonomy concerns the classification into emotion-focused coping strategies (i.e., efforts made to manage the negative emotions linked to the stressful situation) and problem-focused coping strategies (i.e., efforts made to actively face the situation by taking actions/making plans to change it) [36,37,38,39,40,41,42]. However, coping has often been categorized also in terms of active coping (i.e., including both emotion-focused and problem-focused strategies) and passive coping (e.g., denying/avoiding the stressor) [43, 44]. This latter sub-division has been proposed to deepen and further distinguish those emotion-focused strategies that can be more adaptive, such as seeking social support and positive distraction, from those that can be less effective, such as avoiding, denying, or minimizing the stressors [45, 46].
Nevertheless, despite these slight differences in taxonomy, research has reached a clear consensus on the idea that there are no “good” and “bad” strategies in itself, yet the effectiveness of coping strategies needs to be evaluated by using a more complex dynamic approach [34, 35]. In this perspective, whereas the earlier works on coping adopted a trait-based approach, so conceptualizing coping as a rather static and stable set of individuals’ responses, afterward, coping research has evolved, and greater emphasis has been given to situation-based models, which considered stress, health, and coping as dynamic processes [47, 48].
Within the latter perspective, the transactional model of stress and coping represents the most renowned and influential theory [49]. According to this perspective, “the person and the environment are viewed as being in a dynamic, mutually reciprocal, bidirectional relationship” [34]. Stress is determined by the interplay between individual and situational factors, and it derives from two processes, namely the primary appraisal (i.e. individuals’ evaluation of the situation/stressor) and the secondary appraisal (i.e. perceived coping resources available to deal with the situation/stressors) [34, 35, 39, 49].
The authors also suggested that individuals have habitual coping preferences, so that stress and coping processes can be moderately stable across diverse stressful situations [34]. It is therefore clear that the transactional model of stress and coping has promoted research advancements on the possibility of shedding light on the role of individual differences in stress and health/occupational health processes [22, 47].
The person-centred approach
In the same research direction, in the last decades, the person-centred approach has been proposed [15,16,17,18,19,20,21,22,23,24]. From a methodological point of view, this conceptual framework focuses on individuals instead of study variables [50]. Specifically, whereas, on the one hand, the variable-centred approach aims to examine the effects of one/more independent variables on one/more outcomes by applying statistical methodologies such as Regression Analyses and Structural Equation Models, on the other hand, the person-centred approach aims to identify subgroups of people based on the selected variables—and then it aims to compare their characteristics—by applying statistical methodologies such as cluster analysis and latent profile analysis [15,16,17,18,19,20,21,22,23,24, 50].
The application of this approach to coping research has several advantages [22]. It allows researchers to account for the idea that people may use more than one strategy to deal with stress according to the situation, yet people tend to predominantly use the same pool of strategies across several situations. Moreover, this approach allows for capturing unique nuances in coping responses (i.e., people can be classified into distinguished groups even in cases where some coping strategies are adopted to a roughly similar extent by them). Furthermore, by identifying patterns of coping and then exploring differences in perceived stress and health according to the belonging to the emerged patterns, researchers can call into practice the value of the application of a transactional approach for developing more adequate and efficient programs and interventions addressing the specificities/differences among groups of individuals.
Stress, health, and coping among nursing professionals
Nursing is – undoubtedly—a highly demanding and stress-prone profession both physically (e.g., long scheduled hours of work; intense physical duties from patient handling; risk for hazardous exposures) and emotionally (e.g., repeated/prolonged exposure to suffering and death; excessive exposure to requests from patients and their relatives; balancing the needs to providing care and setting boundaries; demands to coordinate – to a greater extent – with the other healthcare professionals) [31, 32].
Research has therefore well-demonstrated the noteworthy high risk for nurses to report stress-related outcomes [5,6,7,8, 33, 51], mainly in terms of anxiety and depression [52,53,54], somatic symptoms [55, 56], emotional exhaustion/compassion fatigue [57,58,59], but also interpersonal-sensitivity, anger/hostility [55, 60]. This high-risk condition can lead to severe consequences for healthcare organizations (e.g., turnover, increased risk of medical errors, lower productivity [61, 62]) and has received renewed attention in recent years – also following the COVID-19 pandemic [24, 54, 62]. Therefore, deepening the dynamics underpinning stress processes in nursing and, in particular, the ways nurses cope with stressful experiences – the latter occurring daily in their work life – is of particular interest and, mainly, it is an urgent need on the agendas worldwide.
However, whereas research in nursing on the effectiveness of single coping strategies provided – by the situation-based nature of coping – mixed and therefore rather inconclusive results in terms of identification of those strategies promoting or hindering nurses’ health conditions [63,64,65,66,67], research on coping profiles would be promising in meeting and responding to the abovementioned need, yet it is still scarce. To the best of our knowledge, only a few studies explored nurses’ patterns of coping [23, 24]. For example, a study conducted in a sample of 1223 Polish nurses [23]—by using statistically valid measures and questions developed by the authors—identified three groups of nurses based on various factors including coping styles, stress, and health, namely: 1. Non-harmonious/organized (i.e. nurses who moderately use emotion-focused strategies and reported moderate stress/higher psychophysical disease); 2. Harmonious (i.e., nurses who mainly use the task-oriented coping style and reported lower levels of stress/psychophysical disease); 3. Non-harmonious/disorganized (i.e., nurses who mainly use emotion-oriented/avoidance coping and reported higher levels of stress/moderate psychophysical disease).
More recently, a study conducted in a sample of 429 Greek nurses has explored coping profiles in association with vicarious post-traumatic growth [24]. Three patterns of coping were identified, namely Active, Avoidant, and Passive profiles. However, this research was conducted during the COVID-19 emergency to explore the ways nurses responded to this unprecedented/unexpected event [24]. Therefore, further studies in the same research direction – yet using validated measurement tools and going beyond the specificities of the pandemic experience—are needed. The present study sought to target this aim.
Objective
This study proposed a research application of the DRIVE-Nurses Model [12,13,14] and adopted the person-centred approach [15,16,17,18,19,20,21,22,23,24] with the aim to target two main objectives: 1. To identify distinguished patterns of coping strategies (Problem-Focused; Seek-Advice; Self-Blame; Wishful-Thinking; Escape/Avoidance) adopted by nurses to deal with stress; 2. To test potential differences between nurses belonging to the different patterns of coping in terms of perceived levels of Demands (i.e., Efforts), Resources (i.e., Rewards, Job Control, Social Support), and Psychopathological Symptoms (i.e., Anxiety, Phobic-Anxiety, Obsessive–Compulsive, Somatization, Depression, Interpersonal-Sensitivity, Hostility, Psychoticism, Paranoid-Ideation). In line with the abovementioned objectives, and considering the research reported above, the following hypotheses have been tested.
-
Hypothesis one (H1)
Nurses can be differentiated based on unique combinations of coping strategies (patterns of coping).
-
Hypothesis two (H2)
Perceived levels of Demands, Resources, and Psychopathological Symptoms reported by nurses will statistically significantly vary according to the emerged patterns of coping.
Material and methods
Sample
This cross-sectional multi-centre study was reported by employing the STROBE Checklist. Participants were nurses recruited between January and August 2023 from Italian Hospitals of the Public Health Service. Chairpersons/Nursing Managers were first contacted to ask for permission to administer a questionnaire to the nursing staff. Afterward, 300 nurses were directly contacted and given all the information about the research objective as well as about the confidentiality of the data collection procedure (i.e., procedure: self-report questionnaires, face-to-face administration by trained psychologists who introduced the project and were always available to respond to any queries/doubt). The study was performed in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards, and it was approved by the Ethical Committee of Psychological Research of the University of Naples Federico II (Protocol Code: 33/2019). Overall, 265 nurses agreed to participate in the research (88.3% Response Rate), they completed the questionnaire in all its sections (there were no missing data) and provided written and verbal informed consent.
Measures
The questionnaire included a section for nurses’ background information, along with valid measures for the assessment of adopted Coping Strategies, perceived Demands, Resources, and Psychological Health Conditions. All the measurement tools were included within the validated Italian version of the DRIVE Questionnaire, in its tailored version for the nursing workforce [12, 13]. The description of the measures considered, along with Cronbach’s α and McDonald’s ω values for the present study, are displayed in Table 1.
Data analysis
All the statistical analyses were carried out by using the software SPSS (Version 29). Preliminarily, Descriptive Analyses and zero-order correlations (Pearson’s Correlations) for all the study variables were carried out. Cohen’s thresholds (r < 0.30 weak/ small correlation; 0.30 < r < 0.50 moderate/medium correlation; r > 0.50 strong/large correlation) were used to interpret the effect sizes [71].
Therefore, in order to test the first research objective and hypothesis (H1), Cluster Analysis was used to identify patterns of coping strategies. Specifically, a non-hierarchical k-means clustering procedure was employed, starting by establishing an initial partition, later calculating the centroid (means) of the clusters, and then determining the Euclidean distances to all the centroids in the clusters. Nurses were grouped and assigned to the nearest cluster, reducing the pooled within-group variance. This procedure was repeated until a stable cluster solution was reached [72]. The use of this iterative approach was recommended to reduce the chances of biases entering the designation of initial cluster seeds, assuring stable clusters once the procedure reached the 2% convergent criterion [72,73,74]. MANOVA and Tukey’s HSD post hoc test were also used to further validate the cluster solution (i.e., the cluster membership was included as the independent variable, and the five coping strategies were included as the dependent variables) [72].
Furthermore, in order to test the second research objective and hypothesis (H2), MANOVAs and Tukey’s HSD post hoc test were used to explore potential differences in perceived levels of Demands, Resources, and Psychological Health conditions according to the coping cluster membership. For Psychological Health conditions, frequencies and percentages of nurses reporting low (below the cut-off point scores) and high (clinically relevant) levels of psychopathological symptoms were also calculated (i.e., the cut-off scores provided by the Italian validation study of the SCL-90-R were used [70]; please, see Table 1) and compared according to the cluster membership by using Cross-tabulations and Chi-Square (χ2) analyses.
Results
Preliminary analyses
Table 2 illustrates the characteristics of study participants. The nursing sample was adequately representative of the workforce by sex and the diverse age range (21–65 years old), and also included nurses working in a wide set of wards.
Descriptive statistics and Pearson’s correlations between all study variables are reported in Table 3.
With respect to coping strategies, firstly, preliminary data revealed statistically significant correlations within the coping construct. According to Cohen’s thresholds, statistically significant positive correlations between Problem-focused and Seek-Advice coping (i.e., between active coping strategies), along with those between Escape/Avoidance and, respectively, Wishful-Thinking and Self-Blame coping (i.e., between passive coping strategies) were found to be strong/large in size. Differently, the statistically significant positive correlations between the active and the passive coping strategies were found to be weak/small or moderate/medium in size. Secondly, statistically significant correlations between coping strategies and, respectively, Demands and Resources (small/weak in size), and Psychological Health Conditions (small/weak to moderate/medium in size) were also found (Table 3).
These preliminary findings suggest the meaningfulness to proceed with the testing of the proposed study hypotheses.
Hypothesis one (H1)—nurses’ patterns of coping
With respect to the first research objective and hypothesis (H1), results from the non-hierarchical k-means cluster analysis fully supported H1 and indicated that a three-cluster solution was the most appropriate for the data, suggesting three stable and meaningful patterns of coping adopted by nurses.
Table 4 illustrates the patterns identified, along with the values corresponding to the centroids of the coping strategies and the frequencies/percentages of the groups.
The first pattern (n = 85, 33.1%) included nurses characterized by the highest adoption of Problem-Focused coping, along with the lowest adoption of Escape/Avoidance and Wishful Thinking coping strategies, and a moderate adoption of Seek-Advice and Self-Blame coping strategies. Therefore, the pattern was labelled as Active/Solution-Oriented.
The second pattern (n = 58, 21.9%) included nurses characterized by the highest adoption of Wishful Thinking, Escape/Avoidance, Self-Blame and Seek-Advice coping strategies, and by relatively high adoption of Problem-Focused coping (displaying the second largest mean scores on this dimension). Therefore, it was labelled as Dysregulated/Emotion-focused.
The third pattern (n = 122, 46.0%) included nurses characterized by the lowest adoption of Problem Focused, Seek-Advice and Self-Blame coping strategies and featured by a moderate adoption of Escape/Avoidance and Wishful Thinking coping strategies. Therefore, it was labelled as Passive/Disengaged.
Findings from MANOVA and Tukey’s HSD post hoc test further supported the three-cluster solution, confirming that the subgroups differed significantly on coping strategies (F(10, 516) = 86.325, p < 0.001; Wilk’s λ = 0.140; partial η2 = 0.626).
Hypothesis two (H2) – nurses’ perceived demands, resources, and psychopathological symptoms by patterns of coping
With respect to the second research objective and hypothesis (H2), overall findings from MANOVA and Tukey’s HSD post hoc test fully supported H2, also highlighting specificities that will be summarized as follows.
Nurses’ perceived demands and resources by patterns of coping
Data revealed that the three subgroups of nurses, varying according to the Patterns of Coping, differed significantly on perceived levels of Demands and Resources (F(8, 518) = 3.574, p < 0.001; Wilk’s λ = 0.898; partial η2 = 0.052). Specifically, nurses belonging to the Dysregulated/Emotion-focused group reported statistically significantly higher levels of perceived Effort and statistically significantly lower levels of perceived Resources (Rewards, Job Control, Social Support) than nurses belonging to the Active/Solution-Oriented group. Moreover, they also reported statistically significantly lower levels of perceived Rewards than nurses belonging to the Passive/Disengaged group. However, nurses belonging to the latter group (Passive/Disengaged) reported statistically significantly lower levels of perceived Job Control and Social Support than nurses belonging to the Active/Solution-Oriented group (Table 5).
Nurses’ psychological health by patterns of coping
Data revealed that the three subgroups of nurses, varying according to the Patterns of Coping, differed significantly on self-reported levels of psychological health conditions (F(18, 508) = 6.296, p < 0.001; Wilk’s λ = 0.668; partial η2 = 0.182). Specifically, nurses belonging to the Dysregulated/Emotion-focused group reported statistically significantly higher levels of all psychopathological symptoms than nurses belonging to the other two groups. Furthermore, nurses belonging to the Passive/Disengaged group reported statistically significantly higher levels of all psychopathological symptoms (except for Phobic-Anxiety) than nurses belonging to the Active/Solution-Oriented group (Table 6).
Moreover, Table 7 illustrates frequencies and percentages of nurses reporting low (below the cut-off point scores) and high (clinically relevant) levels of psychopathological symptoms, which were calculated and compared according to the coping pattern membership. Data revealed that sampled nurses statistically significantly differ in their clinical profiles by the coping patterns groups (Chi-square values ranging from 47.91 to 7.33), with nurses belonging to the Dysregulated/Emotion-focused group reporting the worse profile in terms of psychopathological suffering. Specifically, with respect to nurses belonging to the Dysregulated/Emotion-focused group, data revealed that 48.8% reported clinically relevant levels of Psychoticism, 41.4% of Somatization and Interpersonal Sensitivity, 37.9% of Paranoid Ideation, 34.5% of Phobic-Anxiety, 29.3% of Depression and Obsessive–Compulsive symptoms, 27.6% of Anxiety, and 20.7% of Hostility.
However, despite statistically significantly lower, the clinical profiles of psychopathological suffering featuring the two other groups were also remarkable (Fig. 1). Indeed, with respect to nurses belonging to the Passive/Disengaged group, data revealed that 17.2% reported clinically relevant levels of Paranoid Ideation, 15.6% of Anxiety and Somatization, 14.8% of Interpersonal Sensitivity, 13.9% of Depression, 11.5% of Hostility, 10.7% of Psychoticism, 8.2% of Obsessive–Compulsive symptoms, and 5.7% of Phobic-Anxiety. With respect to nurses belonging to the Active/Solution-Oriented group, data revealed that 9.4% reported clinically relevant levels of Paranoid Ideation, 8.2% of Depression, 7.1% of Somatization, Interpersonal Sensitivity, and Psychoticism, 5.9% of Hostility and Phobic-Anxiety, 4.7% of Obsessive–Compulsive symptoms, and 2.4% of Anxiety.
Discussion
In line with the growing calls for putting individuals at the centre of research/interventions, and responding to the need to develop targeted interventions fostering nurses’ ways to deal with stress and promoting their psychological and occupational health effectively [66, 75], the present study was designed with a twofold objective, namely to identify patterns of coping strategies adopted by nurses to deal with perceived stress, and, therefore, to investigate potential differences in perceived levels of Demands, Resources, and Psychopathological Symptoms reported by nurses belonging to the different patterns that emerged.
Concerning the first research objective, preliminary data from correlation analyses aligned with the research that adopted the coping taxonomy distinguishing active and passive coping strategies [43, 44] and provided initial evidence supporting our first hypothesis (H1), namely that nurses can be differentiated based on unique combinations of coping strategies. From this perspective, findings from cluster analysis fully supported H1 and, specifically, nurses were grouped into three distinguished categories according to the ways they deal with work-related stress, which were labelled as Active/Solution-Oriented, Passive/Disengaged, and Dysregulated/Emotion-focused. Somewhat in line with previous research on coping profiles [23, 24], the first two out of three clusters roughly reflected the polarization activity-passivity, while a middle ground cluster (i.e., Dysregulated/Emotion-focused) was featured by the prominent recourse by nurses to emotion-focused strategies.
However, findings should be discussed by also considering the second research objective/hypothesis (H2) (i.e., differences in perceived Demands, Resources, and Psychopathological Symptoms according to the emerged patterns of coping), so achieving a greater understanding of the conceptual and statistically significant differences featuring these three groups. Specifically, the Active/Solution-Oriented group included nurses who share a higher degree of activity and engagement (i.e., pronounced recourse to problem-solving/ lower tendency to rely on passive strategies) and, at the same time, they seem to display also a tendency to deal with emotional aspects of stressful situations by personally taking charge of the events they may encounter in everyday working life (i.e., moderate – but not high – recourse to self-blame strategies). It is possible to hypothesize that this latter tendency to feel guilt/blame themselves can be linked to their pronounced recourse to active strategies. Indeed, self-blame is indirectly related to perceived control [76], so that people who frequently self-blame are more likely to believe they have greater control over situations. From this perspective, when considering the data on differences in Demands/Resources (H2), findings showed that nurses belonging to this group perceived not only lower levels of effort but also higher levels of all resources—including job control—so further endorsing the hypothesized link between self-blame and control. This should be carefully considered in light of our findings on their psychological health conditions. Indeed, although nurses belonging to Active/Solution Oriented group reported a better and more adjusted psychological profile, they still reported a noteworthy psychopathological risk, mainly in terms of symptoms of paranoid ideation (i.e., distrustful thoughts/behaviours and fear of loss of autonomy), depression, and somatization.
From this perspective, the nursing work—in its nature (e.g., being daily at the forefront of relationships with ill and/or dying patients and with the suffering of the patient’s relatives) may collide with the relevant sense of agency and control featuring nurses belonging to this group, since it implicitly requires nurses to deal with the idea that despite every "action" and "task" has been conducted adequately yet still something can go wrong. This can potentially elicit feelings of helplessness, frustration, and guilt. Therefore, despite the high sense of control/agency may represent the key resource driving nurses’ continuous search for solutions, yet it should be carefully addressed in order to prevent it from becoming a double-edged sword harming their wellbeing.
However, overall, data aligned with previous research [23, 24] by suggesting that nurses belonging to the Active/Solution Oriented group are at a lower risk of occupational stress and psychological suffering. Also, not only do they resort to advice-seeking strategies fairly frequently, but they also seem to perceive an adequate payback (i.e. in their work experience, support is not only sought but it is also found), so potentially feeding reciprocal positive individual-environment transactions.
On the opposite pole, the Passive/Disengaged group (that is the largest group) included nurses characterized by a certain degree of disengagement and low activation. It is possible to hypothesize that nurses belonging to this group are the least motivated and engaged in their work, yet it is also possible to trace back and link this profile to high emotional burden, compassion fatigue, and defensive responses [57,58,59]. In other words, nurses belonging to this group may feel exhausted and feel such a lack of control over events that they may have responded by defending themselves, thus becoming cynical, fatalistic, detached, and avoidant [77].
The latter hypothesis could be supported if one examines findings from testing H2. Indeed, nurses belonging to this group perceived lower levels of resources (control/support) and they also exhibited a significantly higher risk (in most cases doubled compared to the Active/Solution oriented group) of reporting clinically relevant levels of psychopathological symptoms – mainly in terms of paranoid-ideation (whose symptomatology goes from mild suspiciousness/distrust to full persecutory delusions [78, 79]), but also anxiety, somatization, interpersonal sensitivity, and depression.
From this perspective, interventions targeting nurses belonging to the Passive/Disengaged group should carefully consider their significant risk of being detached, self-deloused, and depersonalized as a consequence of extremely high levels of stress/perceived low control and support. Indeed, we need to also take into account the growing body of research which have linked paranoid thinking/behaviours to work-related stress, burnout, and depression [80,81,82,83], which seems to align with our findings.
Finally, the Dysregulated/Emotion-focused group included nurses who predominantly attempted to manage emotions to cope with stressful events/situations and who were at very high risk for both perceived work-related stress and psychological suffering. In this regard, findings "portray" those nurses who appear to be highly sensitive, reactive – rather than active – impulsive and disorganized.
Given that nursing/caring is an extremely emotionally demanding profession [84, 85], nurses belonging to this latter group require particular attention when defining tailored support interventions. Indeed, their predominant tendency to minimize or deny the stressors also having positive unrealistic expectations which are often far from reality (i.e., extremely high use of wishful thinking coping), to detach when instead hyper-engaged and hyper-involved (i.e., higher imbalance between perceived efforts and rewards, extremely high use of avoidance coping), to recur to self-criticism along with perceiving lack of control over situations (i.e., lower control and higher use of self-blame coping), and to try to seek-advice along with perceiving – at the same time – lack of support at work (i.e., low perceived support with high recourse to seek-advice coping), but also their moderate recourse to problem-solving in such complex vicious circle of unfulfilling individual-environment transactions, expose them to extremely high risk.
From this perspective, about one-half of nurses belonging to Dysregulated/Emotion-focused group displayed clinical symptoms referable to psychoticism (i.e., this latter needs to be considered along a continuum from mild interpersonal alienation and withdrawal to severe psychosis with symptoms such as hallucinations and thought control), about 40% reported clinically relevant symptoms of somatization, interpersonal sensitivity, and paranoid ideation, about 30% anxious and depressive symptomatology, and over 20% hostility. These findings – which fairly aligned with research linking stress/work-related stress, emotional dysregulation, interpersonal sensitivity, and psychotic symptoms [86, 87], and with recent evidence warning about a vicious circle of stress, conflict, individual and interpersonal suffering among nursing professionals [60]—highlighted the urgent need to develop interventions promoting awareness, adjustment processes and emotion regulation strategies among nursing professionals.
Research implications
Overall, the findings can have several theoretical and practical implications. Indeed, results provided further evidence endorsing the meaningful of applying the DRIVE Model framework and the person-centred approach for deepening nurses’ subjectivity and achieving a greater understanding of stress and health processes among nursing professionals.
Furthermore, researchers, practitioners, and healthcare managers could benefit from this study not only for developing future research but also for implementing more adequate, efficient, and tailored evidence-based programs/interventions. From this perspective, three distinct groups of nurses were identified, for whom specific interventions need to be designed and implemented. This will also ultimately provide benefits for the whole healthcare staff and the healthcare organization and could foster the welfare of the society (i.e., promoting better work engagement, high standards of quality of care, better relations within/outside the wards, and higher performance).
Specifically, for nurses belonging to the Active/Solution Oriented group, who appear to handle stress more adequately and were at lower risk of stress and psychological discomfort, interventions can be focused on supporting the active strategies they already adopt and on continuously preserving and enhancing those key work resources they actually need, namely rewards, control, and support (i.e., so keeping fostering positive exchanges with the environment). This is in line with research highlighting the utmost need to implement evidence-based interventions for stress management within the healthcare environments [9, 10, 75] along with studies on nurses’ patterns of coping suggesting the effectiveness of promoting the use of active/problem-solving strategies among nurses to prevent psychological disease and enhance their wellbeing [23, 24]. Yet, findings from the present study also suggested that training/support programs should also consider the need to critically reflect and foster awareness of nurses’ need for control (and their tendency to blame) to further reduce their risk and promote their psychological and occupational health.
For nurses belonging to the Passive/Disengaged group, who may be either demotivated or disillusioned and highly defended and who were at moderate/intermediate – but still considerable – risk for psychological suffering and occupational stress, key resources within the working environment (i.e., control/autonomy and support) should be strengthened and, at the same time, interventions should be implemented to foster emotional regulation strategies that enable them to be/be again engaged in their care work and to find/re-discover the reasons for their professional choice. This is in line with recent research underlining the need to develop interventions aiming at reducing avoidance and promoting engagement among nurses [88].
For nurses belonging to the Dysregulated/Emotion-focused group, who are at extreme psychopathological risk and in great suffering at work, timely interventions and paths of psychological support must be proposed and offered in the work contexts. Considering research demonstrating that training/programs focused on emotion regulation can be effective in reducing stress and promoting wellbeing among nurses [89, 90], a particular focus must be given to the management of emotions, i.e. on the possibility of handling the different situations that feature the everyday life of nurses, who have chosen a very delicate and emotionally charged profession. This is by promoting the ability to recognize their ways to appraise situations, tolerate and manage stress and frustration, and adjust to the (difficult) daily reality.
Limitations and conclusions
Despite the abovementioned results and implications, some limitations need to be underlined. Firstly, the sample size is relatively small and restricted to the Italian public healthcare context, thus limiting the generalizability of research results. Indeed, despite the sample being rather representative by sex, age, and wards, future research could be conducted with a larger sample, and it would be interesting to also investigate these profiles across genders, various generations, specific wards, along with different cultures and nations to explore possible differences and commonalities. Secondly, the cross-sectional design limits the possibility of determining the stability of the identified patterns over time, and future studies could be developed with a longitudinal design to verify whether the identified patterns of coping can be confirmed across the different life and career stages. Also, a pre-to-post interventional study could be developed to test the effectiveness of tailored support programs/interventions aiming at promoting awareness of own coping responses, emotional regulation, and adjustment processes among nurses. Thirdly, despite the application of the DRIVE Model-Nurses Version allowing the investigation of a wide range of dimensions, our findings have raised the interest to examine further individual (e.g., personality functioning) and situational characteristics (e.g., type of stressful situations) according to these profiles. This – indeed – would allow researchers/practitioners to achieve an even deeper understanding of stress and health processes among nursing professionals.
Notwithstanding the abovementioned limitations, in conclusion, the study findings captured three unique nuances in coping responses by nurses and provided evidence supporting differences in stress and health processes based on them. Fostering nurses’ awareness of their latent coping patterns and supporting active approaches and adequate emotional regulation strategies for stress management should represent a key goal when defining interventions promoting nurses’ health within and beyond the healthcare settings.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due to the terms of consent to which the participants agreed but available from the corresponding author on reasonable request.
Abbreviations
- DRIVE Model:
-
Demands-Resources and Individual Effects Model
References
WHO. Health workers. 2020. Available Online: https://www.who.int/news-room/fact-sheets/detail/occupational-health--health-workers . Accessed on 14 May 2024.
WHO. State of the World’s Nursing 2020, Investing in Education, Jobs and Leadership. 2020. Available Online: https://www.who.int/publications/i/item/9789240003279 . Accessed on 13 May 2024.
Della Bella V, Fiorini J, Gioiello G, Zaghini F, Sili A. Towards a new conceptual model for nurses’ organizational well-being: an integrative review. J Nurs Manag. 2022;30(7):2833–44.
Xiao Q, Cooke FL, Chen L. Nurses’ well-being and implications for human resource management: a systematic literature review. Int J Manag Rev. 2022;24(4):599–624.
Birgit E, Gunnevi S, Ann Ö. Work experiences among nurses and physicians in the beginning of their professional careers–analyses using the effort–reward imbalance model. Scand J Caring Sci. 2013;27(1):36–43.
Schneider A, Hering C, Peppler L, Schenk L. Effort-reward imbalance and its association with sociocultural diversity factors at work: findings from a cross-sectional survey among physicians and nurses in Germany. Int Arch Occup Environ Health. 2023;96(4):537–49.
Papazian L, Hraiech S, Loundou A, Herridge MS, Boyer L. High-level burnout in physicians and nurses working in adult ICUs: a systematic review and meta-analysis. Intensive Care Med. 2023;49(4):387–400.
Salyers MP, Bonfils KA, Luther L, Firmin RL, White DA, Adams EL, Rollins AL. The relationship between professional burnout and quality and safety in healthcare: a meta-analysis. J Gen Intern Med. 2017;32:475–82.
Alkhawaldeh JF, Soh KL, Mukhtar FB, Ooi CP. Effectiveness of stress management interventional programme on occupational stress for nurses: a systematic review. J Nurs Manag. 2020;28(2):209–20.
Alkhawaldeh JF, Soh KL, Mukhtar FB, Peng OC, Anshasi HA. Stress management interventions for intensive and critical care nurses: a systematic review. Nurs Crit Care. 2020;25(2):84–92.
De la Fuente-Solana EI, Pradas-Hernández L, Ramiro-Salmerón A, Suleiman-Martos N, Gómez-Urquiza JL, Albendín-García L, Cañadas-De la Fuente GA. Burnout syndrome in paediatric oncology nurses: a systematic review and meta-analysis. Healthcare. 2020;29(8):309.
Vallone F, Smith AP, Zurlo MC. Work-related stress and wellbeing among nurses: testing a multi-dimensional model. Jpn J Nurs Sci. 2020;17(4):e12360.
Zurlo MC, Vallone F, Smith AP. Effects of individual differences and job characteristics on the psychological health of Italian nurses. Eur J Psychol. 2018;14(1):159.
Mark G, Smith AP. Occupational stress, job characteristics, coping, and the mental health of nurses. Brit J Health Psychol. 2012;17(3):505–21.
Woo SE, Jebb AT, Tay L, Parrigon S. Putting the “person” in the center: review and synthesis of person-centered approaches and methods in organizational science. Organ Res Methods. 2018;21(4):814–45.
Zurlo MC, Vallone F, Dell’Aquila E, Marocco D. Teachers’ patterns of management of conflicts with students: a study in five European countries. Eur J Psychol. 2020;16(1):112.
Ahola K, Hakanen J, Perhoniemi R, Mutanen P. Relationship between burnout and depressive symptoms: a study using the person-centred approach. Burn Res. 2014;1(1):29–37.
Yao X, Wen S, Song Z, Wang J, Shen Y, Huang X. Work–family conflict categories and support strategies for married female nurses: a latent profile analysis. Front Public Health. 2024;12:1324147.
Mauno S, Mäkikangas A, Kinnunen U. A longitudinal person-centred approach to the job demands-control model. Eur J Work Organ Psychol. 2016;25(6):914–27.
Aguayo-Estremera R, Membrive-Jiménez MJ, Albendín-García L, Gómez-Urquiza JL, Romero-Bejar JL, De la Fuente-Solana EI, Cañadas GR. Analyzing latent burnout profiles in a sample of Spanish nursing and psychology undergraduates. Healthcare. 2024;12(4):438.
Nagy L, Balázs K. Typical coping patterns: a person-centered approach to coping. New Ideas Psychol. 2023;70:101023.
Somers MJ, Casal J. Patterns of coping with work-related stress: a person-centred analysis with text data. Stress Health. 2021;37(2):223–31.
Iwanowicz-Palus G, Mróz M, Kowalczuk K, Szlendak B, Bień A, Cybulski M. Nurses coping with stressful situations—a cross-sectional study. IJERP. 2022;19(17):10924.
Kalaitzaki A, Theodoratou M, Tsouvelas G, Tamiolaki A, Konstantakopoulos G. Coping profiles and their association with vicarious post‐traumatic growth among nurses during the three waves of the COVID‐19 pandemic. J Clin Nurs. 2024; Advance online publication. https://doi.org/10.1111/jocn.16988.
Jourdain G, Chênevert D. Job demands–resources, burnout and intention to leave the nursing profession: a questionnaire survey. Int J Nurs Stud. 2010;47(6):709–22.
Enns V, Currie S, Wang J. Professional autonomy and work setting as contributing factors to depression and absenteeism in Canadian nurses. Nurs Outlook. 2015;63(3):269–77.
Wang X, Liu L, Zou F, Hao J, Wu H. Associations of occupational stressors, perceived organizational support, and psychological capital with work engagement among Chinese female nurses. BioMed Res Int. 2017;2017(1):5284628.
Siegrist J. Adverse health effects of high-effort/low-reward conditions. J Occup Health Psychol. 1996;1(1):27.
Karasek R, Brisson C, Kawakami N, Houtman I, Bongers P, Amick B. The Job Content Questionnaire (JCQ): an instrument for internationally comparative assessments of psychosocial job characteristics. J Occup Health Psychol. 1998;3(4):322.
Williams GM, Smith AP. A practical method of predicting wellbeing at work: the Wellbeing Process Tool. Adv Soc Sci Res J. 2018;5(2):86–93.
Rink LC, Oyesanya TO, Adair KC, Humphreys JC, Silva SG, Sexton JB. Stressors among healthcare workers: a summative content analysis. Glob Qual Nurs Res. 2023;10:23333936231161130.
National Institute for Occupational Safety and Health [NIOSH]. Healthcare Workers and Work Stress. Available Online at: https://www.cdc.gov/niosh/topics/healthcare/workstress.html#:~:text=Work%20in%20healthcare%20often%20involves,patient%2C%20family%20members%2C%20and%20employers. Accessed 14 May 2024.
Almeida D, Figueiredo AR, Lucas P. Nurses’ well-being at work in a hospital setting: a scoping review. Healthcare. 2024;12(2):173.
Folkman S, Lazarus RS, Gruen RJ, DeLongis A. Appraisal, coping, health status, and psychological symptoms. J Pers Soc Psychol. 1986;50(3):571.
Folkman S, Moskowitz JT. Coping: pitfalls and promise. Annu Rev Psychol. 2004;4(55):745–74.
Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: a theoretically based approach. J Pers Soc Psychol. 1989;56(2):267.
Carver CS. You want to measure coping but your protocol’too long: consider the brief cope. Int J Behav Med. 1997;4(1):92–100.
Galvin J, Evans MS, Nelson K, Richards G, Mavritsaki E, Giovazolias T, Koutra K, Mellor B, Zurlo MC, Smith AP, Vallone F. Technostress, coping, and anxious and depressive symptomatology in university students during the COVID-19 pandemic. Eur J Psychol. 2022;18(3):302.
Lazarus RS. Coping theory and research: past, present, and future. PM. 1993;55(3):234–47.
Muller L, Spitz E. Multidimensional assessment of coping: validation of the Brief COPE among French population. Encéphale. 2003;29(6):507–18.
Vitaliano PP, Russo J, Carr JE, Maiuro RD, Becker J. The ways of coping checklist: revision and psychometric properties. Multivar Behav Res. 1985;20(1):3–26.
Zeidner M, Endler NS, editors. Handbook of coping: Theory, research, applications (vol.195). John Wiley & Sons; 1995.
Brown GK, Nicassio PM. Development of a questionnaire for the assessment of active and passive coping strategies in chronic pain patients. Pain. 1987;31(1):53–64.
Perez-Tejada J, BSBIO LG, Ainitze Labaka RN, Oscar Vegas BS, Gómez-Lazaro E, Amaia Arregi BS. Active and passive coping strategies. Clin J Oncol Nurs. 2019;23(6):583–90.
Waugh CE, Shing EZ, Furr RM. Not all disengagement coping strategies are created equal: positive distraction, but not avoidance, can be an adaptive coping strategy for chronic life stressors. Anxiety Stress Coping. 2020;33(5):511–29.
Zurlo MC, Cattaneo Della Volta MF, Vallone F. Re-examining the role of coping strategies in the associations between infertility-related stress dimensions and state-anxiety: implications for clinical interventions with infertile couples. Front Psychol. 2020;11:614887.
Dewe PJ, O’Driscoll MP, Cooper C. Coping with work stress: a review and critique. 2010.
Greenaway KH, Louis WR, Parker SL, Kalokerinos EK, Smith JR, Terry DJ. Measures of coping for psychological well-being. In: Boyle GJ, Saklofske DH, Matthews G, editors. Measures of personality and social psychological constructs. Academic Press; 2015. p. 322–351.
Lazarus RS, Folkman S. Stress, appraisal, and coping. Springer publishing company; 1984.
Meyer JP, Morin AJ. A person-centered approach to commitment research: Theory, research, and methodology. J Organ Behav. 2016;37(4):584–612.
Dilmaghani RB, Armoon B, Moghaddam LF. Work-family conflict and the professional quality of life and their sociodemographic characteristics among nurses: a cross-sectional study in Tehran. Iran BMC Nurs. 2022;21(1):289.
Boya FÖ, Demiral Y, Ergör A, Akvardar Y, De Witte H. Effects of perceived job insecurity on perceived anxiety and depression in nurses. Ind Health. 2008;46(6):613–9.
Maharaj S, Lees T, Lal S. Prevalence and risk factors of depression, anxiety, and stress in a cohort of Australian nurses. IJERPH. 2019;16(1):61.
Sahebi A, Nejati-Zarnaqi B, Moayedi S, Yousefi K, Torres M, Golitaleb M. The prevalence of anxiety and depression among healthcare workers during the COVID-19 pandemic: an umbrella review of meta-analyses. Prog Neuropharmacol Biol Psychiatry. 2021;107:110247.
Korkmaz EK, Telli S, Kadioglu H, Karaca S. Alexithymia in nurses and its relationship with burnout, anger, and somatization. J. Psychiatric Nurs/Psikiyatri Hemsireleri Dernegi. 2020;11(4):284–91.
Zurlo MC, Vallone F, Smith AP. Work–family conflict and psychophysical health conditions of nurses: gender differences and moderating variables. Jpn J Nurs Sci. 2020;17(3):e12324.
Al Barmawi MA, Subih M, Salameh O, Sayyah Yousef Sayyah N, Shoqirat N, Abdel‐Azeez Eid Abu Jebbeh R. Coping strategies as moderating factors to compassion fatigue among critical care nurses. Brain Behav. 2019;9(4):e01264.
Upton KV. An investigation into compassion fatigue and self-compassion in acute medical care hospital nurses: a mixed methods study. J Compassionate health care. 2018;5(1):1–27.
Ondrejková N, Halamová J. Qualitative analysis of compassion fatigue and coping strategies among nurses. Int J Nurs Sci. 2022;9(4):467–80.
Vallone F, Zurlo MC. Stress, interpersonal and inter-role conflicts, and psychological health conditions among nurses: vicious and virtuous circles within and beyond the wards. BMC Psychol. 2024;12(1):197.
Michie S, Williams S. Reducing work related psychological ill health and sickness absence: a systematic literature review. Occup Environ Med. 2003;60(1):3–9.
Nagel C, Nilsson K. Nurses’ work-related mental health in 2017 and 2020—a comparative follow-up study before and during the COVID-19 pandemic. IJERPH. 2022;19(23):15569.
Betke K, Basińska MA, Andruszkiewicz A. Sense of coherence and strategies for coping with stress among nurses. BMC Nurs. 2021;20(1):107.
Lim J, Bogossian F, Ahern K. Stress and coping in Australian nurses: a systematic review. Int Nurs Rev. 2010;57(1):22–31.
Martínez-Zaragoza F, Benavides-Gil G, Rovira T, Martin-del-Rio B, Edo S, García-Sierra R, Solanes-Puchol Á, Fernández-Castro J. When and how do hospital nurses cope with daily stressors? A multilevel study. PLoS One. 2020;15(11):e0240725.
Alkhawaldeh JF, Soh KL, Mukhtar F, Peng OC, Alkhawaldeh HM, Al-Amer R, Anshasi HA. Stress management training program for stress reduction and coping improvement in public health nurses: a randomized controlled trial. J Adv Nurs. 2020;76(11):3123–35.
Yeşil A, Polat Ş. Investigation of psychological factors related to compassion fatigue, burnout, and compassion satisfaction among nurses. BMC Nursing. 2023;22(1):12.
Zurlo MC, Pes D, Siegrist J. Validity and reliability of the effort-reward imbalance questionnaire in a sample of 673 Italian teachers. Int Arch Occup Environ Health. 2010;83:665–74.
Derogatis LR. Symptom checklist 90–R: Administration, scoring, and procedures manual (3rd ed.). NCS Pearson; 1994.
Prunas A, Sarno I, Preti E, Madeddu F. SCL-90-R. Symptom Checklist-90-R. Giunti; 2010.
Cohen J. Statistical power analysis for the behavioral sciences (2nd ed.). Erlbaum; 1988.
Aldenderfer MS, Blashfield RK. Cluster analysis: Quantitative applications in the social science. Sage; 1984.
Hair JF, Anderson RE, Tatham RL, Black WC. Multivariate data analysis. Prentice-Hall; 1998.
Lee CK, Lee YK, Wicks BE. Segmentation of festival motivation by nationality and satisfaction. Tour Manag. 2004;25(1):61–70.
Velana M, Rinkenauer G. Individual-level interventions for decreasing job-related stress and enhancing coping strategies among nurses: a systematic review. Front Psychol. 2021;19(12):708696.
Hooker SA. Self-Blame. In: Gellman MD, Turner JR, editors. Encyclopedia of Behavioral Medicine. Springer; 2013. p. 1975.
Austin W, Goble E, Leier B, Byrne P. Compassion fatigue: The experience of nurses. Ethics SocWelfare. 2009;3(2):195–214.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th edn. American Psychiatric Publishing; 2013.
Green CE, Freeman D, Kuipers E, et al. Measuring ideas of persecution and social reference: the Green et al. Paranoid Thought Scales (GPTS). Psychol Med. 2008;38:101–11.
Freeman D, McManus S, Brugha T, Meltzer H, Jenkins R, Bebbington P. Concomitants of paranoia in the general population. Psychol Med. 2011;41:923–36.
Kesting ML, Bredenpohl M, Klenke J, Westermann S, Lincoln TM. The impact of social stress on self-esteem and paranoid ideation. J Behav Ther Exp Psychiatry. 2013;44:122–8.
Freudenberger HJ. Staff burnout. J Soc Issues. 1974;30:159–65.
Bianchi R, Janin L. Burnout, depression and paranoid ideation: a cluster-analytic study. Occup Med. 2019;69(1):35–8.
Kalichman SC, Gueritault-Chalvin V, Demi A. Sources of occupational stress and coping strategies among nurses working in AIDS care. JANAC. 2000;11(3):31–7.
Ha DG, Sung MH. Impact of job stress, coping behavior, hardiness on burnout in nurses in the emergency department. Korean J Occup Health Nurs. 2018;27(4):215–23.
Liu J, Chan TC, Chong SA, Subramaniam M, Mahendran R. Impact of emotion dysregulation and cognitive insight on psychotic and depressive symptoms during the early course of schizophrenia spectrum disorders. Early Interv Psychia. 2020;14(6):691–7.
Lincoln TM, Hartmann M, Köther U, Moritz S. Dealing with feeling: specific emotion regulation skills predict responses to stress in psychosis. Psychiatry Res. 2015;228(2):216–22.
Frögéli E, Rudman A, Ljótsson B, Gustavsson P. Preventing stress-related ill health among newly registered nurses by supporting engagement in proactive behaviors: development and feasibility testing of a behavior change intervention. Pilot Feasibility Stud. 2018;4:1–4.
Saedpanah D, Salehi S, Moghaddam LF. The effect of emotion regulation training on occupational stress of critical care nurses. JCDR. 2016;10(12):VC01.
Foji S, Vejdani M, Salehiniya H, Khosrorad R. The effect of emotional intelligence training on general health promotion among nurse. J Educ Health Promot. 2020;9:4.
Acknowledgements
The authors are thankful to the chairpersons of Healthcare Services and to all nurses who participated in this study.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
F.V. prepared the concept and design, collected data, performed the statistical analysis, interpretated data, and drafted the manuscript; M.F.C.D.V. contributed to interpretation of data, the writing review & editing; M.C.Z. contributed to the concept and data interpretation, reviewed, and supervised the work. All authors have read and agreed to the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was performed in accordance with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards, and it was approved by the Ethics Committee of Psychological Research of University of Naples Federico II (Protocol Number: 33/2019). Verbal and written informed consent was obtained from each participant prior to participating in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Vallone, F., Cattaneo Della Volta, M.F. & Zurlo, M.C. Stress dimensions, patterns of coping, and psychopathological risk among nurses: a person-centred approach. BMC Nurs 23, 569 (2024). https://doi.org/10.1186/s12912-024-02250-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12912-024-02250-y