Abstract
Background
Most studies on female sexual dysfunction are performed in population inventories and under specific clinical conditions. These approaches are performed using validated psychometric scales. Different scales to assess sexual function use different numbers of questions to characterize their domains. They also may or may not include domains of interaction between sexual partners. The objective of this study was to compare the precision between scales to be able to analyze their accuracy for better diagnosis of sexual dysfunction.
Methods
Fifty (50) healthy young women were enrolled in this study. Three questionnaires (FSFI, SQ-F, and GRISS) were applied to assess sexual function (n = 44). The accuracy measured by the area under the ROC curve (AUC) for individual domains and to cross-validated pairwise comparison of the three analyzed instruments was used. Kruskall-Wallis test to analyze individual domains of the scales was also used.The P-value was established as 0.05.
Results
The results showed that all domains and total FSFI and GRISS scores were significantly different between normal and dysfunctional women, but not for SQ-F domains. Indeed, AUC accuracy varied from excellent-good domain discrimination for FSFI and GRISS, but fair-poor for SQ-F. For the paired comparison between the three questionnaires a fair accuracy was detected. The specificity percentage was around 84% whereas that for sensibility was low, around 30%.
Conclusions
The best agreement was between FSFI and SQ-F, probably being related to high similar shared questions when compared to GRISS. The agreement between SQ-F and GRISS was low possible due to low number of questions in SQ-F to characterize similar domains. This study evidenced high agreement between scales to sensitivity and low agreement for specificity, thereby conferring fair accuracy between them. Thus, the limited grade for discriminatory capacity (AUC) for sexual response should be considered when comparing results from these three different questionnaires and also when comparing with other different scales. In addition, despite the diversity of scales, the high reliability and fit for their desire domain suggest that the FSFI scale has good accuracy for the current clinical assessment of women’s sexual health.
Clinical trial registration
NCT03241524. Retrospectively registered on 08/02/2017.
Similar content being viewed by others
Background
Most studies on female sexual dysfunction (FSD) are performed in population inventories and under specific clinical conditions such as postpartum, urinary incontinence, post-breast cancer surgery, obesity, and diabetes, among others [1,2,3,4,5]. These approaches are performed using validated psychometric scales, with the most frequently used being FSFI [6], GRISS [7] and, also, the SQ-F in the Brazilian population [8].
Female sexual dysfunction is a complex and multi-faceted disorder that has a wide spectrum of symptoms and severity and during their life cycle, women are frequently incapable or disinterested in participating in a sexual relationship. The causes are often multifactorial, requiring multidisciplinary assessment that addresses biological, psychological, sociocultural and relational aspects [9]. The concept of female sexual response has changed since Basson et al. [10] proposed the inclusion of an intimacy-based sex response cycle, in a nonlinear model that incorporates the value of emotional intimacy, sexual stimulus, and satisfaction with the relationship to replace the current linear model. In this context, in addition to a reproductive repertoire, sexuality comprises both physical and psychological feelings during part of a woman’s lifetime both for their own feeling as well as in relation to their partner [11]. In this perspective, scales which have included domains of interaction between sexual partners could have a higher chance to better diagnose sexual dysfunction.
According to the Fifth Edition of the Diagnostic and Statistical Manual [12] three disorders are cited: Female Orgasmic Disorder (FOD); Female Sexual Interest/Arousal Disorder (FSAD), and Genito-Pelvic Pain/Penetration Disorder (GPPPD). These disorders include four main domains for desire, arousal, orgasm, and pain (dyspareunia and vaginism), in which both physiological and psychological aspects of the female sexual experience influence the response [13].
Sexual dysfunctions are highly prevalent in the sexual disorders of both sexes according to Laumann, Paik & Rosen [14] who analyzed 1749 women and 1410 men, aged 18–59 years, living in the USA. The authors found that sexual dysfunction is more prevalent in women (43 to 34%), where the main complaints range from 27 to 32% for lack of interest in sex, 22–28% for inability to reach orgasm, 8–21% for pain during sex, and 17–27% for unpleasant sex.
For the Brazilian population, a study of 1219 women with a mean age of 35.6 + 12.31, observed that 49.0% exhibit at least one sexual dysfunction, 26.7% for desire, 23% dyspareunia and 21% for orgasm. In this study, educational level was inversely correlated with the risk of sexual desire, orgasm and pain dysfunctions during sexual intercourse [15]. In another cross-sectional study of 201 sexually active Brazilian women aged from 18 to 45 years, 90 from a public health service and 111 from private services, dysfunction occurred in 30.2% without a significant difference in the prevalence of sexual dysfunction or in sexual domain scores between income or educational status [16]. A prevalence of at least one type of sexual dysfunction in 36% of a sample of 100 women aged between 20 and 39 years old was also found [17]. Orgasm dysfunction occurred in 18% of the participants, and dyspareunia was reported by 13% of the women during the month prior to the study. Sexual appetite dysfunction occurred in 11% of the women, 8% had excitation dysfunction and only 1% reported vaginismus.
Even though there is high prevalence of sexual dysfunction in women, both physicians and patients are frequently hesitant to discuss this topic [18]. Moreover, according to reported sexual difficulties collected in the Global Study of Sexual Attitudes and Behaviors study 27,500 people (men and women aged 40–80 years) only around 19% (18.0% of men and 18.8% of women) sought medical help [19]. Sexual activity, sexual dysfunctions and related help-seeking behavior were investigated in adults (aged 40–80 years) using a telephone survey (5998 individuals; 2992 men and 3006 women) in 5 countries (United States, Canada, the United Kingdom, Australia, and New Zealand). Seventy-two percent (72%) of the respondents positive for dysfunction had no action in regards to it, and supposedly had a lack of perception or lack of discomfort about the problem. In addition, they did not know they needed to seek a doctor in such cases. Another cited cause was embarrassment (23%) [20]. Thus, this reflects lacking a favorable environment in both which men and women would feel not comfortable asking for information, and poses a challenge to physicians and other health professionals. This also indicates the importance of using questionnaires that have high precision resulting in accurate diagnoses and for effective monitoring treatments to counterbalance this gap [21, 22].
Sexual function has been evaluated by different surveys, but they may or not include domains of interaction with partners [21]. They also show a large variation in number of items that characterize each domain and they consequently vary in terms of psychometric properties. For example, FSFI is one of the most used questionnaires, but no domain related to the couple’s relationship is present. [6] On the other hand two others frequently used scales are the GRISS and SF-Q, with the latter being the most for the Brazilian population, covering issues where the quality of the couple’s relationships are addressed [7, 8]. Thus, the objective of this study was to compare the precision between scales which only quantify properties of female-specific sexual dysfunction and those which also score for quality of the couples’ relationship for diagnosing sexual dysfunction therefore directing the improvement of primary diagnosis of sexual disorders.
Methods
Study design and participants
This study is a quantitative descriptive applied research and used convenience sampling. The sample was composed of 60 female undergraduate students attending a private University in João Pessoa, northeastern Brazil, but only 50 agreed to participate in the study and also met the inclusion criteria. The inclusion criteria were: age between 19 and 35 years, heterosexual, active sex life, living in a stable relationship for at least 6 months no pregnancy or parturition in the last 6 months, clinically healthy and agreeing with the terms for participating in the study. Six women completed only 2 questionnaires and the final sample size for those women who filled out the three questionnaires was n = 44. The women were evaluated at the Physical Therapy Clinic and Laboratory of the Faculty where the study was conducted.
Assessment of female sexual response
Three questionnaires that assess sexual function were used to compare the accuracy in detecting both functional and dysfunctional sexual evaluation. The FSFI was selected because it is the most widely used instrument [20]. SQ-F is an instrument validated for the target population of this study, and GRISS (similar to SQ-F) includes an assessment of interactions with the sexual partner as one of its items. The three questionnaires were completed by the participants and all were translated and validated for Portuguese, as follows: (1) Female Sexual Function Index (FSFI), based on Rosen et al. [6]; (2) Female Sexual Quotient (SQ-F) validated for the Brazilian population [8] and (3) Sexual Satisfaction Inventory, female version (GRISS) based on Rust & Golombok [7] and Pacagnella et al. [23] validated and adapted for the Brazilian population [24].
Female sexual function index (FSFI) questionnaire
This questionnaire was proposed by Rosen et al. [6] for the diagnosis of female sexual function. The instrument was validated and adapted to Portuguese and contains 19 questions with multiple-choice responses that assess sexual function in the last four weeks, associated with six domains and possible types of disorders: (a) desire, (b) arousal, (c) lubrication, (d) orgasm, (e) satisfaction with sexual life, and (f) pain during or after intercourse. Participants completed the instrument by choosing the option that best described their situation. Each question was associated with a value corresponding to the degree of gratification of the participant. A score of 0 indicates no sexual activity in the last four weeks, and the others are numbered 1 to 5 on an incremental scale. For the pain domain, the range of values from 1 to 5 is inversed while the grades vary from 0 to 5 on questions 3 to 14 and 17 to19, and from 1 to 5, and for questions 1,2,15 and 16. The overall score is the sum of each domain multiplied by its corresponding factor and ranges from 2 to 36. Total scores smaller than 26 indicate one or more dysfunction in the specific domains.
SQ-F questionnaire (SQ-F)
SQ-F is an instrument developed and validated for Brazilian women by Abdo [8] and is composed of 10 questions that assess sexual function, addressing desire and interest in sex (questions 1, 2, 8), foreplay (question 3), sexual arousal and harmony with the partner (questions 4, 5), comfort in sexual intercourse (questions 6, 7) and orgasm and sexual satisfaction (questions 9, 10). The overall scores range from 0 to 100, in accordance with sexual performance, where: 82–100 = good to excellent; 62 |– 82 = regular to good; 42 |- 62 = unfavorable to regular; 22 |- 42 = bad to unfavorable; 0 |- 22 null to bad. A total score smaller than 62 indicates a poor sexual relationship.
Golombok-Rust inventory of sexual satisfaction (GRISS)
The GRISS questionnaire was developed to evaluate sexual dysfunction in heterosexual couples, discriminating between those with and without sexual difficulties. It is a 28-item questionnaire that produces a total GRISS score as well as two separate scales for both males and females. The scale has 8 items for females, including anorgasmia, vaginismus, non-communication, infrequency, female avoidance, female non-sensuality, female dissatisfaction, and anorgasmia [7]. The score ranges from 0 to 10, with values greater than 5 indicating sexual dysfunction.
Statistical analysis
To analyze the differences between each domain within each of the three scales, the Kruskall-Wallis nonparametric test was used to compare medians calculated in the group that presented the typical sexual response and, in the group, where the sexual response was dysfunctional. A p-value < 0.05 was established.
The diagnostic performance or accuracy of a test in discriminating disease cases from normal cases is evaluated using Receiver Operating Characteristic (ROC) curve analysis [25]. A receiver operating characteristics (ROC) graph is a technique for visualizing, organizing and selecting classifiers based on their performance. ROC analysis has been extended to visualize and analyze the behavior of diagnostic systems [26]. ROC curves can also be used to compare the diagnostic performance of two or more laboratory or diagnostic tests. The closer the ROC curve is to the upper left corner, the higher the overall accuracy of the test [26, 27].
The curve is created by plotting the true positive rate (TPR) against the false positive rate (FPR) at various threshold settings. The true-positive rate is also known as sensitivity, or recall in machine learning. The false-positive rate is also referred to as the fall-out and can be calculated as (1-specificity). Thus, the ROC curve is sensitivity as a function of fall-out.
Accuracy is measured by the area under the ROC curve (AUC) and is used in classification analysis to determine which of the models best predicts the classes. An area of 1 represents a perfect test and 0.5 a worthless test. A rough guide for classifying the accuracy of a diagnostic test is the traditional academic point system: 0.90–1 = excellent; 0.80–0.90 = good; 0.70–0.80 = fair; 0.60–0.70 = poor; 0.50–0.60 = fail.
The receiver operating characteristic (ROC) curve was used to test accuracy in predicting sexual function within domains and among the three instruments applied to evaluate female sexual response.
Results
In regard to relationship status, 60% of the participants reported being single (n = 30), 30.0% married (n = 15) and five divorced (10.0%). Fifty-six percent (56%) identified themselves as white (n = 28), 28.0% brown and 16.0% black. In relation to life style, 35.4% (n = 17) of the sample were social drinkers, 100% (n = 48) non-smokers, 70.8% sedentary. There were 60.4% (n = 29) who did not use birth control pills and 20.8% (n = 10) had children.
Within the sample, 18.8% (n = 9) of the women exhibited sexual dysfunctions according to the FSFI. Analysis using the SQ-F detected 7 women (14.6%) with sexual dysfunction, whereas the GRISS Inventory also found that 18.2% (n = 8) of the women presented dysfunctions.
Analysis by sexual response domains in the FSFI, SQ-F and GRISS questionnaires
For the three questionnaires, the total and individual means of scores by domains for functional and dysfunctional women are shown in Table 1. The Kruskall-Wallis test showed that FSFI differences between functional and dysfunctional women in relation to measured sexual variables (Desire, p-value < 0.05; Arousal, Lubrification, Satisfaction, Orgasm and Pain, p-value < 0.01) were significant. For SQ-F scale, significant differences between women with dysfunction and those without were not observed for any domain. Analysis for individual domains and total scores for GRISS showed significant differences in all (Infrequency, p-value < 0.05; No-Communication, Dissatisfaction, Avoidance, No-sensuality, Vaginism and Anorgasmia, p-value < 0.01).
With respect to the use of the three questionnaires to evaluate participants’ sexual dysfunction, most domains of each instrument showed good discriminatory capability using ROC analysis (Table 2). AUC values varied from excellent (0.90|-1.00) (FSFI: Arousal and Pain; and GRISS: Non-sexuality, Dissatisfaction) to fail (0.50|-0.60) (SQ-F: Preliminaries and Comfort). A good AUC rating (0.80|-0.90) was observed for FSFI (Lubrification, Satisfaction and Orgasm), and GRISS (Non-communication, Vaginismus, Anorgasmia). A fair AUC grade was detected for FSFI (Desire), GRISS (Infrequency) and SQ-F (Sexual interest, Satisfaction) and a poor AUC grade for SQ-F (Arousal).
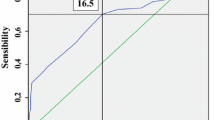
The SQ-F domains had a lower discriminatory capacity to indicate sexual dysfunction compared to the GRISS and FSFI domains, meaning that the domains of the last two instruments more accurately discriminated the sexual dysfunction of women. Figure 1 shows the graphical representation of the domains for each questionnaire and indicates that the closer the point approaches the upper left corner of the graph, the greater its ability to correctly estimate women who have the presence or absence of sexual dysfunction.
Analysis of the agreement between FSFI, SQ-F and GRISS questionnaires
Classifying a high-frequency diagnosis of sexual dysfunction of one particular instrument with another instrument that did not diagnose (false positive) and classify as no dysfunction when another instrument diagnosed dysfunction (false negative), demonstrates incompatibilities in the results of these instruments. Thus, to achieve the best combination of sensitivity and specificity, the results were analyzed and can be observed by the ROC curve (Fig. 2). As already mentioned, the closer the point approaches the upper left corner of the graph, the greater the instrument’s ability to correctly estimate women’s sexual disorders.
The statistical values for comparison between questionnaires in terms of sensibility (truth-positive, i.e. typical sexual function) and specificity (truth-negative, i.e. sexual dysfunction) indicate the agreement between each other and are shown in Table 3. The agreement between FSFI and SQ-F was 84.6% in detecting of women with normal sexual function and 33.3% in those with dysfunction, with an accuracy of 0.778 and a discriminatory capacity of around .59. The agreement between FSFI and GRISS was 28.6% for the diagnosis of true sexual dysfunction and 82.9% for women without sexual dysfunction. According to the results, the precision between these instruments was 0.738 and AUC = 0.557. The agreement between the GRISS and SQ-F questionnaires varied in terms of classifying women with dysfunction (25.0% sensitivity) and no dysfunction (82.1% specificity). Thus, the agreement between them was acceptable and accurate to 0.767, but with a regular discriminatory ability (AUC = 0.535). Thus, all these results were classified above 0.70, indicating good concordance between instruments with the highest agreement in predicting typical sexual function as well as sexual dysfunction was between FSFI x SQ-F (Table 3).
Discussion
According to the results of this study, all three questionnaires detected sexual dysfunction or its absence. The results showed “excellent to good”’ domain discrimination for FSFI and GRISS, but “fair to poor” for SQ-F. However, agreement for paired-comparison between the three questionnaires showed a similar fair accuracy for the detected sexual response. These findings indicate that even those questionnaires that have an excellent to fair accuracy in most domains (FSFI and GRISS), and that which show “fair to poor” agreement in detected dysfunction (SQ-F) are fair in accordance. This might have occurred because some domains need to be reviewed in terms of their detection ability in these scales. For instance, the desire domain shows low reliability [21] on the FSFI questionnaire, as well as in the present study, where it showed a fair probability (low sensibility and specificity) when compared to its other domains which were excellent or good. A similar specificity grade (fair) for desire was also observed for SQ-F and was probably higher due to this similarity agreement between both questionnaires. Moreover, the proximity among the domains explored by them are higher than those of GRISS.
The domains explored by GRISS are more general and also included the feelings about the partners while FSFI has only specific female psychometric properties and does not explore a partnerships evaluation.
Although the prevalence of sexual dysfunction increases in middle-age and menopause, a significant percentage of sexual dysfunctions are also reported for young women. For instance, in using a sample of 201 sexually active Brazilian women aged 18 to 45 years, Prado, Mota & Lima [16] demonstrated that sexual dysfunction affected 30.2% of these individuals. Similarly, Ferreira, Souza & Amorim [17] found that 36% of women aged between 20 and 39 years exhibit at least one type of sexual dysfunction, 18% for orgasm and 13% for dyspareunia.
Around 18% of the sample of the present study showed sexual dysfunctions and the concordance between questionnaires was around 30%, but increases to 80% for characterizing typical sexual function. Therefore, the use of questionnaires to investigate sexual function in women should be re-evaluated and updated to improve their reliability for diagnoses if necessary.
In a study where the scales for diagnosing female sexual dysfunction were systematized, 27 available scales were listed, of which ten measure psychometric properties of specific domains of sexual dysfunction in women [20]. Of these, five presented reliability scores equal to or above 0.9 (Cronbach’s alpha), including FSFI. However, only the FSFI [6] contains items that contemplate the general domains to characterize the female sexual response included in the DSM-5 [12]. For example, one scale specifically addressed a cut-off point for the desire disorder domain in FSFI in order to achieve high sensitivity and specificity. Both indices increased from 75 and 84% to 92 and 89%, respectively. This scale (FSFI), as previously mentioned, has a moderate discriminative effect for this domain [28]. The other scales showed good scores for arousability, [29] impact of sexual dysfunction on women’s sexual life quality, [30] and to exclusively diagnose hypoactive sexual desire disorder (HSDD) [31] or HSDD due female distress [32]. From this evidence, application of the FSFI scale associated to a correction of the desire sexual domain is recommended [28].
The present study has limitations in estimating the sensitivity of inter-questionnaire agreement, likely due to the sample size and the fact that only young women were assessed. Also, data generalization is restricted since the sampling was performed by convenience. However, this study showed evidence of a need to improve the questionnaires that are presently being used to better characterize female sexual function Although more complete protocols have been proposed in relation to the main aspects of sexual function for constructing guidelines of the sexual history of men and women for health care professionals, [33] at the moment this protocol is not available in the public health service. Thus, the high reliability and adjustments introduced in the FSFI seem to provide a good instrument for its current use in the clinical diagnosis of the sexual health of women.
Conclusions
A comparison of accuracy to detect typical sexual function and sexual dysfunction was investigated using three widely used questionnaires, namely the FSFI, GRISS and SQ-F. Precision grades from “excellent to good” were detected for most FSFI and GRISS individual domains, and “fair to poor” accuracy for SQ-F. Despite these results, the comparison between each 2 scales using the ROC curve to test the accuracy in predicting female sexual response diagnoses, were similar, being measured as “fair”. The sensitivity and specificity between FSFI x SQ-F were 84.6 and 33.3%, respectively, whereas between FSFI and GRISS were 82.9 and 28.6% and GRISS x SQ-F 82.1 and 25.0%. The number of questions per domains of the scales ranged from one to four, and it was found that lower scores for a domain for the FSFI were also low for a similar domain in the SQ-F. In addition, these two questionnaires have high similar questions when compared to GRISS. As SQ-F and GRISS contain items related to the sexual partnership a better agreement between them was expected. However, they were the lowest which might be due to the low number of questions on the SQ-F to characterize similar domains. This study evidenced high agreement between scales to truth-positive symptoms and low agreement for truth-negative symptoms thereby conferring fair accuracy between the studied scales. The limited grade for discriminatory capacity (AUC) between surveys for sexual response must be considered when comparing results from these three different questionnaires and also to compare with other different scales. In addition, despite the diversity of scales, the high reliability and fit for their desire domain suggest that the FSFI scale has good accuracy for the current clinical assessment of women’s sexual health.
Abbreviations
- FSFI:
-
Female Sexual Function Index
- SQ-F:
-
Female Sexual Quotient
- GRISS:
-
Golombok-Rust Inventory of Sexual Satisfaction
- ROC:
-
Receiver-operating characteristic
References
Leeman LM, Rogers RG. Sex after childbirth: postpartum sexual function. Obstet Gynecol. 2012;119(3):647–55. https://doi.org/10.1097/AOG.0b013e3182479611.
Chu CM, Arya LA, Andy UU. Impact of urinary incontinence on female sexual health in women during midlife. Women’s Midlife Health. 2015;1(6). https://doi.org/10.1186/s40695-015-0007-6.
Cornell LF, Mussallem DM, Gibson TC, Diehl NN, Bagaria SP, McLaughlin SA. Trends in sexual function after breast cancer surgery. Annals of Surgery Oncology. 2017;24(9):2526–38. https://doi.org/10.1245/s10434-017-5894-3.
Yaylali GF, Tekekoglu S, Akin F. (2010). Sexual dysfunction in obese and overweight women. International Journal of Impotence Research Jul-Aug. 2010;22(4):220–6. https://doi.org/10.1038/ijir.2010.7.
Mazzilli R, Imbrogno N, Elia J, Delfino M, Bitterman O, Napoli A, Mazzilli F. Sexual dysfunction in diabetic women: prevalence and differences in type 1 and type 2 diabetes mellitus. Diabetes Metabolic Syndrome and Obesity. 2015;8:97–101. https://doi.org/10.2147/DMSO.S71376.
Rosen R, Brown C, Heiman J, Leiblum S, Meston C, Shabsigh R, Ferguson D, D’ Agostino R Jr. The female sexual function index (FSFI): a multidimensional self-report instrument for the assessment of female sexual function. Journal of Sex & Marital Therapy. 2000;26:191–208. https://doi.org/10.1080/009262300278597.
Rust J, Golombok S. The Golombok-Rust inventory of sexual satisfaction (GRISS). Br J Psychiatry. 1985;24:63–4. https://doi.org/10.1192/bjp.209.1.A3.
Abdo CHN. Elaboração e validação do quociente sexual - versão feminina: uma escala para avaliar a função sexual da mulher. Revista Brasileira de Medicina. 2006;63(9):477–82 (in portuguese).
DeUgarte CM, Berman L, Berman J. Female sexual dysfunction – from diagnosis to treatment. Sexuality, Reproduction and Menopause. 2004;2:139–45. https://doi.org/10.1016/j.sram.2004.07.002.
Basson R, Leiblum S, Brotto L, Derogatis L, Fourcroy J, Fugl-Meye K, Graziottin A, Heiman JR, Laan E, Meston C, Schover L, Van Lankveld J, Schultz WW. Revised definitions of Women's sexual dysfunction. International Society for Sexual Medicine. 2004;1:40–9. https://doi.org/10.1111/j.1743-6109.2009.01238.x.
Basson R, Berman J, Burnett A, Derogatis L, Ferguson D, Fourcroy J, Goldstein I, Graziottin A, Heiman J, Laan E, Leiblum S, Padma-Nathan H, Rosen R, Segraves K, Segraves RT, Shabsigh R, Sipski M, Wagner G, Whipple B. Report of the international consensus development conference on female sexual dysfunction: definitions and classifications. J Urol. 2000;63:888–93. https://doi.org/10.1016/S0022-5347(05)67828-7.
Diagnostic and Statistical Manual of Mental Disorders (DSM–5). American Psychiatric Association, 2013.
The Voice of the Patient. Female Sexual Dysfunction Public Meeting: October 27, 2014 report. Center for Drug Evaluation and Research (CDER)/U.S. Food and Drug Administration (FDA) 2015.
Laumann EO, Paik A, Rosen RC. Sexual dysfunction in the United States: prevalence and predictors. The Journal of American of the Association. 1999;281:537–44. https://doi.org/10.1001/jama.281.6.537.
Abdo CHN, Oliveira WM, Moreira ED, Fittipaldi JAS. Prevalence of sexual dysfunctions and correlated conditions in a sample of Brazilian women. Int J Impot Res. 2004;16:160–6.
Prado DS, Mota VPLP, Lima TIA. Prevalence of sexual dysfunction in two women groups of different socioeconomic status. Revista Brasileira de Ginecologia e Obstetrícia. 2010;32:139–43. https://doi.org/10.4103/0022-3859.52842.
Ferreira ALCG, Souza AI, Amorim MMR. Female sexual dysfunction prevalence in a family planning clinic at a university hospital located in Recife. Pernambuco Revista Brasileira de Saúde Materno Infantil. 2007;7:143–50.
Moreira Jr ED, Brock G, Glasser D B, Nicolosi, A., Laumann, EO, … Paik, A. Help-seeking behaviour for sexual problems: the global study of sexual attitudes and behaviors. Int J Clin Pract, 59(1), 6–16, 2005. doi:https://doi.org/10.1111/j.1742-1241.2005.00382.x.
Nicolosi A, Laumann EO, Glasser DB, Brock G, King R, Gingell C. Sexual activity, sexual disorders and associated help-seeking behavior among mature adults in five anglophone countries from the global survey of sexual attitudes and behaviors (GSSAB). J Sex Marital Ther. 2006;32(4):331–42. https://doi.org/10.1080/00926230600666469.
Rizvi SJ, Yeung NY, Kennedy SH. Instruments to measure sexual dysfunction in community and psychiatric populations. J Psychosom Res. 2011;70:99–109. https://doi.org/10.1016/j.jpsychores.2010.05.009.
Meston CM. Validation of the female sexual function index (FSPI) in women with female orgasmic disorder and women with hypoactive sexual desire disorder. J Sex Marital Ther. 2003;29(1):39–46. https://doi.org/10.1080/713847100.
Raina R, Pahlajani G, Khan S, Gupta S, Agarwal A, Zippe CD. Female sexual dysfunction: classification, pathophysiology, and management. Fertil Steril. 2007;88:1273–84. https://doi.org/10.1016/j.fertnstert.2007.09.012.
Pacagnella RC, Vieira EM, Rodrigues OM, Souza C Jr. Crosscultural adaptation of the female sexual function index. Cadernos de Saúde Pública. 2008;24:416–26. https://doi.org/10.1590/S0102-311X2008000200021.
Pacagnella RC, Martinez EZ, Vieira EM. Construct validity of a Portuguese version of the female sexual function index. Cadernos de Saúde Pública. 2009;25:2333–44. https://doi.org/10.1590/S0102-311X2009001100004.
Swets JA. Measuring the accuracy of diagnostic systems. Science. 1988;240:1285–93 PMID:3287615.
Viera AJ, Garrett JM. Understanding interobserver agreement: the kappa statistic. Fam Med. 2005;37:360–3 15883903.
Zweig MH, Campbell G (1993). Receiver-operating characteristic (ROC) plots: a fundamental evaluation tool in clinical medicine. Clin Chem, 39, 561–577, 1993. PMID: 8472349.
Gerstenberger EP, Rosen RC, Brewer JV, Meston CM, Brotto LA, Wiegel M, Sand M. Sexual desire and the female sexual function index (FSFI): a sexual desire cut point for clinical interpretation of the FSFI in women with and without hypoactive sexual desire disorder. J Sex Med. 2010;7(9):3096–103. https://doi.org/10.1111/j.1743-6109.2010.01871.x.
Hoon EF, Joon PW, Wincze JP. An inventory for the measurement of female sexual arousability: the SAI. Arch Sex Behav. 1976;5(4):269–74.
Symonds T, Boolell M, Quirk F. Development of a questionnaire on sexual quality of life in women. Journal of Sex & Marital Therapy. 2005;31(5):385–97. https://doi.org/10.1080/00926230591006502.
Clayton AH, Segraves RT, Leiblum S, Basson R, Pyke R, Cotton D, et al. Reliability and validity of the sexual interest and desire inventory–female (SIDI-F), a scale designed to measure severity of female hypoactive sexual desire disorder. Journal of Sex & Marital Therapy. 2006;32(2):115–35. https://doi.org/10.1080/00926230500442300.
DeRogatis L, Clayton A, Lewis-D’Agostino D, Wunderlich G, Fu Y. Validation of the female sexual distress scale-revised for assessing distress in women with hypoactive sexual desire disorder. J Sex Med. 2008;5(2):357–64. https://doi.org/10.1111/j.1743-6109.2007.00672.x.
Althof SE, Rosen RC, Perelman MA, Rubio-Aurioles E. Standard operating procedures for taking a sexual history. J Sex Med. 2013;10(1):26–35. https://doi.org/10.1111/j.1743-6109.2012.0282.
Acknowledgements
We would like thank to the participants.
Funding
This work was supported by the Brazilian Council for Scientific and Technological Development (CNPq), Proc. No. 306018/2013–6 and Proc. No. 484972/2013–8 to M.B.C.S. and in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001.
Availability of data and materials
The data are available upon request from the corresponding author.
Author information
Authors and Affiliations
Contributions
CKLC, MHCS, and MBCS were involved in the study conception and design. CKLC conducted the acquisition of data. MHCS performed the data statistical analysis. CKLC, MHCS, and MBCS prepare the manuscript. MBCS revised the manuscript for quality and consistency of the data. CKLC, MHCS, and MBCS have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethical Committee of the Federal University of Rio Grande do Norte and Brazilian Health Ministry, under Protocol number 49859915.0.0000.5178. All participants gave their informed written consent to take part in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
da Costa, C.K.L., Spyrides, M.H.C. & de Sousa, M.B.C. Consistency of three different questionnaires for evaluating sexual function in healthy young women. BMC Women's Health 18, 204 (2018). https://doi.org/10.1186/s12905-018-0693-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12905-018-0693-y