Abstract
Background
Early prediction of tracheostomy in traumatic cervical spinal cord injury (TCSCI) patients is often difficult. This study aims to clarify the association between shoulder abductor strength (SAS) and tracheostomy in patients with TCSCI.
Methods
We retrospectively analyzed 513 TCSCI patients who were treated in our hospital. All patients were divided into a tracheostomy group and a non-tracheostomy group. The SAS was assessed using the Medical Research Council (MRC) Scale for Muscle Strength grading. Potential predictors were assessed for their association with tracheostomy in patients. A nomogram was developed based on multivariable logistic regression analysis (MLRA) to visualize the predictive ability of the SAS. Validation of the nomogram was performed to judge whether the nomogram was reliable for visual analysis of the SAS. Receiver operating characteristics curve, specificity, and sensitivity were also performed to assess the predictive ability of the SAS.
Results
The proportion of patients with the SAS grade 0–2 was significantly higher in the tracheostomy group than in the non-tracheostomy group (88.1% vs. 54.8%, p = 0.001). The SAS grade 0–2 was identified as a significant predictor of the tracheostomy (OR: 4.505; 95% CI: 2.080–9.758; p = 0.001). Points corresponding to both the SAS grade 0–2 and the neurological level of injury at C2-C4 were between 60 and 70 in the nomogram. The area under the curve for the SAS grade 0–2 was 0.692. The sensitivity of SAS grade 0–2 was 0.239. The specificity of SAS grade 0–2 was 0.951.
Conclusions
SAS is a novel predictor of tracheostomy in patients after TCSCI. The SAS grade 0–2 had a good predictive ability of tracheostomy.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Traumatic cervical spinal cord injury (TCSCI) is a catastrophic injury that can lead to motor and sensory dysfunction, and in severe cases, death [1]. Pulmonary complications are the main cause and even the primary cause of death after TCSCI [2, 3]. So, mechanical ventilation and tracheostomy are required in some patients with TCSCI [4]. Early tracheostomy can increase patient comfort, improve respiratory complications, reduce the number of ventilator days, and shorten Intensive Care Unit (ICU) and hospital stays [5,6,7,8,9]. To take advantage of these benefits and allocate resources accordingly, it is important for surgeons to have a tool to predict whether a patient might need a tracheostomy. However, early prediction of tracheostomy in patients with TCSCI has so far been often difficult [10]. Many scholars have studied the risk factors for tracheostomy after TCSCI, the results showed that forced vital capacity, neurological level of injury (NLI) at C4 or above, MRI scans showing hematoma-like changes, smoking history, advanced age, and an American Spinal Injury Association (ASIA) grade A are all risk factors [11,12,13,14]. However, these indicators have some limitations: the clinical application is cumbersome; those who suffer great injury had to receive a tracheostomy may not have acceptable and reproducible pulmonary function test results [15], and there is no standardized bedside predictor.
Previous studies have shown that a grade of ASIA A and an injury level above C4 are the most common predictors of tracheostomy [16, 17]. The shoulder abduction is accomplished by the deltoid in conjunction with the supraspinatus [18]. The deltoid is innervated by the axillary nerve, and the supraspinatus is innervated by the suprascapular nerve. Interestingly, the cervical spinal cord innervating the axillary nerve has some overlap with the cervical spinal cord innervating the phrenic and intercostal nerves, respectively. And the cervical spinal cord innervating the suprascapular nerve also has some overlap with the cervical spinal cord innervating the phrenic and intercostal nerves, respectively. Meanwhile, we believe that the shoulder abductor strength (SAS) is related to the ASIA grade and the NLI to some extent. So, we hypothesize that the SAS may be a novel predictor for tracheostomy after TCSCI. The purpose of this study was to clarify the association between the SAS and the tracheostomy in patients with TCSCI. To the best of our knowledge, this is the first study to investigate the association between the SAS and the tracheostomy in patients with TCSCI.
Methods
Patients and data collection
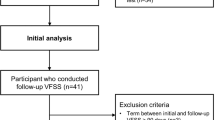
This retrospective study reviewed the electronic medical records of patients with TCSCI who were treated in our hospital from October 2010 to October 2020. All assessments were performed by experienced senior physicians on admission. The assessment of SAS was also performed by experienced senior physicians at the time of admission. The decision to perform a tracheostomy was made by the spine surgeon in conjunction with the ICU physician and was made when prolongation of the mechanical ventilation (MV) was expected, considering the patient's neurologic function, respiratory function, age, concomitant injury, and other factors. Tracheostomy was performed if any of the following criteria were met: (1) the patient was retained in a transoral tracheal tube and failed to evacuate mechanical ventilation after several attempts; (2) the patient had a lot of sputum and poor coughing power, requiring retention of an artificial airway to drain sputum. The inclusion criteria were as follows: (1) clear history of trauma, (2) well-diagnosed cervical spinal cord injury (SCI), and (3) complete medical records. The exclusion criteria were as follows: (1) brachial plexus injury, (2) severe brain injury, (3) multiple traumas, such as rib fractures, hemothorax, and pneumothorax, etc., (4) acute pulmonary trauma, and (5) pulmonary complications (e.g., aspiration pneumonia) and history of lung disease such as chronic obstructive pulmonary disease (COPD). A total of 513 patients were enrolled, of whom 84 underwent tracheostomy.
Data including sex, age, smoking history, ASIA impairment scale grade, NLI, and the SAS were recorded. The SAS was assessed using manual muscle testing, based on the Medical Research Council (MRC) Scale for Muscle Strength grading: total paralysis (grade 0); palpable or visible contraction (grade 1); active movement, full range of motion with gravity eliminated (grade 2); active movement, full range of motion against gravity (grade 3); active movement, full range of motion against moderate resistance (grade 4); and (normal) active movement, full range of motion against full resistance (grade 5) [19]. ASIA impairment scale grade was assessed using the American Spinal Injury Association (ASIA) standards [20]. According to our previous clinical experience, the SAS was divided into two groups: grade 0–2 and grade 3–5. Referring to the previous literature, ASIA grade was divided into two groups: grade A and grade B-D, and NLI was divided into C2-C5 and C6-C8 [21,22,23].
Statistical analysis
Pearson’s chi-squared test was used to determine whether there was a difference in recorded categorical variables between the tracheostomy and non-tracheostomy groups. Spearman's rank correlation coefficient was calculated to determine the relationship between tracheostomy and the SAS. MLRA was subsequently performed to identify the predictors which is closely related to the prediction of tracheostomy. The nomogram for tracheostomy was constructed for visualization the predictive ability of the SAS.
Sensitivity and specificity of the SAS were calculated. Receiver operating characteristic (ROC) curves were established to evaluate the performance of the SAS and nomogram. In order to judge whether the visual analysis of SAS by nomogram is reliable, the nomogram was also evaluated: the area under the curve (AUC) and C-index were calculated to test the discrimination of nomogram for tracheostomy. An internal calibration curve was also established to calibrate and assess the predictive ability of the nomogram. We also performed a ROC analysis of ASIA plus NLI together to predict tracheostomy and a ROC analysis of ASIA and NLI plus SAS together to predict tracheostomy. All analyses and nomogram development were performed using R software (version 4.2.0). Statistical significance was set at p < 0.05.
Results
Demographics
A total of 513 patients were included in this study. The mean time interval between performing a tracheostomy and injury was 6.88 ± 3.18 days. The baseline characteristics of the included patients with TCSCI are shown in Table 1. Of these 513 patients (413 males and 100 females), 179 (34.9%) had a history of smoking. In terms of neurologic status, 174 (33.9%) patients were classified as having ASIA grade A, 116 (22.6%) ASIA grade B, 127 (24.8%) ASIA grade C, and 96 (18.7%) ASIA grade D. The most common NLI was C5 (n = 150, 29.2%), followed by C6 (n = 115, 22.4%), then C4 (n = 112, 21.8%). Among all patients, the SAS grade was as follows: 216 patients (42.1%) had grade 0, 67 (13.1%) grade 1, 26 (5.1%) grade 2, 101 (19.7%) grade 3, 47 (9.2%) grade 4, and 56 (10.9%) grade 5.
In the present study, 84 (16.4%) patients with TCSCI underwent tracheostomy. The comparison of patients who underwent tracheostomy and those who did not is shown in Table 2. The tracheostomy group had a significantly higher proportion of patients that were of advanced age (35.7% vs. 25.2%, p = 0.046). At neurological status, there were statistically significant differences in the NLI at C2-C5 (71.4% vs. 52.4%, p = 0.001), and ASIA grade A (61.9% vs. 28.4%, p = 0.001) between tracheostomy and non-tracheostomy group. The proportion of patients with the SAS grade 0–2 was significantly higher in the tracheostomy group than in non-tracheostomy group (88.1% vs. 54.8%, p = 0.001). There were also significantly more patients who have smoking history in the tracheostomy group (p = 0.001).
The SAS and tracheostomy rate
Regarding the SAS, 26.4%, 19.4%, and 15.4% of patients with grade 0, grade 1 and grade 2 muscle strength, respectively, underwent tracheostomy. The proportions of patients with the SAS of grades 3, 4, and 5 who underwent tracheostomy were 4.0%, 6.4%, and 5.4%, respectively. The percentage of tracheostomies in patients with TCSCI was correlated with the distribution of the SAS. Overall, the percentage of patients requiring tracheostomy decreased as the SAS grade increased (γ = -0.829, p = 0.042) (Table 3).
The SAS and other predictors in the nomogram
The results of the MLRA showed that ASIA A (OR = 11.344, p = 0.001), NLI at C2-C5 (OR = 4.533, p = 0.001), the SAS grade 0–2 (OR = 4.505, p = 0.001) and age > 60 (OR = 1.898, p = 0.048) were significantly associated with predicting the tracheostomy (Table 4). These predictors and smoking history (OR = 1.798, p = 0.051) were included in the nomogram for visual analysis of the effects of the SAS on tracheostomy. In the nomogram, each factor was given a point, and the total number of points was calculated, which corresponded to the risk of tracheostomy. The important finding was that, the points corresponding to the SAS grade 0–2 were between 60 and 70, which suggested that the SAS had pretty good predictive capabilities of tracheostomy. ASIA A carried the most weight, and its corresponding number of points was 100 in the nomogram. The points corresponding to the NLI at C2-C5 were second only to ASIA A, which reflected the NLI had an important impact on the prediction of tracheostomy (Fig. 1).
Nomogram to predict the risk of tracheostomy after cervical spinal cord injury. The patient’s score for each risk predictor is plotted on the appropriate scale and vertical lines are drawn from that value to the top points scale to obtain the corresponding scores. All scores are summed to obtain the total points score. The total points score is plotted on the bottom Total Points scale. The corresponding value shows the predicted probability of tracheostomy. C-index = 0.881, SD = 0.039, P < 0.05
The evaluation of the SAS
The nomogram was firstly evaluated. The C-index of the nomogram was 0.881 (SD = 0.039, p < 0.05). The ROC curve used to evaluate the performance of the nomogram is shown in Fig. 2. The AUC value was 0.881 (sensitivity = 0.807, specificity = 0.798). The internal calibration curve is shown in Fig. 3. The calibration curves revealed satisfactory consistency, indicating that the nomogram had excellent calibration capabilities. Therefore, the visual analysis of the predictive ability of the SAS for tracheostomy by nomogram was reliable.
Further, to examines the predictive value of the SAS for the tracheostomy, the ROC curve analysis was performed. As shown in Fig. 4, the area under the curve for the SAS grade 0–2 was 0.692. The sensitivity of the SAS grade 0–2 was 0.239. The specificity of the SAS grade 0–2 was 0.951. These findings suggest that the SAS grade 0–2 could predict tracheostomy in patients with TCSCI, providing valuable information for the physicians to make treatment decisions. The comparison of the SAS with ASIA and NLI was also performed. The area under the curve for ASIA A was 0.735. The sensitivity of ASIA A was 0.299. The specificity of ASIA A was 0.906. The area under the curve for NLI at C2-C5 was 0.724. The sensitivity of NLI at C2-C5 was 0.211. The specificity of NLI at C2-C5 was 0.895. In Fig. 5A, using only ASIA grade A and NLI at C2-C5 to predict tracheostomy, the AUC was 0.831. In Fig. 5B, using ASIA grade A and NLI at C2-C5 plus SAS grade 0–2 together to predict tracheostomy, the AUC was 0.866.
Discussion
The SAS grade can be easily assessed using manual muscle test without complicated auxiliary examinations. The manual muscle test has previously been proven to be a reliable and valid examination tool for clinical applications [24]. Consistent with our approach, Sho Ishiwata also used the manual muscle test in one study to measure the SAS [18]. The nomogram clearly showed that a SAS grade 0–2 had a strong predictive ability: the weight was high, and the corresponding points were between 60 and 70. This demonstrates that the SAS is a simple, practical, and reliable predictor of tracheostomy in patients with TCSCI.
The reason of the SAS as a predictor is that, we believe, it combines the characteristics of ASIA Impairment Scale grade and NLI. Respiratory physiology indicates that the central nervous system regulates breathing through the phrenic nerve that controls the diaphragm (the most important respiratory dynamic muscle), and the intercostal nerve controls the intercostal muscle (the secondary auxiliary respiratory dynamic muscle). The shoulder abduction is performed by the deltoid and supraspinatus. The deltoid muscle is completely innervated by the axillary nerve, which arises from segments C4-C6 [25]. The supraspinatus is innervated by the suprascapular nerve, which arises from C5-C6 [26]. Banneheka found that the origin of the phrenic nerve is from segments C3-C5 [27]. The cervical spinal cord segments innervating the intercostal nerves are C4-C5 [28]. The cervical spinal cord innervating the axillary nerve has some overlap with the cervical spinal cord innervating the phrenic and intercostal nerves, respectively. And the cervical spinal cord innervating the suprascapular nerve also has some overlap with the cervical spinal cord innervating the phrenic and intercostal nerves, respectively. Therefore, we speculated that in some emergency situations, the SAS may be used to indirectly and roughly assess the function of the diaphragm and intercostal muscles. This provides an anatomical basis of SAS as a predictor of tracheostomy.
The SAS as a predictor of tracheostomy has several advantages. One advantage is that its predictive ability is considerable, Third to AIS A and NLI at C2-C5. Another advantage is that its clinical application is very simple. Additionally, the SAS can not only be anatomically connected with the phrenic nerve and intercostal nerve, but can also express the severity of cervical SCI to some extent. Therefore, in case of an emergency, the SAS could be used to predict tracheostomy in patients with TCSCI as a simple, practical, and reliable tool.
The ASIA Impairment Scale grade and the level of C5 injury have been shown the most two important risk factors for tracheostomy in patients with TCSCI [11, 13, 14, 29,30,31]. The present study was consistent with these researches, The OR of ASIA A, the NLI at C2-C5 and the SAS grade 0–2 were 11.344, 4.544 and 4.505, respectively. The AUC of ASIA A, the NLI at C2-C5 and the SAS grade 0–2 were 0.735, 0.724 and 0.692, respectively. In the nomogram, both the SAS grade 0–2 and NLI at C2-C5 corresponded to a score of 60–70, while ASIA grade A corresponded to a score of 100. Compared with the ASIA grade A and the NLI at C2-C5, it demonstrated that the SAS is less predictive of tracheostomy than these two classical factors. However, in some cases, the shoulder abductor strength is also a simple and practical predictor.
Although SAS grade 0–2 is a weaker predictor of tracheostomy than ASIA grade A and NLI at C2-C5, SAS is not intended to replace ASIA or NLI, but rather SAS serves as a new predictor of tracheostomy that complements ASIA, NLI, and other predictors in predicting tracheostomy in TCSCI patients, and together with other predictors predict tracheostomy, allowing for more accurate clinical prediction. This purpose can also be illustrated in the results of this study Fig. 5A and B. In Fig. 5A, using only ASIA grade A and NLI at C2-C5 to predict tracheostomy, an AUC of 0.831 was obtained for the ROC analysis. In contrast, in Fig. 5B, the AUC of the ROC analysis obtained using ASIA grade A and NLI at C2-C5 plus SAS grade 0–2 together to predict tracheostomy was 0.866. This demonstrated that SAS increased the AUC for predicting tracheostomy and that SAS can be clinically helpful in predicting tracheostomy in patients with TCSCI. To make a clinical prediction of tracheostomy more accurate, the more predictors the better. Therefore, this is of great significance that we demonstrated that SAS, a simple and reliable bedside indicator, is a new predictor of tracheostomy.
There are three main limitations to this study. First, this is a retrospective study with a limited level of evidence. Second, the relationship between the shoulder abduction and the respiratory muscles needs further neurophysiological experiments to determine. Third, this study reflected only the experience of a single-specialty spine injury center. Future prospective studies are needed to verify the relationship between the SAS and tracheostomy in patients after TCSCI.
Conclusion
The SAS was shown to be a novel predictor of tracheostomy in patients after TCSCI. The SAS grade 0–2 had a good predictive ability of tracheostomy. This simple predictor can assist clinicians in making decisions about tracheostomy at the bedside.
Availability of data and materials
There is identifiable personal information in the data, so the data generated and analyzed during the study are not publicly available. But data are available from the authors upon reasonable request. If anyone would like to request the data from this study, please contact the corresponding author of this study, Zhengfeng Zhang, M.D., Ph.D. (e-mail address: zhangz3@126.com).
References
Jin GX, Li L, Cui SQ, Duan JZ, Wang H. Persistent hypoalbuminemia is a predictor of outcome in cervical spinal cord injury. Spine J. 2014;14(9):1902–8.
Lemons V, Wagner F. Respiratory complications after cervical spinal cord injury. Spine. 1994;19(20):2315–20.
Hagen EM, Lie SA, Rekand T, Gilhus NE, Gronning M. Mortality after traumatic spinal cord injury: 50 years of follow-up. J Neurol Neurosurg Psychiatry. 2010;81(4):368–73.
Arora S, Flower O, Murray N, Lee B. Respiratory care of patients with cervical spinal cord injury: a review. Crit Care Resusc J Australas Acad Crit Care Med. 2012;14(1):64–73.
Lee D, Park C, Carriere K, Ahn J. Classification and regression tree model for predicting tracheostomy in patients with traumatic cervical spinal cord injury. Eur Spine J. 2017;26(9):2333–9.
Anand T, Hanna K, Kulvatunyou N, Zeeshan M, Ditillo M, Castanon L, Tang A, Gries L, Joseph B. Time to tracheostomy impacts overall outcomes in patients with cervical spinal cord injury. J Trauma Acute Care Surg. 2020;89(2):358–64.
Armstrong P, McCarthy M, Peoples J. Reduced use of resources by early tracheostomy in ventilator-dependent patients with blunt trauma. Surgery. 1998;124(4):763–6.
Ball P. Critical care of spinal cord injury. Spine. 2001;26:S27-30.
Brook A, Sherman G, Malen J, Kollef M. Early versus late tracheostomy in patients who require prolonged mechanical ventilation. Am J Crit Care. 2000;9(5):352–9.
Hou Y, Lv Y, Zhou F, Tian Y, Ji H, Zhang Z, Guo Y. Development and validation of a risk prediction model for tracheostomy in acute traumatic cervical spinal cord injury patients. Eu Spine. 2015;24(5):975–84.
Mu Z, Zhang Z. Risk factors for tracheostomy after traumatic cervical spinal cord injury. J Orthop Surg (Hong Kong). 2019;27(3):2309499019861809.
Higashi T, Eguchi H, Wakayama Y, Sumi M, Saito T, Inaba Y. Analysis of the risk factors for tracheostomy and decannulation after traumatic cervical spinal cord injury in an aging population. Spinal cord. 2019;57(10):843–9.
Tanaka J, Yugue I, Shiba K, Maeyama A, Naito M. A study of risk factors for tracheostomy in patients with a cervical spinal cord injury. Spine. 2016;41(9):764–71.
Yugué I, Okada S, Ueta T, Maeda T, Mori E, Kawano O, Takao T, Sakai H, Masuda M, Hayashi T, et al. Analysis of the risk factors for tracheostomy in traumatic cervical spinal cord injury. Spine. 2012;37(26):E1633-1638.
Alyson Kelley EG, Gross ER, Lieberman SL, Tun CG, Brown R. Spirometry testing standards in spinal cord injury. Chest. 2003;123(3):725–30.
Leelapattana P, Fleming J, Gurr K, Bailey S, Parry N, Bailey C. Predicting the need for tracheostomy in patients with cervical spinal cord injury. J Trauma Acute Care Surg. 2012;73(4):880–4.
Romero J, Vari A, Gambarrutta C, Oliviero A. Tracheostomy timing in traumatic spinal cord injury. Eur Spine J. 2009;18(10):1452–7.
Ishiwata S, Iizuka Y, Shitara H, Mieda T, Takasawa E, Tsunoda D, Kakuta Y, Honda A, Ito S, Inomata K et al: The Association Between the Rotator Cuff Status and the Severity and Recovery of Weakness in the Shoulder Abductor Strength in a Case of Proximal Type Cervical Spondylotic Amyotrophy. Global Spine J 2020:2192568220980441.
Maynard F, Bracken M, Creasey G, Ditunno J, Donovan W, Ducker T, Garber S, Marino R, Stover S, Tator C, et al. International standards for neurological and functional classification of spinal cord injury American spinal injury association. Spinal cord. 1997;35(5):266–74.
F M Maynard Jr MBB, G Creasey, J F Ditunno Jr, W H Donovan, T B Ducker, S L Garber, R J Marino, S L Stover, C H Tator, R L Waters, J E Wilberger, W Young: International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. spinal cord 1997.
McCully BH, Fabricant L, Geraci T, Greenbaum A, Schreiber MA, Gordy SD. Complete cervical spinal cord injury above C6 predicts the need for tracheostomy. Am J Surg. 2014;207(5):664–8 discussion 668-669.
Long PP, Sun DW, Zhang ZF. Risk factors for tracheostomy after traumatic cervical spinal cord injury: a 10-year study of 456 patients. Orthop Surg. 2022;14(1):10–7.
Branco BC, Plurad D, Green DJ, Inaba K, Lam L, Cestero R, Bukur M, Demetriades D. Incidence and clinical predictors for tracheostomy after cervical spinal cord injury: a National Trauma Databank review. J Trauma. 2011;70(1):111–5.
Cuthbert S, Goodheart G. On the reliability and validity of manual muscle testing: a literature review. Chiropr Osteopat. 2007;15:4.
Moser T, Lecours J, Michaud J, Bureau N, Guillin R, Cardinal É. The deltoid, a forgotten muscle of the shoulder. Skeletal Radiol. 2013;42(10):1361–75.
Basta M ST, Varacallo M: Anatomy, Shoulder and Upper Limb, Suprascapular Nerve. 2021 Oct 9.
Banneheka S. Morphological study of the ansa cervicalis and the phrenic nerve. Anat Sci Int. 2008;83(1):31–44.
Nicaise C, Hala TJ, Frank DM, Parker JL, Authelet M, Leroy K, Brion JP, Wright MC, Lepore AC. Phrenic motor neuron degeneration compromises phrenic axonal circuitry and diaphragm activity in a unilateral cervical contusion model of spinal cord injury. Exp Neurol. 2012;235(2):539–52.
Wang Y, Guo Z, Fan D, Lu H, Xie D, Zhang D, Jiang Y, Li P, Teng H. A meta-analysis of the influencing factors for tracheostomy after cervical spinal cord injury. Biomed Res Int. 2018;2018:5895830.
Childs B, Moore T, Como J, Vallier H. American spinal injury association impairment scale predicts the need for tracheostomy after cervical spinal cord injury. Spine. 2015;40(18):1407–13.
Como JJ, Sutton ER, McCunn M, Dutton RP, Johnson SB, Aarabi B, Scalea TM. Characterizing the need for mechanical ventilation following cervical spinal cord injury with neurologic deficit. J Trauma. 2005;59(4):912–6 discussion 916.
Acknowledgements
We thank all participants in this study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Yunbo Jian: manuscript writing, research design, data collection, statistical analysis; Zhiping Mu: data collection, research design; Dawei Sun: statistical analysis, data collection; Dan Zhang: statistical analysis; Chunmei Luo: paper review; Zhengfeng Zhang: paper review, research design. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research protocol complied with the ethical guidelines of the Declarations of Helsinki and was approved by the Medical Ethics Committee of Second Affiliate Hospital of Army Medical University with special ID 2021–165-01. We obtained informed consent for participation from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Jian, Y., Mu, Z., Sun, D. et al. The shoulder abductor strength is a novel predictor of tracheostomy in patients with traumatic cervical spinal cord injury. BMC Musculoskelet Disord 23, 1029 (2022). https://doi.org/10.1186/s12891-022-05988-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05988-1