Abstract
Background
While research has explored the risk of periodontal disease in various eye conditions, the link between dry eye and periodontal disease remains underexplored, especially in Japanese adults. This study aims to investigate the association between dry eye and periodontal disease in community-dwelling Japanese adults.
Methods
This study is a subset of the Uonuma cohort study, which includes Japanese adults aged 40 years and older residing in the Uonuma area of Niigata Prefecture, Japan. Participants completed a self-administered, paper-based questionnaire. Statistical analyses, including the chi-square test, independent t test, ANOVA test, and logistic regressions, were employed to assess the association of periodontal disease with independent variables.
Results
Among 36,488 participants (average age 63.3 years, 47.4% men), 39.3% had a history of periodontal disease, and gender differences were statistically significant (p < 0.001). Significant associations were found between periodontal disease and dry eye diagnosis or symptoms. Univariable logistic regression revealed links between periodontal disease and age, gender, living status, alcohol consumption, remaining teeth, bite molar availability, and history of dry eye disease or symptoms. Multiple-adjusted regression found that doctor-diagnosed dry eye was associated with a higher likelihood of periodontal disease (odds ratio, 1.12; 95% confidence interval, 1.03–1.22). Participants who never experienced dryness or foreign body sensation had lower ORs of periodontal disease than those who always experienced such symptoms across all models.
Conclusion
A significant correlation was found between dry eye and periodontal disease in Japanese adults. Regular check-ups, early detection, and effective management of both conditions are strongly recommended.
Similar content being viewed by others
Background
Periodontal disease (PD) is a common disease experienced by an estimated 20.0–50.0% of the global population [1]. It can lead to the destruction of supporting tissues of the teeth in susceptible patients, potentially resulting in eventual tooth loss [2]. Additionally, it stands as a leading cause of tooth loss among Japanese adults affecting 32.4% of those aged 25–34 years, 49.5% of those aged 45–54 years, and 57.5% of those aged 65–74 years [3].
PD is associated with multiple systemic diseases including rheumatoid arthritis, diabetes, adverse pregnancy outcomes, and cardiovascular diseases [4, 5]. The long-term systemic inflammation caused by oral bacteria in patients with PD can affect the entire body through both infectious and inflammatory responses, potentially increasing the risk of systemic diseases [2, 6]. As a result, the impact of PD on general health has been increasing to focus on research interests. Acknowledging that PD is both preventable and irreversible, many countries have initiated efforts to reduce the burden of PD [7].
Similar to PD, several eye diseases are associated with systemic inflammatory pathways, and reports have linked them to PD [8, 9]. Among these diseases, dry eye disease (DED) is one of the most common ocular diseases worldwide, with an estimated prevalence of 11.6% [10]. This condition poses a growing public health concern due to its impact on visual function and quality of life [11]. Common causes of DED include aging, certain medical conditions such as Sjögren’s syndrome, and wearing contact lenses [10].
Sjögren’s syndrome is an autoimmune disease characterized by the cardinal symptoms of dry eye and dry mouth. Several studies have investigated the risk of PD in patients with Sjögren’s syndrome and those with dry mouth, indicating the common inflammatory pathways through systemic inflammatory responses and alterations in pro-inflammatory cytokines [2, 6, 9]. Similarly, DED is also characterized by elevated levels of inflammatory cytokines [10], hinting a potential systemic link between DED and PD. However, the available evidence concerning the association between these conditions remains limited. Furthermore, to the best of our knowledge, there is a lack of information regarding the relationship between DED and PD among Japanese adults. Therefore, this study aims to investigate the association between DED and PD in a community-dwelling Japanese adult population. We hypothesize that individuals with a history of dry eye disease or related symptoms will exhibit a higher prevalence of PD than those without any history of dry eye disease or symptoms.
Methods
Study design and participants
This study is a subset of the Uonuma cohort study, which targeted Japanese adults aged 40 years and older in the Uonuma area of Niigata Prefecture, Japan [12]. The study utilized the results of a self-administered questionnaire survey conducted between 2012 and 2014 as its baseline. All Japanese residents of Minami-Uonuma City and Uonuma City aged 40 years and older (n = 61,762) were invited to complete a questionnaire. Out of them, 39,774 residents (64.4%) responded to the questionnaire. After excluding individuals who withdrew their consent, or provided invalid responses, the study analyzed data from 36,488 residents (59.1%). This study protocol was approved by the Ethics Committee of Niigata University, Japan (Approval number. 2017-0071). All methods were carried out in accordance with the guidelines and regulations established in the Declaration of Helsinki. Participants who agreed to participate in the study signed their written consent forms.
Data collection
Self-administered questionnaires enclosed in sealed envelopes with return envelopes were mailed to the residents in cooperation with the local government authorities. Information regarding their age and gender was obtained from the local government records. Participants completed and returned the questionnaires. The questionnaire included inquiries about body weight and height to calculate the body mass index, BMI (1: healthy, 2: underweight, 3: overweight, or 4: obese), living status (1: with 5 persons and above, 2: with 3–4 persons, 3: with 1–2 persons, or 4: alone), smoking habit (1: never, 2: former smoker, or 3: current smoker), drinking habit (1: never, 2: former drinker, or 3: current drinker), history of PD diagnosed by a dentist (1: no or 2: yes), number of remaining teeth (1: ≥20 teeth, 2: 10–19 teeth, 3: 1–9 teeth, 4: no natural teeth, or 5: don’t know), biting availability on right and left molars or with dentures (1: both sides, 2: one side, or 3: no side), history of DED diagnosed by a doctor (1: no or 2: yes), feeling dryness of eyes (1: never, 2: sometimes, or 3: always), and feeling a foreign body sensation in eyes (1: never, 2: sometimes, or 3: always).
Statistical analysis
We performed statistical analyses using IBM SPSS Statistics for Windows, version 22.0 (SPSS; Chicago, IL, USA). Demographics and general data were reported using descriptive statistics. Participants were classified into two groups: those with a history of PD and those without such a history (0: no history of PD, 1: history of PD). The associations between periodontal disease and independent variables were examined using the chi-square test, independent t test, and ANOVA test. We also employed univariable and multivariable logistic regression analyses to assess the potential risk factors related to PD. Multivariable logistic regression was conducted across a series of models. Model 1 adjusted for sociodemographic variables such as age, gender, BMI, and living status. Model 2 further adjusted for behavioral factors, including smoking and drinking habits. Model 3 extended the adjustments to oral conditions such as the number of remaining teeth and the bite availability on the right and left molars or with dentures. Subsequently, we calculated the 95% confidence interval (95% CI) for each odds ratio (OR) in our logistic regression models. The threshold for statistical significance for all tests was set at p < 0.05.
Results
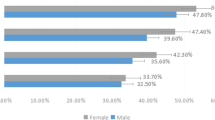
The sample consisted of 36,488 participants, with an average age of 63.3 years, and 47.4% of them were men (n = 17,302). The mean number of present teeth (standard deviation) was 20.6 (9.3) in men and 21.0 (9.0) in women. The general characteristics of the participants are presented in Table 1. Overall, 39.3% of the participants had a history of PD diagnosed by a dentist, and there was a statistically significant difference in PD history between genders (p < 0.001). Gender exhibited a significant association with most variables in our study, excluding questions related to the history of dry eye disease or symptoms and smoking habits.
We observed significant associations between individuals with and without PD and the diagnosis or symptoms of dry eye (Table 2). Among male participants, those who reported experiencing dryness (p = 0.041) or a foreign body sensation in their eyes (p = 0.034) exhibited significantly higher rates of PD history than those without such symptoms. However, these symptoms did not correlate with a history of PD in female participants. Conversely, among female participants, a diagnosis of DED by a doctor was significantly linked to a history of PD (p = 0.014).
Table 3 presents the associations between a history of PD and the diagnosis or symptoms of dry eye, stratified by age groups. In the participants aged 50–59 years, individuals who reported experiencing dryness in their eyes demonstrated significantly increased rates of PD history compared to those without those symptom(p = 0.004). Furthermore, in older adults aged 70–79 years, the occurrence of a foreign body sensation in their eyes exhibited a significant association with a history of PD (p = 0.004).
The findings presented in Table 4 represents the results of the univariable logistic regression analysis for PD. Significant associations with PD were found for sociodemographic factors such as age, gender, and living status. Smoking habits did not influence the likelihood of PD in our study, but alcohol consumption was significantly associated with PD. Participants with ≥ 20 remaining teeth were less likely to have PD than those with 10–19 teeth (OR 1.78; 95% CI, 1.67–1.89), 1–9 teeth (OR 1.83; 95% CI, 1.70–1.97), and no natural teeth (OR 1.42; 95% CI, 1.28–1.58). Additionally, molar bite availability emerged as a significant factor associated with PD history. A history of DED diagnosed by a doctor was associated with a higher likelihood of PD (OR 1.13; 95% CI, 1.04–1.22). Similarly, dry eye symptoms, including dryness and a foreign body sensation, were significantly linked to PD.
Table 5 shows the adjusted ORs for PD. In the variable “history of DED diagnosed by a doctor”, the multiple adjusted ORs for PD were 1.13 (95% CI, 1.04–1.23) for model 1, 1.13 (95% CI, 1.03–1.23) for model 2, and 1.12 (95% CI, 1.03–1.22) for model 3. Furthermore, participants who reported never experiencing dryness or a foreign body sensation in their eyes were significantly less likely to have PD than those who always experienced these symptoms in all models. Conversely, among male participants, only the variable “feeling a foreign body sensation in their eyes” was significantly associated with PD in all models (Supplementary Table 1). Female participants with a history of DED diagnosis were more likely to have PD than those without a DED diagnosis in all models (Supplementary Table 2).
Discussion
Previous studies have explored the potential links between PD and a range of eye diseases [2, 6, 9, 13, 14]. However, the evidence concerning the correlation between PD and dry eye remains limited. To our knowledge, this study represents the first large-scale population-based study into the impact of a history of dry eye disease or related symptoms on PD within the specific context of the Japanese population. Overall, the prevalence of PD in Japanese adults is considered high, with a significant gender difference in its history. However, there was no significant association found between DED and gender. The study revealed a significant association between the diagnosis or symptoms of dry eye and the history of PD among Japanese adults. Furthermore, significant associations were observed between PD and most variables, except for BMI and smoking habit.
Our study demonstrated that a range of DED diagnoses or related symptoms exhibited a significant association with PD, even after adjusting for potential confounding factors. A poorer periodontal status was more prevalent among individuals with a history of DED or related symptoms compared to those without such problems. While the exact causality remains uncertain in the existing literature, plausible explanations, including inflammatory processes, immunological factors, shared risk factors, medication use, and microbial translocation, have been suggested [2, 8, 9, 15,16,17]. In particular, it is worth noting that the inflammatory process, characterized by alterations in the cytokine network, may play a crucial role in linking these two conditions via a common inflammatory pathway [2, 16]. Previous studies have suggested that this pathogenic link might be mediated by shared immune responses and autoimmune diseases such as Sjögren’s syndrome, through the dysregulation of the immune system in both eye diseases and PD, potentially increasing susceptibility to inflammatory conditions [2, 18].
The pathogenesis of DED and PD can also be influenced by various common risk factors. Ageing, certain medications, and comorbidities such as diabetes, hypertension, as well as unhealthy behaviors like cigarette smoking and alcohol consumption, could be implicated in these associations [9, 19]. Dietary factors, such as vitamin deficiencies or imbalances in omega-3 fatty acids, may impact inflammation and contribute to the simultaneous occurrence of dry eye and PD [20, 21]. Moreover, individual factors such as genetics and lifestyle choices can further complicate the relationship between these two conditions. However, it is important to acknowledge that the complete mechanisms underpinning PD and DED are intricate and not yet fully understood. Therefore, further research is necessary to fully comprehend the underlying mechanisms and explore whether effectively managing one condition might have a positive impact on the other. Nevertheless, based on the findings of our study, we strongly advocate for early detection, targeted prevention, and effective management of both conditions. This entails the implementation of a multifaceted approach, encompassing good oral hygiene practices, overall health preservation, and mindful lifestyle choices.
The effects of demographic inequalities on oral health have been well documented. We observed a higher likelihood of PD development among older individuals and men in our study, which is consistent with findings in the literature supporting the widely recognized aging and gender differences in the development of PD [22, 23]. In the present study, it was observed that nearly half of the participants who lived alone had a history of PD, and living status showed a significant association with the likelihood of PD. Living status is recognized as a strong factor influencing individuals’ oral health [24]. Living alone is associated with a higher likelihood of developing depressive symptoms compared to living with family members [25]. Consequently, perceived psychological stressors have been identified as risk indicators for poor oral health, including periodontal diseases [26, 27].
Our study demonstrated that having fewer natural teeth and reduced chewing ability are associated with an increased risk of PD. This phenomenon can be attributed to a reduced self-cleaning mechanism and dietary changes [28]. Individuals with fewer teeth or reduced chewing ability may not effectively remove food remnants, and they may choose softer, processed foods that are higher in sugars and carbohydrates. This can foster the accumulation of plaque and bacteria, which are significant contributors to the development of PD. While the study identified a drinking habit as a significant associated factor for PD, smoking habit did not influence the likelihood of PD in the present study. This is perhaps because our survey only included general questions concerning these variables, omitting the duration and intensity of smoking. Consequently, respondents may have provided inaccurate or misleading responses.
This study has some limitations. First, while the sample is large enough, this study was carried out among Japanese adults residing in the Uonuma area of Niigata Prefecture, Japan. Therefore, this study could not be generalized to the entire Japanese population. Second, the potential presence of information bias may be considered. All measures utilized in this investigation relied on self-perceptions and self-reports. The determination of dry eye and periodontal disease was solely based on participants’ responses, without a current confirmation by a doctor or dentist. Third, this study utilizes data from the baseline of the Uonuma cohort study, which is inherently cross-sectional in design. Consequently, it is not possible to establish the direction of causality between the variables examined. Fourth, we did not perform missing data analysis in this study. Moreover, information pertaining to medication use and comorbidities could not be incorporated. Finally, it is important to acknowledge that in unforeseen circumstances, including delayed inter-researcher agreement, particularly during the COVID-19 pandemic, the completion of this study’s report was significantly delayed. Nevertheless, the study’s findings contribute valuable knowledge regarding the association between dry eye and periodontal disease, as the first large-scale epidemiological survey in Japan.
Conclusion
Our study has revealed a significant correlation between dry eye and periodontal disease, suggesting that individuals with a history of dry eye disease or related symptoms were more likely to be associated with the development of subsequent periodontal disease. These findings underscore the importance of regular check-ups with both eye specialists and dentists, emphasizing the need for early detection and appropriate management of both conditions to ensure optimal health outcomes.
Data Availability
The datasets generated and/or analyzed during the current study are not publicly available due to the restrictions by the Ethics Committee of Niigata University, Japan in order to protect the participants’ privacy but are available from the corresponding author on reasonable request.
Change history
10 February 2024
The typo in the article title has been corrected.
Abbreviations
- PD:
-
Periodontal Disease
- DED:
-
Dry Eye Disease
- BMI:
-
Body Mass Index
- OR:
-
Odds Ratio
- 95% CI:
-
95% Confidence Interval
References
American Academy of Periodontology Task Force report on the update to. The 1999 classification of periodontal Diseases and conditions. J Periodontol. 2015;86(7):835–8.
Lin CY, Tseng CF, Liu JM, Chuang HC, Lei WT, Liu LY, et al. Association between periodontal Disease and subsequent Sjögren’s syndrome: a nationwide population-based cohort study. Int J Environ Res Public Health. 2019;16(5):771.
Ministry of Health, Labour and, Welfare J. 2016 dental disease survey. https://www.mhlw.go.jp/toukei/list/62-28.html. Accessed 22 Sept 2023.
Kapila YL. Oral health’s inextricable connection to systemic health: special populations bring to bear multimodal relationships and factors connecting periodontal Disease to systemic Diseases and conditions. Periodontol 2000. 2021;87(1):11–6.
Ceccarelli F, Saccucci M, Di Carlo G, Lucchetti R, Pilloni A, Pranno N, et al. Periodontitis and rheumatoid arthritis: the same inflammatory mediators? Mediators Inflamm. 2019. https://doi.org/10.1155/2019/6034546.
Chau SF, Lee CY, Huang JY, Chou MC, Chen HC, Yang -F. The existence of periodontal Disease and subsequent ocular Diseases: a population-based cohort study. Medicina. 2020;56(11):621.
Fadl AE, Abdel Fattah RK, Helmi MA, Wassel MA, Badran MO, Elgendi AS. Periodontal Diseases and potential risk factors in Egyptian adult population: results from a national cross-sectional study. PLoS ONE. 2021. https://doi.org/10.1371/journal.pone.0258958.
Klig JE. Ophthalmologic Complications of systemic Disease. Emerg Med Clin North Am. 2008;26(1):217–31.
Pockpa ZA, Struillou X, Coulibaly NT, Weber M, Soueidan A, Badran Z. Potential relationship between periodontal Diseases and eye Diseases. Med Hypotheses. 2017;99:63–6.
Papas EB. The global prevalence of dry eye Disease: a bayesian view. Ophthalmic Physiol Opt. 2021;41(6):1254–66.
Aragona P, Giannaccare G, Mencucci R, Rubino P, Cantera E, Rolando M. Modern approach to the treatment of dry eye, a complex multifactorial Disease: a P.I.C.A.S.S.O. board review. Br J Ophthalmol. 2021;105(4):446–53.
Kabasawa K, Tanaka J, Nakamura K, Ito Y, Yoshida K, Takachi R, et al. Study design and baseline profiles of participants in the Uonuma CKD cohort study in Niigata, Japan. J Epidemiol. 2020;30(4):170–76.
Lv X, Li W, Fang Z, Xue X, Pan C. Periodontal Disease and age-related macular degeneration: a meta-analysis of 112,240 participants. Biomed Res Int. 2020. https://doi.org/10.1155/2020/4753645.
Sun KT, Shen TC, Chen SC, Chang CL, Li CH, Li X, et al. Periodontitis and the subsequent risk of glaucoma: results from the real-world practice. Sci Rep. 2020;10(1):17568.
Badran Z, Struillou X, Verner C, Clee T, Rakic M, Martinez MC, et al. Periodontitis as a risk factor for systemic Disease: are microparticles the missing link? Med Hypotheses. 2015;84(6):555–6.
Martínez-García M, Hernández-Lemus E. Periodontal inflammation and systemic Diseases: an overview. Front Physiol. 2021;12:709438.
Genco RJ, Borgnakke WS. Risk factors for periodontal Disease. Periodontol 2000. 2013;62(1):59–94.
Negrini S, Emmi G, Greco M, Borro M, Sardanelli F, Murdaca G, Indiveri F, Puppo F. Sjögren’s syndrome: a systemic autoimmune Disease. Clin Exp Med. 2022;22(1):9–25.
Knight ET, Liu J, Seymour GJ, Faggion CM Jr, Cullinan MP. Risk factors that may modify the innate and adaptive immune responses in periodontal Diseases. Periodontol 2000. 2016;71(1):22–51.
Jo YJ, Lee JS. Effects of dietary high dose DHA omega-3 supplement in dry eye with meibomian gland dysfunction. Int J Ophthalmol. 2021;14(11):1700–6.
Santonocito S, Polizzi A, Palazzo G, Indelicato F, Isola G. Dietary factors affecting the prevalence and impact of Periodontal Disease. Clin Cosmet Investig Dent. 2021;13:283–92.
Clark D, Kotronia E, Ramsay SE. Frailty, aging, and periodontal Disease: Basic biologic considerations. Periodontol 2000. 2021;87(1):143–56.
Lipsky MS, Su S, Crespo CJ, Hung M. Men, and oral health: a review of sex and gender differences. Am J Mens Health. 2021;15(3):15579883211016361.
Nakahara M, Ekuni D, Kataoka K, Yokoi A, Uchida-Fukuhara Y, Fukuhara D, et al. Living with family is directly associated with regular dental checkup and indirectly associated with gingival status among Japanese university students: a 3-year cohort study. Int J Environ Res Public Health. 2021;18(1):324.
Stahl ST, Beach SR, Musa D, Schulz R. Living alone and depression: the modifying role of the perceived neighborhood environment. Aging Ment Health. 2017;21(10):1065–71.
López R, Ramírez V, Marró P, Baelum V. Psychosocial distress and periodontitis in adolescents. Oral Health Prev Dent. 2012;10(3):211–8.
Thwin KM, Lin WT, Takehara S, Ogawa H. Socioeconomic, behavioral, and psychological factors related to oral health in Myanmar: a cross-sectional study. J Public Health Dent. 2023. https://doi.org/10.1111/jphd.12585.
Lertpimonchai A, Rattanasiri S, Arj-Ong Vallibhakara S, Attia J, Thakkinstian A. The association between oral hygiene and periodontitis: a systematic review and meta-analysis. Int Dent J. 2017;67(6):332–43.
Acknowledgements
The authors would like to thank local authorities and personnel who assisted in the study for their kind support.
Funding
This study was financially supported by the Health and Labor Sciences Research Grant (grant number: 21FA1013), and Grants-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (grant numbers: 17K17367, 18H03013, and 19K10421).
Author information
Authors and Affiliations
Contributions
Conceptualization and study design: Noboru Kaneko, Takayuki Yamaga, Kana Suwama, Akihiro Yoshihara, Masanori Iwasaki, Hiroshi Ogawa. Data collection: Akihiro Yoshihara, Yumi Ito, Junta Tanaka, Ichiei Narita. Data cleaning and verification: Noboru Kaneko, Takayuki Yamaga, Hikaru Okubo. Data analysis and interpretation: Kaung Myat Thwin. Drafting the initial manuscript: Kaung Myat Thwin, Noboru Kaneko, Hikaru Okubo. Approval of the final manuscript: All authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study protocol was approved by the Ethics Committee of Niigata University, Japan (Approval number. 2017-0071). The participants who agreed to participate in the study signed their written consent forms. All methods were carried out in accordance with the guidelines and regulations established in the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The original online version of this article was revised due to typo in the article title has been corrected.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Thwin, K.M., Kaneko, N., Okubo, H. et al. Association between dry eye and periodontal disease in community-dwelling Japanese adults: data from the Uonuma cohort study. BMC Oral Health 24, 47 (2024). https://doi.org/10.1186/s12903-023-03773-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12903-023-03773-7