Abstract
Background
Although treatment options for rheumatoid arthritis (RA) have evolved significantly since the introduction of biologic agents, degenerative lumbar disease in RA patients remains a major challenge. Well-controlled comparisons between RA patients and their non-RA counterparts have not yet been reported. The objective of the present study was to compare postoperative outcomes of lumbar spine surgery between RA and non-RA patients by a retrospective propensity score-matched analysis.
Methods
Patients who underwent primary posterior spine surgery for degenerative lumbar disease in our prospective multicenter study group between 2017 and 2020 were enrolled. Demographic data including age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) physical status classification, diabetes mellitus, smoking, steroid usage, number of spinal levels involved, and preoperative patient-reported outcome (PRO) scores (numerical rating scale [NRS] for back pain and leg pain, Short Form-12 physical component summary [PCS], EuroQOL 5-dimension [EQ-5D], and Oswestry Disability Index [ODI]) were used to calculate a propensity score for RA diagnosis. One-to-one matching was performed and 1-year postoperative outcomes were compared between groups.
Results
Among the 4567 patients included, 90 had RA (2.0%). RA patients in our cohort were more likely to be female, with lower BMI, higher ASA grade and lower current smoking rate than non-RA patients. Preoperative NRS scores for leg pain, PCS, EQ-5D, and ODI were worse in RA patients. Propensity score matching generated 61 pairs of RA and non-RA patients who underwent posterior lumbar surgery. After background adjustment, RA patients reported worse postoperative PCS (28.4 vs. 37.2, p = 0.008) and EQ-5D (0.640 vs. 0.738, p = 0.03), although these differences were not significant between RA and non-RA patients not on steroids.
Conclusions
RA patients showed worse postoperative quality of life outcomes after posterior surgery for degenerative lumbar disease, while steroid-independent RA cases showed equivalent outcomes to non-RA patients.
Similar content being viewed by others
Background
Rheumatoid arthritis (RA) is a systemic inflammatory disease that involves multiple joints [1]. Synovitis leading to joint destruction is well known to involve major weight-bearing joints such as the knees and ankles. RA also affects the spine by damaging the synovium in facet joints. Classically, atlantoaxial instability is one of the pathognomonic changes seen in RA patients [2]. In recent years, treatment options for RA have significantly evolved. Disease-modifying antirheumatic agents including methotrexate (MTX) and biologics such as Tissue Necrosis Factor alpha (TNF-α) inhibitors and Janus kinase (JAK) inhibitors have drastically changed the prognosis of joint destruction [3]. As for spinal pathology, atlantoaxial instability and subsequent basilar invagination are also known to be significantly suppressed following introduction of biologics [4].
The lumbar spine is not exempt from the destruction seen in RA [5, 6]. RA in the lumbar spine manifests as spinal canal stenosis as well as back pain and spondylolisthesis caused by joint instability [7]. In particular, spondylolisthesis has been reported more frequently in RA patients than in the general population, possibly due to facet joint erosion [8, 9]. Despite tremendous success in the treatment of cervical spine pathologies in RA, degenerative lumbar disease in RA remains a major challenge. Lumbar spondylopathy has also become a significant burden as a growing issue among RA patients with the improvements in activities of daily living seen in the era of biologics [10].
In addition to the complexity of spinal pathology, RA patients also suffer a higher rate of complications such as vertebral fractures, surgical site infection and revisions required following spinal surgery [11,12,13]. This has been attributed to impaired bone strength related to inflammation and steroid usage, immunosuppression due to RA treatment and progressive erosion of the facet joints. While outcomes in RA patients undergoing lumbar spinal surgery have been studied [11, 12, 14,15,16], well-controlled comparisons between RA patients and their non-RA counterparts have yet to be reported. Complicating such comparisons is the fact that background health status and the pathologies found in lumbar spondylopathy differ between these two groups. The objective of the present study was to compare postoperative outcomes after lumbar spine surgery between RA and non-RA patients.
Methods
Patient sample and outcome measurements
Patients > 20 years old who underwent posterior spine surgery as a primary procedure for degenerative lumbar disease in our prospective multicenter study group (the University of Tokyo Spine Group) between 2017 and 2020 were enrolled. Demographic data including age, sex, body mass index (BMI), American Society of Anesthesiologists (ASA) physical status classification, diabetes mellitus, rheumatoid arthritis, smoking, steroid usage, and number of spinal levels involved were investigated. Surgical details including fusion level, operation time, and estimated blood loss were recorded. Patient-reported outcome (PRO) scores were also collected preoperatively by distributing questionnaires including a numerical rating scale (NRS) for back pain, NRS for leg pain, 12-item Short Form (SF-12) physical component summary (PCS) [17], EuroQOL 5-dimension (EQ-5D) [18], and Oswestry Disability Index (ODI) [19]. Complications occurring within 30 days after surgery were recorded and categorized as neurological, surgical site infection, hematoma, implant-related, organ damage, respiratory, urinary tract infection, cardiovascular/cerebrovascular, in-hospital death, or other. All patients were encouraged to attend the 1-year follow-up appointment and to complete the same PRO questionnaires.
Propensity score-matched analysis
To make comparisons between RA and non-RA patients adjusted for preoperative background factors, propensity score matching was performed. Propensity score-matched analysis is widely used in cohort studies to adjust for confounding biases [20]. With this statistical approach, propensity scores estimate the probability of a patient being diagnosed with RA based on patient characteristics. Propensity scores were calculated from logistic regression models. In the present study, demographic data (age, sex, BMI, ASA classification, diabetes mellitus, smoking, and number of spinal levels involved) as well as preoperative PRO scores (NRS back pain, NRS leg pain, PCS, EQ-5D, and ODI) were used to calculate a propensity score for RA diagnosis. Fusion was not used as a variable because this was a resultant treatment option rather than a background factor discriminating RA and non-RA. Next, one-to-one matching was performed to match one patient with RA to another non-RA patient with the same propensity score, representing comparable background characteristics. The pairing was performed with the caliper tolerance of 20% of standard deviation of propensity score, and a random selection was made among the patients with the same propensity score. RA and non-RA patients were gathered to form two groups with similar backgrounds for comparison. Matched RA patients were further investigated for pre-operative serum C-reactive protein (CRP), steroid dosage, MTX and biologic use. One-year postoperative PRO scores and 30-day complication rates were compared between groups.
Statistical analyses
All analyses were carried out using the IBM SPSS Statistics version 26 (IBM Corp., Armonk, NY). To analyze differences between groups, a paired t-test, Wilcoxon signed-rank test, or Mann–Whitney U-test was used for continuous variables and McNemar’s test or Chi-square test was used for categorical variables. For comparisons among three groups, the Kruskal–Wallis test with Dunn-Bonferroni post-hoc testing was used. For all statistical tests, values of p < 0.05 were considered significant.
Results
Demographics
Among the 4567 patients included, 90 had RA (2.0%). Demographic data in each group are summarized in Table 1. Compared to non-RA patients, RA patients in our cohort were more likely to be female (80.0% vs. 41.7%, p < 0.001), with lower BMI (23.2 kg/m2 vs. 24.4 kg/m2, p = 0.002), higher ASA classification (p = 0.01) and lower current smoking rate (2.2% vs. 10.6%, p = 0.01). Among patients who successfully completed preoperative PRO questionnaires, NRS for leg pain (7.3 vs. 6.6, p = 0.03), PCS (19.0 vs. 26.1, p < 0.001), EQ-5D (0.514 vs. 0.558, p = 0.01), and ODI (51.1 vs. 42.1, p < 0.001) were all worse in RA patients.
No significant differences were seen in the number of spinal levels involved, but fusion surgery was more common in the RA group (48.9% vs. 33.8%, p = 0.003). Operation time was longer (162 min vs. 140 min, p = 0.01) and estimated blood loss was greater (254 vs. 154 mL, p < 0.001) in the RA group.
A total of 2394 patients (52.4%) completed 1-year postoperative PRO questionnaires, enabling further analysis. Table 2 shows the results for PRO scores with intergroup comparisons. All PRO scores investigated in the present study showed significant postoperative improvement compared to preoperative scores (p < 0.001) for the entire cohort. Comparisons between RA and non-RA patients revealed that postoperative NRS for leg pain, PCS, EQ-5D, and ODI were significantly worse in RA patients. Thirty-day complication rates were higher in the RA group (11.1%) than in the non-RA group (4.5%, p = 0.003), with urinary tract infection as the most frequent complication among RA patients (3.3%).
Propensity score matching
Propensity score matching generated 61 pairs of RA and non-RA patients who underwent posterior lumbar surgery. As expected, no differences were evident between groups for any of the factors included in propensity score calculation, and the two groups showed statistically identical baseline characteristics (Table 3). Fusion surgery represented approximately half of surgeries in both groups (49% vs. 46%, p = 0.72).
In this matched cohort, a total of 40 pairs (65.6%) completed 1-year postoperative PRO questionnaires, enabling further analyses. Although similar interventions were performed for the two groups of patients with similar backgrounds, RA patients still reported worse postoperative PCS (28.4 vs. 37.2, p = 0.008) and EQ-5D (0.640 vs. 0.738, p = 0.03) than non-RA patients (Table 4), although 30-day complications rates did not differ significantly between RA and non-RA groups (11.5% vs. 3.3%, p = 0.08).
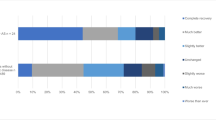
Impact of steroid usage on postoperative outcomes (post-hoc analysis)
Approximately half of the RA group (18 out of 40 patients) were steroid users, while only one patient in the non-RA group was using steroids (p < 0.001). Among RA patients on steroid, the dosage ranged from 0 to 10 prednisolone mg equivalents per day with a mean 2.2 mg/day. MTX usage and biologic usage were not different between RA patients with and without steroid (MTX: 50% vs. 50%, p > 0.99, biologics: 28% vs. 14%, p = 0.43), but preoperative serum CRP were significantly higher in RA patients on steroid (mean 0.80 vs. 0.51 mg/dL, p = 0.03). To clarify the impact of steroid usage on postoperative outcomes, further analysis was conducted to compare outcomes among non-steroid users without RA (n = 39), non-steroid users with RA (n = 22), and steroid users with RA (n = 18). Kruskal–Wallis testing revealed significant differences among the three groups for PCS (p = 0.003), EQ-5D (p = 0.007), and ODI (p = 0.02), despite a lack of significant differences in back or leg pain (p = 0.15 and 0.25). Comparisons of PRO scores are summarized in Fig. 1. According to post-hoc analyses, steroid-dependent RA patients showed significantly inferior results to non-RA patients in PCS (mean: 23.0 vs. 37.3, p = 0.002), EQ-5D (0.580 vs. 0.737, p = 0.006), and ODI (37.5 vs. 24.2, p = 0.02), whereas steroid-independent RA patients showed comparable results to non-RA patients. Among the steroid-dependent RA patients, those with daily steroid dosage equivalent to 5 mg of prednisolone or more tended to show the lowest quality of life scores with mean PCS of 18.5, mean EQ-5D of 0.582 and mean ODI of 39.7. 30-day complications rates did not differ significantly among the three groups (17% in steroid-dependent RA patients, 18% in steroid-independent RA patients, 3% in non-RA patients, p = 0.09).
Discussion
The present study used propensity score-matched analyses to elucidate the differences in outcomes following lumbar spinal surgery between RA and non-RA patients. This controlled comparative study minimized the risk of biases in terms of patient demographics, allowing us to elucidate the true impact of RA as a diagnosis on postoperative outcomes following lumbar surgery. Our results revealed that RA patients showed worse SF-12 PCS and EQ-5D than the non-RA matched cohort, indicating that RA negatively affected postoperative outcomes. However, steroid-independent RA patients showed comparable outcomes to non-RA patients.
Very few previous studies have reported on the relative equivalence of postoperative outcomes for RA and non-RA patients. Crawford et al. first reported that clinical outcomes after posterolateral lumbar fusion as graded using the Herkowitz and Kurtz scale [21] (excellent, good, fair, and poor) were similar between 19 RA patients and 19 age-, sex-, smoking status-, and spinal level-matched non-RA patients, although RA patients displayed a slightly higher complication rate due to osteopenia and immunosuppression [11]. Gulati et al. showed more detailed outcome measures, including ODI, EQ-5D, NRS for back pain, and NRS for leg pain at 1 year after lumbar decompression surgery, finding no differences between 37 RA patients and 1396 non-RA patients, although the two cohorts were not matched and background characteristics differed [14]. Gulati et al. denied any increased risk of complications in the RA group. In contrast, Kang et al. more recently argued that 40 RA patients displayed lower ODI scores at 1 and 2 years after posterolateral lumbar fusion, compared to a total of 134 age-, sex-, bone mineral density-, smoking-, diabetes-, and spinal level-matched non-RA patients [16]. In summary, the conclusions drawn from previous studies have been inconsistent, with some including non-matched cohorts or patients treated using outdated surgical strategies.
Kang et al. speculated in their report showing poorer improvement in RA than in non-RA patients that multiple joint involvement in RA lead to increased overall disability [16]. It is true that quality of life in RA patients is inherently impaired due to the destruction of multiple joints along with the associated chronic pain [22]. Postoperative health conditions are thus inevitably affected in a negative manner compared to non-RA patients, and fair comparison between the two groups has remained a huge challenge. The novelty of the present study lies in the meticulous propensity score-matching process incorporating preoperative PRO measurements. Through the statistical adjustment of background factors between RA and non-RA patients, this baseline impairment was already accounted for before the comparisons. The present study achieved inclusion of the largest number of matched pairs with the most statistically robust matching method in the literature. In the present propensity-score matched analysis, our results supported the findings of Kang et al., [16] suggesting unfavorable postoperative outcomes in RA patients even after adjustment for background. Interestingly, however, these differences were missing in comparisons among non-steroid users. These results implicated that poorer outcomes in RA patients were mainly due to steroid-related complications. These quite encouraging findings for both RA patients and spinal surgeons can be explained by two major hypotheses. First, the side effects of steroid treatment appear closely related to possible complications that could occur after lumbar spinal surgery and thereby negatively affect patient outcomes. Immunosuppression can lead to a higher chance of surgical site infection as well as other types of infectious complication, such as urinary tract infection and aspiration pneumonia [23]. Osteopenia and osteoporosis can result in vertebral fractures in adjacent segments and instrument failure due to screw loosening [12]. Steroid usage has been part of the classic presentation of RA patients and places significant burdens on surgical outcomes in general. Mitsuyama et al. also classically reported the pitfalls in surgical management of lumbar spinal canal stenosis in RA patients lie in the higher risk of infection, instrumentation failure and vertebral fracture showing the post-operative results of their 11 out of 12 patients being on steroid [24]. Second, as treatment options have markedly increased with the introduction of biologics, steroid usage might be interpreted as a surrogate marker of suboptimal RA control [25]. This may not be the case for all RA patients on steroids, but steroid-independent RA patients as a group might have achieved better disease control, and thus show a lower likelihood of ongoing joint destruction and instability.
Several limitations to the present study must be kept in mind when interpreting these findings. First, the database used in the analysis was obtained retrospectively and some pertinent information related to treatments received by patients was not obtainable. For instance, serological and/or physical proofs of RA control, including serum erythrocyte sedimentation rate and Disease Activity Score in 28 joints, were also not investigated. Therefore, even though RA patients did show inferior postoperative outcomes, the explanations for these findings remain speculative, while RA patients on steroid, who were particularly associated with poor outcomes, showed higher serum CRP indicating suboptimal control of systemic inflammation. In particular, the effects of RA control or treatment options on postoperative outcomes need to be validated in future studies. A second limitation was the percentage of patients who provided completed questionnaires at 1 year postoperatively. Although loss to follow-up is an unavoidable problem in surveillance-based multicenter studies, potentially leading to selection bias, outcomes in non-responders may not be inferior to those of responders [26]. Lastly, the present study focused on mid-term postoperative results and long-term outcomes with more than 2 years of follow-up are yet to be elucidated. A follow-up period of 1 year has been considered appropriate to analyze postoperative results following decompression, as Gulati et al. reported with a similar study design [14], but instrumentation-related long-term complications such pseudarthrosis and adjacent segment disease ideally need to be investigated for 2 years [16]. Further studies are warranted to elucidate whether RA or its control affect postoperative outcomes over the long term.
Conclusions
In conclusion, a diagnosis of RA was associated with worse postoperative outcomes after posterior surgery for degenerative lumbar disease compared with propensity score-matched non-RA patients. However, steroid-independent RA cases showed comparable outcomes to steroid-independent non-RA patients. Contemporary well-controlled RA patients warrant a reconsideration of risk assessment for spinal surgery, as the previous impression of a high-risk profile may no longer be entirely appropriate.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- RA:
-
Rheumatoid arthritis
- BMI:
-
Body mass index
- ASA:
-
American Society of Anesthesiologists
- PRO:
-
Preoperative patient-reported outcome
- NRS:
-
Numerical rating scale
- SF-12:
-
Short Form-12
- PCS:
-
Physical component summary
- EQ-5D:
-
EuroQOL 5-dimension
- ODI:
-
Oswestry Disability Index
- TNF-α:
-
Tissue Necrosis Factor alpha
- JAK:
-
Janus Kinase
References
Scott DL, Wolfe F, Huizinga TW. Rheumatoid arthritis. Lancet. 2010;376:1094–108.
Boden SD, Dodge LD, Bohlman HH, Rechtine GR. Rheumatoid arthritis of the cervical spine. a long-term analysis with predictors of paralysis and recovery. J Bone Joint Surg Am. 1993;75:1282–97.
Nam JL, Ramiro S, Gaujoux-Viala C, Takase K, Leon-Garcia M, Emery P, Gossec L, Landewe R, Smolen JS, Buch MH. Efficacy of biological disease-modifying antirheumatic drugs: a systematic literature review informing the 2013 update of the EULAR recommendations for the management of rheumatoid arthritis. Ann Rheum Dis. 2014;73:516–28.
Kaito T, Hosono N, Ohshima S, Ohwaki H, Takenaka S, Fujiwara H, Makino T, Yonenobu K. Effect of biological agents on cervical spine lesions in rheumatoid arthritis. Spine (Phila Pa 1976). 2012;37:1742–6.
Lawrence JS, Sharp J, Ball J, Bier F. Rheumatoid arthritis of the lumbar spine. Ann Rheum Dis. 1964;23:205–17.
Sims-Williams H, Jayson MI, Baddeley H. Rheumatoid involvement of the lumbar spine. Ann Rheum Dis. 1977;36:524–31.
Joo P, Ge L, Mesfin A. Surgical Management of the Lumbar Spine in Rheumatoid Arthritis. Global Spine J. 2020;10:767–74.
Hagege B, Tubach F, Alfaiate T, Forien M, Dieude P, Ottaviani S. Increased rate of lumbar spondylolisthesis in rheumatoid arthritis: a case-control study. Eur J Clin Invest. 2018;48:e12991.
Sugimura Y, Miyakoshi N, Miyamoto S, Kasukawa Y, Hongo M, Shimada Y. Prevalence of and factors associated with lumbar spondylolisthesis in patients with rheumatoid arthritis. Mod Rheumatol. 2016;26:342–6.
Kothe R, Kohlmann T, Klink T, Ruther W, Klinger R. Impact of low back pain on functional limitations, depressed mood and quality of life in patients with rheumatoid arthritis. Pain. 2007;127:103–8.
Crawford CH 3rd, Carreon LY, Djurasovic M, Glassman SD. Lumbar fusion outcomes in patients with rheumatoid arthritis. Eur Spine J. 2008;17:822–5.
Park JS, Shim KD, Song YS, Park YS. Risk factor analysis of adjacent segment disease requiring surgery after short lumbar fusion: the influence of rheumatoid arthritis. Spine J. 2018;18:1578–83.
Seki S, Hirano N, Matsushita I, Kawaguchi Y, Nakano M, Yasuda T, Motomura H, Suzuki K, Yahara Y, Watanabe K, Makino H, Kimura T. Lumbar spine surgery in patients with rheumatoid arthritis (RA): what affects the outcomes? Spine J. 2018;18:99–106.
Gulati A, Solberg T, Giannadakis C, Hoff M, Haugeberg G, Nygaard O, Gulati S. Surgery for lumbar spinal stenosis in patients with rheumatoid arthritis: a multicenter observational study. Eur J Rheumatol. 2016;3:56–60.
Mesfin A, El Dafrawy MH, Jain A, Hassanzadeh H, Kostuik JP, Lemma MA, Kebaish KM. Surgical outcomes of long spinal fusions for scoliosis in adult patients with rheumatoid arthritis. J Neurosurg Spine. 2015;22:367–73.
Kang CN, Kim CW, Moon JK. The outcomes of instrumented posterolateral lumbar fusion in patients with rheumatoid arthritis. Bone Joint J. 2016;98-B:102–8.
Cheak-Zamora NC, Wyrwich KW, McBride TD. Reliability and validity of the SF-12v2 in the medical expenditure panel survey. Qual Life Res. 2009;18:727–35.
EuroQol Group. EuroQol–a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208.
Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy. 1980;66:271–3.
Rosenbaum PR, Rubin DB. The central role of the propensity score in observational studies for causal effects. Biometrika. 1983;70:41–55.
Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. a prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am. 1991;73:802–8.
Haridoss M, Bagepally BS, Natarajan M. Health-related quality of life in rheumatoid arthritis: Systematic review and meta-analysis of EuroQoL (EQ-5D) utility scores from Asia. Int J Rheum Dis. 2021;24:314–26.
Bernstein DN, Kurucan E, Menga EN, Molinari RW, Rubery PT, Mesfin A. Comparison of adult spinal deformity patients with and without rheumatoid arthritis undergoing primary non-cervical spinal fusion surgery: a nationwide analysis of 52,818 patients. Spine J. 2018;18:1861–6.
Mitsuyama T, Kubota M, Yuzurihara M, Mizuno M, Hashimoto R, Ando R, Okada Y. The pitfalls in surgical management of lumbar canal stenosis associated with rheumatoid arthritis. Neurol Med Chir (Tokyo). 2013;53:853–60.
Black RJ, Lester S, Buchbinder R, Barrett C, Lassere M, March L, Whittle S, Hill CL. Factors associated with oral glucocorticoid use in patients with rheumatoid arthritis: a drug use study from a prospective national biologics registry. Arthritis Res Ther. 2017;19:253.
Solberg TK, Sorlie A, Sjaavik K, Nygaard OP, Ingebrigtsen T. Would loss to follow-up bias the outcome evaluation of patients operated for degenerative disorders of the lumbar spine? Acta Orthop. 2011;82:56–63.
Acknowledgements
The authors thank all members of the University of Tokyo Spine Group for supporting this work.
University of Tokyo Spine Group
Yasushi Oshima1, Naohiro Kawamura,2 Akiro Higashikawa,3 Nobuhiro Hara,7 Takashi Ono,6 Yujiro Takeshita,4 Yuki Taniguchi,1 Yoshitaka Matsubayashi,1 So Kato1
1Department of Orthopaedic Surgery, the University of Tokyo, 7–3-1 Hongo, Bunkyo-ku, Tokyo, 113–8655, Japan, 2Department of Spine and Orthopedic Surgery, Japanese Red Cross Medical Center, 4–1-22 Hiroo, Shibuya-ku, Tokyo, 150–8935, Japan, 3Department of Orthopedic Surgery, Japan Organization of Occupational Health and Safety Kanto Rosai Hospital, Kizukisumiyoshi-cho, Nakahara-ku, Kawasaki, 211–8510, Japan, 4Department of Orthopedic Surgery, Japan Organization of Occupational Health and Safety Yokohama Rosai Hospital, 3211 Kozukue-Chō, Kōhoku-Ku, Yokohama, 222–0036, Japan, 6Department of Spinal Surgery, Japan Community Health-Care Organization Tokyo Shinjuku Medical Center, 5–1 Tsukudo-cho, Shinjuku-ku, Tokyo, 162–8543, Japan, 7Department of Orthopedic Surgery, Japanese Red Cross Musashino Hospital, 1–26-1 Kyonancho, Musashino, Tokyo, 180–8610, Japan.
Funding
No funds were received in support of this work.
Author information
Authors and Affiliations
Consortia
Contributions
SK, HN, designed the research, analyzed data, and wrote the manuscript. YM, YT, TD, ST, YO designed the research and supervised the study. YY, AH, YT, MF, TO, NH, RO, HI, MO, SS, SH, KM designed the research and acquired the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent was obtained from all participants and approval for this study was given by the institutional review board of the Clinical Research Support Center at the University of Tokyo. All procedures performed in the studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki Declaration and its later amendments or comparable ethical standards.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visithttp://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kato, S., Nakamoto, H., Matsubayashi, Y. et al. Postoperative outcomes after degenerative lumbar spine surgery in rheumatoid arthritis patients -a propensity score-matched analysis. BMC Musculoskelet Disord 23, 380 (2022). https://doi.org/10.1186/s12891-022-05326-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12891-022-05326-5