Abstract
Background
Berberine (BBR) is a traditional antimicrobial herbal medicine. Recently, BBR has gained popularity as a supplement to lower blood lipids, cholesterol and glucose. Bile acids (BAs) are known to regulate blood levels of triglycerides, cholesterol, glucose and energy homeostasis, and gut flora play an important role in BA metabolism. However, whether BBR alters BAs metabolism or dose-response effect of BBR on gut flora is unknown.
Methods
In this study, the effects of various doses of BBR on the concentrations of BAs in liver and serum of male C57BL/6 mice were determined by UPLC-MS/MS, and the expression of BA-related genes, as well as the amount of 32 of the most abundant gut bacterial species in the terminal ileum and large intestine of male C57BL/6 mice were quantified by RT-PCR and Quantigene 2.0 Reagent System, respectively.
Results
Unconjugated BAs and total BAs were significantly altered by BBR in serum but not in liver. Increased primary BAs (βMCA, TβMCA and TUDCA) and decreased secondary BAs (DCA, LCA and the T-conjugates) were observed in livers and serum of mice fed BBR. The expression of BA-synthetic enzymes (Cyp7a1 and 8b1) and uptake transporter (Ntcp) increased 39-400 % in liver of mice fed the higher doses of BBR, whereas nuclear receptors and efflux transporters were not markedly altered. In addition, Bacteroides were enriched in the terminal ileum and large bowel of mice treated with BBR.
Conclusion
The present study indicated that various doses of BBR have effects on BA metabolism and related genes as well as intestinal flora, which provides insight into many pathways of BBR effects.
Similar content being viewed by others
Background
Bile acids (BAs) are important natural detergents that form micelles to facilitate the absorption of dietary fat and lipid soluble vitamins from the gastrointestinal tract. BAs are also the driving force for bile formation, and can reduce bacteria in the biliary tract and intestine [1]. In addition, BAs are important metabolic and inflammatory signaling molecules as they regulate lipid- and energy-related nuclear hormone receptors, such as farnesoid-X-receptor (FXR) and transmembrane G-protein-coupled receptor 5 (TGR5 or GPBAR1) [2, 3].
Primary BAs are synthesized in the liver and are converted to secondary BAs by bacteria in the intestine. Secondary BAs are more toxic than primary BAs, possibly because of their higher hydrophobicity [4]. For instance, deoxycholic acid (DCA) and lithocholic acid (LCA), which are secondary BAs produced by bacteria, are thought to play roles in colorectal cancer, liver cancer, and cholesterol gallstones [5–8].
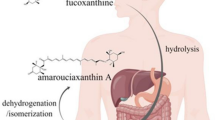
BAs are synthesized and circulate in the liver and intestine, which is orchestrated by feedback loops [6]. The liver synthesizes primary BAs, namely cholic acid (CA) and chenodeoxycholic acid (CDCA) from cholesterol. In rodents, CDCA is further hydroxylated to alpha-muricholic acid (αMCA), and then epimerized to beta-muricholic acid (βMCA). The rate-limiting enzyme of primary BA synthesis is Cytochrome P450 (Cyp) 7a1 (cholesterol 7α-hydroxylase), which initiates the classic synthetic pathway, whereas Cyp27a1 and Cyp7b1 are important in the alternative route of BA synthesis [9]. Primary BAs are conjugated with glycine (predominant in human) or taurine (predominant in rodent) in the liver. A portion of the BAs are directly effluxed into the blood by the efflux transporters on the basolateral membrane of hepatocytes, including multiple drug resistance-related protein (Mrp) 3, Mrp4 and organic solute transporter (Ost) β. However, most BAs in the liver are pumped into the biliary tree by the efflux transporters on the canalicular membrane of hepatocytes, mainly the bile salt export pump (Bsep). The BAs are stored in the gallbladder to be further concentrated [10], and thereafter delivered into the intestine to promote emulsification of lipids and fat soluble vitamins [11]. In the intestine, primary BAs are deconjugated, dehydroxylated at C-7, epimerized, and oxidized to form secondary BAs in the terminal ileum and large bowel by anaerobic bacteria [12]. In the ileum, through a BA-activated FXR-dependent pathway, fibroblast growth factor 15 (FGF15) is secreted into the blood, and interacts with the fibroblast growth factor receptor 4 (Fgfr4) in the hepatocytes to inhibit BA synthesis [13, 14]. In the liver, BAs activate FXR, which induce the expression of small heterodimer partner (SHP) that represses liver receptor homolog-1 (LRH-1), leading to decreased transcription of Cyp7a1 [15]. Thus BAs regulate their own synthesis by FXR-Fgf15 in the intestine and FXR-SHP in the liver. CDCA, TCDCA, TCA, TDCA, DCA and CA are potent activators of FXR activity [16, 17], whereas TβMCA and UDCA are natural antagonists of FXR [14, 18]. However, the entire regulatory mechanism of BA synthesis is not fully understood.
About 5 % of secreted BAs in the gut are excreted into feces and is the most important eliminating channel of cholesterol from the body [19], whereas, the remaining 95 % are reclaimed at the terminal ileum by the apical sodium-dependent BA uptake transporter (Asbt) into the ileocytes, followed by Ostα/β active transport to the portal blood. The BAs are then taken up into hepatocytes by the sodium taurocholate cotransporting polypeptide (Ntcp: uptake of conjugated BAs) and the organic anion transporting peptide 1b2 (Oatp1b2: uptake of unconjugated BAs) [20]. This entire process is termed the enterohepatic circulation (EHC) [10] (Fig. 1).
Schematic diagram of BAs EHC. This is the recirculation of BAs between the intestine and the liver. BAs are synthesized in the hepatocyte (from cholesterol) by Cyp7a1, 27a1, 7b1 and 8b1, released into bile, transformed by the gut microbiota, reabsorbed in the small intestine, and returned to the liver to be recycled. The major genes involved in the EHC are shown
Berberine (BBR) is a quaternary ammonium salt from the protoberberine group of isoquinoline alkaloids, and it is traditionally used for gastrointestinal inflammation in Chinese and native American medicines [21, 22]. Recently, because its potential cytostatic, antiproliferative, and antioxidative activities, the raw herb of BBR was ranked as the sixth most commonly used herbal supplement for children in America [23]. BBR has been reported to have inhibitory effects against Staphylococcus aureus, Plasmodium falciparum, cholera, amoebiasis, and viruses, but also affects the gut microflora including Bifidobacterium longum, Bifidobacterium bifidum, Clostridium perfringens, and Clostridium paraputrificum [22, 24, 25]. It has been reported that modulation of the gut microbiota by BBR may contribute to its antidiabetic effect [26, 27]. BBR is also becoming widely used as a supplement to prevent hypercholesterolemia for decreasing cholesterol absorption from the intestine and stimulating BA synthesis [28, 29].
Antibiotics affect BA metabolism theoretically due to their ability to alter intestinal bacteria, which play a fundamental role not only on the generation of secondary BAs, but also as a modulator of hepatic BA synthesis [14, 30]. BBR is also proven to stimulate bile secretion [31, 32], however, it is not clear if and how BBR affects BA concentrations, transporters involved in the EHC of BAs, and the abundance of individual gut microbiota.
To systematically explore the impact of different doses of BBR on BA profiles in liver and serum and the potential mechanism for these alterations, in the present study, BBR were given to mice, and concentrations of total BAs, individual BAs, and genes involved in BA homeostasis, as well as bacteria in the terminal ileum and large intestine were quantified. Various doses of BBR increased primary BAs, whereas it decreased secondary BAs, and has effects on BA metabolism and related genes as well as intestinal flora, which provides insight into many pathways of BBR effects.
Methods
Ethics statement
Mice were housed according to guidelines of the Institutional Animal Care and Use Committee at the University of Kansas Medical Center. Procedures were carried out in compliance with standards for the use of laboratory animals. Animal experiments performed in this manuscript were approved by the Institutional Animal Care and Use Committee at the University of Kansas Medical Center.
Animals and treatments
Seven-week-old male C57BL/6 mice were purchased from Charles River Laboratories, Inc. (Wilmington, MA), housed according to the American Animal Association Laboratory Animal Care guidance under a standard 12-h dark-light cycle and humidity-controlled environment with a room temperature at approximately 25 °C, and acclimated for at least 1 week before treatment. Mice were arbitrarily divided into six groups and had access to Laboratory Rodent Chow 8604 (Harlan, Madison, WI) and drinking water ad libitum.
Sample collection
BBR (B3251) was purchased from Sigma-Aldrich (USA). Six doses (0, 3, 10, 30, 100, 300 mg/kg) of BBR were given to mice by gavage (4-6 for each group) for 2 weeks after a pilot study. Control animals received the vehicle (saline; 0 mg/kg) only. Mice were anesthetized, blood was collected by orbital bleeding, and serum was obtained by centrifuging blood at 6,000 g for 15 min. Livers with gallbladders removed were harvested from the same animals, washed, frozen in liquid nitrogen, and stored at -80 °C. Ileum and large intestine were separated and the contents of the terminal ileum and large bowel were collected into 3 ml of phosphate buffered saline containing 10 mM dithiothreitol (DTT). All tissues and contents were stored at -80 °C until use.
UPLC-MS/MS analysis of BAs
Serum and liver samples were prepared and analyzed as described previously [33] with modification [11]. Individual bile acids were quantified by ultraperformance liquid chromatography–mass spectrometry (UPLC-MS/MS) according to peak areas and a series of working standard curves as described previously [11, 33]. The standards included unconjugated bile acids, which are cholic acid (CA), chenodeoxycholic acid (CDCA), α, β and ω muricholic acids (MCA), deoxycholic acid (DCA), lithocholic acid (LCA), ursodeoxycholic acid (UDCA), hyodeoxycholic acid (HDCA), and murideoxycholic acid (MDCA), as well as taurine (T) conjugates, which are TCA, TCDCA, TDCA, TLCA, TUDCA, and TMCA. Quantification of TωMCA and ωMCA were relative to TαMCA and αMCA respectively.
Total RNA isolation
Approximately 50 mg of liver or ileum were homogenized in 1 ml RNAzol Bee reagent (Tel-Test Inc., Friendswood, TX). Total messenger RNA (mRNA) was isolated according to the manufacturer’s protocol, and concentrations were quantified using a NanoDrop Spectrophotometer (NanoDrop Technologies, Wilmington, DE) at 260 nm. Formaldehyde-agarose gel eletrophoresis was used for evaluating the integrity of these total RNA samples, which were confirmed by visualization of the 18 s and 28 s rRNA bands. The diethyl pyrocarbamate (DEPC)-treated double-distilled water was used to dilute each of the RNA samples to 50 ng/μl for real-time PCR quantification.
Synthesis of cDNA and real-time PCR quantification
Reverse transcription of RNA to cDNA was performed using the Applied Biosystems High Capacity Reverse Transcriptase kit (Applied Biosystems, Foster City, CA). Subsequently, quantitative PCR was performed on the resulting cDNA using SYBR Green PCR Master Mix in 7300HT Fast Real-Time PCR System (Applied Biosystems). Primers (Additional file 1: Table S1) for RT-PCR were synthesized by Integrated DNA Technologies (Coralville, IA).
Bacterial DNA extraction and quantification
Bacterial DNA was extracted by QIAmp DNA® stool kit (Qiagen, Valencia, CA) following the instructions, and then techniques that rely on 16S rRNA gene sequences were used for the identification and classification of bacterial species as described previously [30, 34]. In brief, intestinal contents were centrifuged at 20,000 g for 30 min at 4 °C. Total genomic bacterial DNA was extracted from the pellet. The integrity, concentration, and quality of the total DNA were assessed by agarose gel electrophoresis, and determined by absorption at A260, and A260 to A280 ratio, respectively. The 16S rDNA gene of 32 bacteria was quantified in pooled and individual samples using Quantigene 2.0 Reagent System (Panomics/Affymetrix, Fremont, CA) according to the manufacturer’s protocol.
Statistical analysis
Data are expressed as mean ± S.E. (n = 4-6). Differences between mean values were tested for statistical significance (P < 0.05) by one-way analysis of variance (ANOVA) followed by Duncan’s post hoc test. Spearman’s rank test was conducted to analyze the associations between BBR concentrations and BA profile, related genes and gut microbiota in mice (SPSS Inc., Chicago, IL, USA, version 16.0). Statistical significance was set at P < 0 · 05 for all analyses.
Results
Concentrations of T-conjugated BAs, unconjugated BAs and total BAs in livers and serum of control and BBR-treated mice
The T-conjugated BAs and total BAs did not change significantly in livers of the BBR-treated mice (Fig. 2a), however, in serum, the unconjugated BAs significantly increased (P = 0.0017) about 90–92 % at the two middle doses of BBR (10 and 30 mg/kg) while they tended to decrease after the highest dose. The total BAs in serum had a similar trend to unconjugated BAs, with a significant decrease (P = 0.006, 62 %) after the highest dose of BBR. There was no significant change in the T-conjugated BAs in serum of mice fed the various doses of BBR (Fig. 2b).
Concentrations of T-conjugated BAs, unconjugated BAs and total BAs in control and BBR-treated mice. T-conjugated, unconjugated BAs and total BAs in liver and serum were quantified and the amounts are showed in a and b, respectively. All values are expressed as mean ± S.E.M. ANOVA followed by Duncan’s post hoc test were used, and * means P < 0.05 when compared with controls
Concentrations of individual BAs in livers of control and BBR-treated mice
Twenty individual BAs were quantified in livers of control and BBR-treated mice (Fig. 3a–b). Of the 10 primary BAs, βMCA (P = 0.004) and TβMCA (P = 0.001) were increased about 100 % in mice treated with 100 or 300 mg/kg BBR, and TUDCA was increased 60 % in livers of mice treated with 100 mg/kg BBR (P = 0.038), whereas the other BAs were not significantly changed (Fig. 3a). BBR significantly decreased the secondary BAs (DCA: P = 0.000006; TDCA: P = 0.000002; LCA: P = 0.0009; ωMCA: P = 0.00027; TωMCA: P = 0.00004; MDCA: P = 0.001; TMDCA: P = 0.001; HDCA: P = 0.00000003; THDCA: P = 0.000000002. Fig. 3b). BBR at the highest dose (300 mg/kg) decreased the concentration of all the secondary BAs in liver. The second to the highest dose of BBR (100 mg/kg) decreased DCA, TDCA, LCA, TLCA, and HDCA. Lower doses of BBR also decreased DCA and TDCA.
Concentrations of individual BAs in livers of control and BBR-treated mice. Twenty individual BAs were quantified in livers of 8-week-old control and BBR-treated mice. a showed the amounts of 10 primary BAs, and b showed the amount of 10 secondary BAs. All values are expressed as mean ± S.E.M. ANOVA followed by Duncan’s post hoc test were used, and * means P < 0.05 when compared with controls
Concentrations of individual BAs in serum of control and BBR-treated mice
Eight primary and four secondary BAs were detected in serum of control and BBR-treated mice (Fig. 4a–b). BA concentrations in serum were much lower than that in liver. Coincident with the rise of primary BAs in liver, βMCA in serum was about 100 % higher (P = 0.012) in all the BBR-treated mice except for the lowest dose (Fig. 4a). Moreover, BBR increased CA 300–400 % in the 10 and 30 mg/kg groups (P = 0.00006), and the 30 mg/kg increased CDCA (P = 0.007) about 50 %. BBR at 30 mg/kg increased αMCA about 300 %, however, no αMCA was detected in the serum after 300 mg/kg (P = 0.003). The secondary BAs in serum, including DCA (P = 0.007) and TDCA (P = 0.016), decreased about 85 % after the highest dose of BBR (Fig. 4b). The changes of ωMCA in serum was similar to that of αMCA, that is the intermediate doses of BBR doubled their concentrations (P = 0.002) in serum.
Concentrations of individual BAs in serum of control and BBR-treated mice. Eight primary (a) and four secondary BAs (b) were detected in serum of control and BBR-treated mice. All values are expressed as mean ± S.E.M. ANOVA followed by Duncan’s post hoc test were used, and * means P < 0.05 when compared with controls
mRNA expression of major BA-related genes in livers of control and BBR-treated mice
To investigate probable mechanisms for the changes of BA concentrations in mice treated with BBR, major genes that are involved in BA synthesis, uptake, efflux and regulation of the processes were examined (Fig. 5).
mRNA expression of major BA-related genes in livers of control and BBR-treated mice were examined (Fig. 5). BA synthetic enzymes involved in classical and alternative pathway were quantified in liver of BBR-treated mice (a). The mRNA expression of major BAs regulating factors in liver including FXR, SHP and Fgfr4 is demonstrated in (b). c illustrates the mRNA expression of major uptake transporters on the basolateral membrane of hepatocyte, which include Ntcp, Oatp1b2. The mRNA expression of major efflux transporters on the basolateral and canalicular membrane of hepatocyte are shown in (d). The left panel in d demonstrates the alteration of major efflux transporters on the canalicular membrane. The right panel of d shows the change of major efflux transporters on the basolateral membrane transporting the bile acids back to the blood after various doses of BBR. All values are expressed as mean ± S.E.M. ANOVA followed by Duncan’s post hoc test were used, and * means P < 0.05 when compared with controls
Enzymes involved in the classical and alternative pathways of BA synthesis were quantified in livers of BBR-treated mice (Fig. 5a). After BBR treatment, the mRNA of Cyp7a1, which is the rate-limiting enzyme in the classic pathway increased 200–400 % (P = 0.001), and Cyp8b1 mRNA increased up to 100 % (P = 0.003). The other enzymes involved in BA synthesis had a relatively minor change.
The mRNA expression of major factors regulating BAs in liver, including FXR, SHP and Fgfr4 are shown in Fig. 5b. Induction of FXR was less than 50 % in liver of mice treated with 300 mg/kg BBR (P = 0.001), and there was no significant difference of SHP or Fgfr4 mRNA expression in mice fed BBR.
Figure 5c illustrates the mRNA expression of major uptake transporters on the basolateral membrane of hepatocytes, which includes the Na+-dependent taurocholate cotransport peptide (Ntcp), and the organic anion–transporting polypeptide (Oatp) 1b2. Ntcp increased less than 50 % (P = 0.0003), and Oatp1b2 was increased about 100 % after 100 and 300 mg/kg BBR (P = 0.013).
The mRNA expression of major efflux transporters on the basolateral and canalicular membranes of hepatocytes is shown in Fig. 5d. The left panel of Fig. 5d demonstrates the alteration of major efflux transporters on the canalicular membrane, which transport chemicals into bile. There were no significant changes for most of these transporters after BBR treatment, however, Mdr2 was increased about 80 % after the highest dose of BBR (P = 0.000007). The right panel of Fig. 5d shows the major efflux transporters on the basolateral membrane that transport chemicals from the liver back to the blood. Mrp3 (P = 0.018) and Mrp4 (P = 0.020) were decreased about 30 % in mice that received the highest dose of BBR.
mRNA expression of major regulating factors and transporters in ileum of control and BBR-treated mice
Because BA concentrations only changed in mice that were given doses of BBR above 30 mg/kg, mRNA expression of FXR, Fgf15, Ostα, Ostβ and Asbt were quantified in the mice given the 3 highest doses of BBR (Fig. 6). Although not statistically significant, mRNA expression of these BA related genes after 100 and 300 mg/kg BBR tended to decrease. However, mice administered 30 mg/kg BBR had decreased expression of FXR and Ostα (37–39 % suppression) and Fgf15 (68 % suppression) in ileum (P = 0.05).
mRNA expression of major regulating factors and transporters including FXR, Fgf15, Ostα, Ostβ and Asbt in ileum of control and BBR-treated mice were quantified with the 3 higher doses groups. All values are expressed as mean ± S.E.M. ANOVA followed by Duncan’s post hoc test were used, and * means P < 0.05 when compared with controls
Bacteria in terminal ileum and large intestinal contents of control and BBR-treated mice
BBR-induced decreases in the concentration of secondary BAs were most evident in mice after the two highest doses of BBR, therefore, the relative amounts of 16S rRNA for 32 of the most abundant gut bacterial species in mice were quantified in pooled samples of control, 100 and 300 mg/kg BBR-treated groups (Fig. 7a), and validated by 7 bacteria in individual samples (Fig. 7b). In pooled samples, Bacteroides increased, but other bacteria decreased with the increasing dosage of BBR. In the individual samples, Ruminococcus gnavus and Ruminococcus schinkii decreased about 40 % (P = 0.007) and 60 % (P = 0.011) in the 100 and 300 mg/kg BBR-treated groups, respectively. Lactobacillus acidophilus, Lactobacillus murinus and Lactococcus lactis decreased about 60 to 90 % in the 300 mg/kg BBR treated mice (Lactobacillus acidophilus: P = 0.013; Lactobacillus murinus: P = 0.002; Lactococcus lactis: P = 0.05). The changes were similar in the pooled versus the individual samples.
Bacteria in terminal ileum and large intestinal contents of control and BBR-treated mice. The relative amounts of 32 of the most abundant gut bacterial species in mice were quantified in the pooled samples of control, 100 and 300 mg/kg BBR treated groups (a), and validated by 7 bacteria in individual samples (b). All values are expressed as mean ± S.E.M. ANOVA followed by Duncan’s post hoc test were used, and * means P < 0.05 when compared with controls
Dose-response of BBR in mice
The associations between BBR concentrations and BA profile, related genes and gut microbiota in mice were analyzed, and the P (those are smaller than 0.05) and R values are shown in Table 1. The primary BAs in livers and serum, as well as related genes in the livers of BBR-treated mice including Oatp1b2, Bsep, Mdr2, Cyp8b1, Cyp7a1, Ntcp and FXR (in liver) were positively correlated to the increase of BBR concentrations, whereas secondary BAs and bacteria including Ruminococcus gnavus, Ruminococcus schinkii, Lactobacillus acidophilus, Lactobacillus murinus and Lactococcus lactis in terminal ileum and large intestinal contents were negatively correlated to the increase of BBR concentrations.
Discussion
Although BBR is used as an herbal medicine and supplement for many ailments, including glucose and lipid metabolism disorders, knowledge about the dose-response of BBR on BAs (which regulate energy homeostasis) and gut flora (which have roles in BA metabolism) in mice are unknown. In the present study, effects of various doses of BBR on BA concentrations in liver and serum, mRNA expression of BA-related genes, as well as the amount of 32 of the most abundant interestinal bacterial species in control mice were examined [30, 34].
Total BAs, including T-conjugated and unconjugated BAs, were not significantly altered in liver, but a change in the serum concentration of BAs was observed in mice treated with BBR. More specifically, unconjugated BAs increased about 90 % in serum of mice treated with 10 and 30 mg/kg BBR, and there was an increase in primary BAs (βMCA, TβMCA and TUDCA) and a decrease in secondary BAs (DCA, LCA and the T-conjugates). With the highest dose of BBR, there was a marked decrease in serum BA concentrations. The expression of BA-synthesis enzymes (Cyp7a1 and 8b1) and uptake transporters (Ntcp) increased 39–400 % in livers of mice treated with higher doses of BBR, whereas nuclear receptors and efflux transporters were not dramatically changed. In addition, Bacteroides were exclusively enriched in the terminal ileum and large bowel of mice treated with the higher doses of BBR. Thus, this study shows that BBR has effects on modulating gut microbiota and host BA metabolism.
There are similarities of mice raised in germ-free environment and mice fed BBR. For example, the total BAs in liver were not altered in mice treated with 300 mg/kg BBR (Fig. 2a) or housed in a germ-free environment; however, the total BAs in serum (Fig. 2b) decreased markedly in both experimental groups [14]. As for individual BAs, an increase in βMCA and TβMCA but a decrease in secondary BAs was the major phenotype in liver of both mice given 300 mg/kg BBR (Fig. 3) or housed in a germ-free environment. However, in serum, TβMCA increased markedly in germ-free mice [14] but did not significantly change in mice given 300 mg/kg BBR (Fig. 4a). In addition, the general expression pattern of BA-related genes in liver of 300 mg/kg BBR-treated mice, including increased rate-limiting synthetic enzyme (Fig. 5a) and uptake transporters (Fig. 5c), as well as decreased efflux transporters (Fig. 5d) resembled that in livers of germ-free mice, but in ileum, the suppression of Fgf15 in germ-free mice was not reproduced (Fig. 6) in the 300 mg/kg BBR-treated mice [14].
The expression of the Cyp7a1, the rate-limiting enzyme in the synthetic pathway (Fig. 5a), and Cyp8b1, the 12α-hydroxylase responsible for the synthesis of CA, as well as BA-uptake transporter Ntcp increased in livers of mice treated with the higher doses of BBR (Fig. 5c), but other genes, including the nuclear receptors and efflux transporters, were not altered (Fig. 5d). The expression of FXR increased 63 % in livers of mice treated with 300 mg/kg BBR (Fig. 5b), however, neither the expression of SHP increased nor the BA synthesis enzymes decreased. But in fact, Cyp7a1 and 8b1 were increased, while the FXR-Fgf15 pathway was down-regulated by BBR. Therefore, the decrease in the inhibition of FXR-Fgf15 pathway is likely the reason for the increase of BA synthesis in liver. The changes of individual BAs in the intestine are likely responsible for the decrease in FXR activation in the intestine, as it has been reported that some BAs are antagonists (αMCA, βMCA and their T-conjugates as well as UDCA) and agonists (CDCA, TCDCA, TCA, TDCA, DCA and CA) of the FXR-Fgf15 pathways [14, 16–18]. The most obvious change of the ratio for αMCA + βMCA + TαMCA + TβMCA + UDCA/CDCA + TCDCA + TCA + TDCA + DCA + CA exhibited at 30 mg/kg group. Interestingly, this group also showed the most dramatic decrease of Fgf15 (Fig. 6), which means the FXR signaling activated by BAs in the intestine decreased. This was consistent with the results observed in germ-free mice [14].
BBR is reported to be a broad-spectrum antibiotic, which in this study enriched Bacteroides and decreased Ruminococcus in the terminal ileum and large bowel (Fig. 7). The present results are consistent with previous work in mice treated with normal chow and a high-fat diet co-administrated with 100 mg/kg BBR [26]. Bacteroides, which deconjugates T-conjugated BAs [35], were enriched by BBR. In the current study, this may result in rapid deconjugation of T-conjugated BAs in the intestine, and account for the trend of decreasing TαMCA and TβMCA concentrations in serum of mice treated with the higher BBR doses, leading to decreased amounts of these BAs in the serum. Therefore, the increase of Bacteroides might be the reason of the difference of TβMCA in serum between germ-free mice and BBR treatment. However, the possibility that antibiotics might have a direct effect on BA metabolism should not be excluded. Further studies by experimental modulation of the bacteria in the intestine may help to directly prove the association of gut flora changes and the alteration of BA composition and quantity in mice treated with BBR.
Some of the previously reported pharmacological effects of BBR might be related to the change in amount and composition of BAs. In mice treated with higher doses of BBR, the quantity of βMCA and its conjugates were elevated. Moreover, although the increase of UDCA was not statistically significant, the relative abundance of UDCA might increase in parallel with the decrease of other BAs in liver and serum (Figs. 3 and 4). The increase of UDCA, βMCA and their conjugates might be cytoprotective by lowering intracellular TCDCA, which is thought to be cytotoxic due to its hydrophilic nature [36, 37]. βMCA and (T)UDCA also protect against drug-induced cholestasis, possibly by inducing a signaling cascade by activating protein kinase C (PKC) [38], or blocking DCA-induced nuclear factor-kappaB (NF-kappaB) and activator protein-1 (AP-1) activity, as reported in colorectal HCT116 cells, which corresponds to the effects of BBR [21, 39–41]. BBR decreased secondary BAs such as DCA and LCA, which might decrease the hydrophobicity and toxicity of the BA pool [8]. Increased DCA can induce nitric oxide mediated DNA damage [42], and treatment of LCA or its conjugate to animals causes intrahepatic cholestasis [43, 44]. In addition, serum levels of DCA in colon cancer patients have been shown to be consistently higher than that in healthy subjects [45, 46]. In the present study, BBR treatment decreased DCA, LCA, and their conjugates in liver and serum of mice (Figs. 3 and 4), which might relate to the potential of BBR to decrease liver cancer [21]. BAs with two hydroxyl groups (CDCA and DCA) induce fluid secretion, increase mucosal permeability, and produce mucosal damage [47]; thus, a decrease of DCA by BBR treatment may contribute to its anti-diarrheal effect. In addition, BAs have metabolic actions in the body resembling those of hormones by acting through TGR5, and the potency of BAs to activate TGR5 has been reported to be LCA > DCA > CDCA > CA [30]. BBR is an antibiotic, which would decrease secondary BAs in mice and the corresponding composition of BAs might negatively regulate TGR5 in BBR-treated mice. However, BBR has been reported to exhibit similar effects to TGR5 activation [48, 49]. Therefore, further studies are required to quantify the expression and activity of TGR5 in mice treated with BBR. Additionally, determining the effect of BA feeding combined with BBR treatment, and the influence of BBR on genetically modified mouse models might provide us with clues to the underlying relationship between BBR and BAs.
Conclusion
The results of the present study showed that various doses of BBR have effects on BA metabolism and signaling pathways as well as gut flora, which will provide guidance for further studies to determine the mechanisms of BBR effects.
Abbreviations
- BA:
-
Bile acid
- BBR:
-
Berberine
- Bsep:
-
Bile salt export pump
- CA:
-
Cholic acid
- CAR:
-
Constitutive androstane receptor
- CDCA:
-
Chenodeoxycholic acid
- Cyp:
-
Cytochrome P450
- DCA:
-
Deoxycholic acid
- EHC:
-
Enterohepatic circulation
- Fgf:
-
Fibroblast growth factor
- Fgfr4:
-
FGF receptor 4
- FXR:
-
Farnesoid X receptor
- G:
-
Glycine
- HDCA:
-
Hyodeoxycholic acid
- LCA:
-
Lithocholic acid
- LRH-1:
-
Liver receptor homolog-1
- MCA:
-
Muricholic acids
- MDCA:
-
Murideoxycholic acid
- Mdr:
-
Multiple drug resistance
- mRNA:
-
Messenger RNA
- Mrp:
-
Multidrug resistance-associated protein
- NF-kappaB:
-
Nuclear factor-kappaB
- Ntcp:
-
Na+-dependent taurocholate cotransporting peptide
- Oatp:
-
Organic anion–transporting polypeptide
- Ost:
-
Organic solute transporter
- PK:
-
Protein kinase
- SHP:
-
Small heterodimer partner
- T:
-
Taurine
- TGR5:
-
Transmembrane G-protein-coupled receptor 5
- UDCA:
-
Ursodeoxycholic acid
- UPLC-MS:
-
Ultraperformance liquid chromatography–mass spectrometry
References
Hofmann AF. The continuing importance of bile acids in liver and intestinal disease. Arch Intern Med. 1999;159(22):2647–58.
Watanabe M, Houten SM, Mataki C, Christoffolete MA, Kim BW, Sato H, et al. Bile acids induce energy expenditure by promoting intracellular thyroid hormone activation. Nature. 2006;439(7075):484–9. doi:10.1038/nature04330.
Fiorucci S, Cipriani S, Mencarelli A, Renga B, Distrutti E, Baldelli F. Counter-regulatory role of bile acid activated receptors in immunity and inflammation. Curr Mol Med. 2010;10(6):579–95.
Song P, Zhang Y, Klaassen CD. Dose-response of five bile acids on serum and liver bile Acid concentrations and hepatotoxicty in mice. Toxicol Sci. 2011;123(2):359–67. doi:10.1093/toxsci/kfr177.
Powolny A, Xu J, Loo G. Deoxycholate induces DNA damage and apoptosis in human colon epithelial cells expressing either mutant or wild-type p53. Int J Biochem Cell Biol. 2001;33(2):193–203.
Ridlon JM, Kang DJ, Hylemon PB. Bile salt biotransformations by human intestinal bacteria. J Lipid Res. 2006;47(2):241–59. doi:10.1194/jlr.R500013-JLR200.
McGarr SE, Ridlon JM, Hylemon PB. Diet, anaerobic bacterial metabolism, and colon cancer: a review of the literature. J Clin Gastroenterol. 2005;39(2):98–109.
Bajor A, Gillberg PG, Abrahamsson H. Bile acids: short and long term effects in the intestine. Scand J Gastroenterol. 2010;45(6):645–64. doi:10.3109/00365521003702734.
Lorbek G, Lewinska M, Rozman D. Cytochrome P450s in the synthesis of cholesterol and bile acids--from mouse models to human diseases. FEBS J. 2012;279(9):1516–33. doi:10.1111/j.1742-4658.2011.08432.x.
Klaassen CD, Aleksunes LM. Xenobiotic, bile acid, and cholesterol transporters: function and regulation. Pharmacol Rev. 2010;62(1):1–96. doi:10.1124/pr.109.002014.
Zhang Y, Klaassen CD. Effects of feeding bile acids and a bile acid sequestrant on hepatic bile acid composition in mice. J Lipid Res. 2010;51(11):3230–42. doi:10.1194/jlr.M007641.
Rajilic-Stojanovic M. Function of the microbiota. Best Pract Res Clin Gastroenterol. 2013;27(1):5–16. doi:10.1016/j.bpg.2013.03.006.
Lu TT, Makishima M, Repa JJ, Schoonjans K, Kerr TA, Auwerx J, et al. Molecular basis for feedback regulation of bile acid synthesis by nuclear receptors. Mol Cell. 2000;6(3):507–15.
Sayin SI, Wahlstrom A, Felin J, Jantti S, Marschall HU, Bamberg K, et al. Gut microbiota regulates bile acid metabolism by reducing the levels of tauro-beta-muricholic acid, a naturally occurring FXR antagonist. Cell Metab. 2013;17(2):225–35. doi:10.1016/j.cmet.2013.01.003.
Chiang JY. Bile acids: regulation of synthesis. J Lipid Res. 2009;50(10):1955–66. doi:10.1194/jlr.R900010-JLR200.
Wang H, Chen J, Hollister K, Sowers LC, Forman BM. Endogenous bile acids are ligands for the nuclear receptor FXR/BAR. Mol Cell. 1999;3(5):543–53.
Makishima M, Okamoto AY, Repa JJ, Tu H, Learned RM, Luk A, et al. Identification of a nuclear receptor for bile acids. Science. 1999;284(5418):1362–5.
Hu X, Bonde Y, Eggertsen G, Rudling M. Muricholic bile acids are potent regulators of bile acid synthesis via a positive feedback mechanism. J Intern Med. 2014;275(1):27–38. doi:10.1111/joim.12140.
Li Y, Jadhav K, Zhang Y. Bile acid receptors in non-alcoholic fatty liver disease. Biochem Pharmacol. 2013;86(11):1517–24. doi:10.1016/j.bcp.2013.08.015.
Csanaky IL, Lu H, Zhang Y, Ogura K, Choudhuri S, Klaassen CD. Organic anion-transporting polypeptide 1b2 (Oatp1b2) is important for the hepatic uptake of unconjugated bile acids: Studies in Oatp1b2-null mice. Hepatology. 2011;53(1):272–81. doi:10.1002/hep.23984.
Vuddanda PR, Chakraborty S, Singh S. Berberine: a potential phytochemical with multispectrum therapeutic activities. Expert Opin Investig Drugs. 2010;19(10):1297–307. doi:10.1517/13543784.2010.517745.
Sun N, Chan FY, Lu YJ, Neves MA, Lui HK, Wang Y, et al. Rational design of berberine-based FtsZ inhibitors with broad-spectrum antibacterial activity. PLoS One. 2014;9(5):e97514. doi:10.1371/journal.pone.0097514.
Barnes PM, Bloom B, Nahin RL. Complementary and alternative medicine use among adults and children: United States, 2007. Natl Health Stat Report. 2008;10(12):1–23.
Homma N, Kono M, Kadohira H, Yoshihara S, Masuda S. The effect of berberine chloride on the intestinal flora of infants. Arzneimittelforschung. 1961;11:450–4.
Chae SH, Jeong IH, Choi DH, Oh JW, Ahn YJ. Growth-inhibiting effects of Coptis japonica root-derived isoquinoline alkaloids on human intestinal bacteria. J Agric Food Chem. 1999;47(3):934–8.
Zhang X, Zhao Y, Zhang M, Pang X, Xu J, Kang C, et al. Structural changes of gut microbiota during berberine-mediated prevention of obesity and insulin resistance in high-fat diet-fed rats. PLoS One. 2012;7(8):e42529. doi:10.1371/journal.pone.0042529.
Han J, Lin H, Huang W. Modulating gut microbiota as an anti-diabetic mechanism of berberine. Med Sci Monit. 2011;17(7):RA164–7.
Zhang Q, Xiao X, Feng K, Wang T, Li W, Yuan T et al. Berberine moderates glucose and lipid metabolism through multipathway mechanism. Evid Based Complement Altern Med. 2011;2011. doi:10.1155/2011/924851
Wang Y, Jia X, Ghanam K, Beaurepaire C, Zidichouski J, Miller L. Berberine and plant stanols synergistically inhibit cholesterol absorption in hamsters. Atherosclerosis. 2010;209(1):111–7. doi:10.1016/j.atherosclerosis.2009.08.050.
Zhang Y, Limaye PB, Renaud HJ, Klaassen CD. Effect of various antibiotics on modulation of intestinal microbiota and bile acid profile in mice. Toxicol Appl Pharmacol. 2014;277(2):138–45. doi:10.1016/j.taap.2014.03.009.
Chan MY. The effect of berberine on bilirubin excretion in the rat. Comp Med East West. 1977;5(2):161–8.
Tsai PL, Tsai TH. Hepatobiliary excretion of berberine. Drug Metab Dispos. 2004;32(4):405–12. doi:10.1124/dmd.32.4.405.
Alnouti Y, Csanaky IL, Klaassen CD. Quantitative-profiling of bile acids and their conjugates in mouse liver, bile, plasma, and urine using LC-MS/MS. J Chromatogr B Analyt Technol Biomed Life Sci. 2008;873(2):209–17. doi:10.1016/j.jchromb.2008.08.018.
Zhang Y, Limaye PB, Lehman-McKeeman LD, Klaassen CD. Dysfunction of organic anion transporting polypeptide 1a1 alters intestinal bacteria and bile acid metabolism in mice. PLoS One. 2012;7(4):e34522. doi:10.1371/journal.pone.0034522.
Masuda N. Deconjugation of bile salts by Bacteroids and Clostridium. Microbiol Immunol. 1981;25(1):1–11.
Ohiwa T, Katagiri K, Hoshino M, Hayakawa T, Nakai T. Tauroursodeoxycholate and tauro-beta-muricholate exert cytoprotection by reducing intrahepatocyte taurochenodeoxycholate content. Hepatology. 1993;17(3):470–6.
Takikawa H, Sano N, Aiso M, Takamori Y, Yamanaka M. Effect of tauro-alpha-muricholate and tauro-beta-muricholate on oestradiol-17 beta-glucuronide-induced cholestasis in rats. J Gastroenterol Hepatol. 1997;12(1):84–6.
Milkiewicz P, Roma MG, Elias E, Coleman R. Hepatoprotection with tauroursodeoxycholate and beta muricholate against taurolithocholate induced cholestasis: involvement of signal transduction pathways. Gut. 2002;51(1):113–9.
Jiang Q, Liu P, Wu X, Liu W, Shen X, Lan T, et al. Berberine attenuates lipopolysaccharide-induced extracelluar matrix accumulation and inflammation in rat mesangial cells: involvement of NF-kappaB signaling pathway. Mol Cell Endocrinol. 2011;331(1):34–40. doi:10.1016/j.mce.2010.07.023.
Kim S, Choi JH, Kim JB, Nam SJ, Yang JH, Kim JH, et al. Berberine suppresses TNF-alpha-induced MMP-9 and cell invasion through inhibition of AP-1 activity in MDA-MB-231 human breast cancer cells. Molecules. 2008;13(12):2975–85. doi:10.3390/molecules13122975.
Luo Y, Hao Y, Shi TP, Deng WW, Li N. Berberine inhibits cyclin D1 expression via suppressed binding of AP-1 transcription factors to CCND1 AP-1 motif. Acta Pharmacol Sin. 2008;29(5):628–33. doi:10.1111/j.1745-7254.2008.00786.x.
Clemons NJ, McColl KE, Fitzgerald RC. Nitric oxide and acid induce double-strand DNA breaks in Barrett's esophagus carcinogenesis via distinct mechanisms. Gastroenterology. 2007;133(4):1198–209. doi:10.1053/j.gastro.2007.06.061.
Fisher MM, Magnusson R, Miyai K. Bile acid metabolism in mammals. I. Bile acid-induced intrahepatic cholestasis. Lab Invest. 1971;25(1):88–91.
Javitt NB. Cholestasis in rats induced by taurolithocholate. Nature. 1966;210(5042):1262–3.
Bayerdorffer E, Mannes GA, Ochsenkuhn T, Dirschedl P, Paumgartner G. Variation of serum bile acids in patients with colorectal adenomas during a one-year follow-up. Digestion. 1994;55(2):121–9.
Bayerdorffer E, Mannes GA, Richter WO, Ochsenkuhn T, Wiebecke B, Kopcke W, et al. Increased serum deoxycholic acid levels in men with colorectal adenomas. Gastroenterology. 1993;104(1):145–51.
Chadwick VS, Gaginella TS, Carlson GL, Debongnie JC, Phillips SF, Hofmann AF. Effect of molecular structure on bile acid-induced alterations in absorptive function, permeability, and morphology in the perfused rabbit colon. J Lab Clin Med. 1979;94(5):661–74.
Wang Y, Huang Y, Lam KS, Li Y, Wong WT, Ye H, et al. Berberine prevents hyperglycemia-induced endothelial injury and enhances vasodilatation via adenosine monophosphate-activated protein kinase and endothelial nitric oxide synthase. Cardiovasc Res. 2009;82(3):484–92. doi:10.1093/cvr/cvp078.
Keitel V, Reinehr R, Gatsios P, Rupprecht C, Gorg B, Selbach O, et al. The G-protein coupled bile salt receptor TGR5 is expressed in liver sinusoidal endothelial cells. Hepatology. 2007;45(3):695–704. doi:10.1002/hep.21458.
Acknowledgements
The authors thank Dr. Helen J. Renaud for proofreading this manuscript, Dr. Xingguo Cheng for technical support of the experiments, and Dr. Pallavi B. Limaye for technical assistance in bacteria quantification, Xiaohong Lei in Dr. Klaassen's lab for support of the experiments, as well as other members of Dr. Klaassen’s laboratory for critical review of the manuscript.
Funding
This work was supported by the National Institutes of Health [Grants ES-025708, ES009649, ES019487]; and the National Scientific Foundation of China [Grant 81503563].
Availability of data and materials
The datasets and materials supporting the conclusions of this article are presented in this main paper.
Authors’ contributions
YG, YCZ and CDK conceived and designed the experiments; YG, YCZ and FPS performed the experiments; YG, YCZ and CDK analyzed the data; YG, YCZ, WHH and CDK wrote the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interest.
Consent for publication
Not applicable.
Ethics approval and consent to participate
All experiments were performed in accordance with the guidelines of the Institutional Animal Care and Use Committee at the University of Kansas Medical Center, enforced on March 22, 2010, and approved by the Institutional Animal Care and Use Committee at the University of Kansas Medical Center (permit number 2007-1704).
Author information
Authors and Affiliations
Corresponding author
Additional file
Additional file 1: Table S1.
RT-PCR primers for related genes. (DOCX 15 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Guo, Y., Zhang, Y., Huang, W. et al. Dose-response effect of berberine on bile acid profile and gut microbiota in mice. BMC Complement Altern Med 16, 394 (2016). https://doi.org/10.1186/s12906-016-1367-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12906-016-1367-7