Abstract
Background
HIV immunosuppression increases susceptibility to other STIs and STIs can enhance HIV transmission, reduce CD4 cell count and increase viral load. Co-infections of HIV and STIs may thus reduce the preventive benefits of ART. Little is known about the incidence rate of STIs among long-term patients on ART.
Method
We conducted a secondary data analysis of all patients enrolled in a rural and an urban longitudinal cohort studies who initiated ART between April 2003 and July 2007 followed up to 2016. Patients were screened for STI every three months using “a syndromic and case management approaches”. STI incidence rate, was defined as the number of new cases per population at risk over the follow-up review period. We performed a time-to-event and Kaplan Meier analysis. We used a multivariable Cox proportional hazards regression model to assess for factors associated with STI incidence.
Result
Of 1012 participants, 402 (39.8%) were urban and 610 (60.2%) rural residents. Mean age was 42.8 years (SD 8.5). The total number of follow up time was 44,304 person years. We observed STI incidence rate of 2.1 per 1000 person-years after follow-up. Rural residence (adjusted hazard ratio [aHR] 3.53, 95% CI: 1.95–6.39), younger age (aHR 2.05, 95% CI: 1.02–4.12 for 18–34 years and aHR 1.65, 95% CI: 1.00–2.72 for 35–44 years) were factors associated with higher incidence of STIs. Being male (aHR 0.51, 95% CI: 0.27–0.93) was associated with a lower incidence of STIs.
Conclusion
We found STIs incidence rate of approximately 3 per 1000 person-years among patients on long-term (≥ 4 years) ART followed up-to 3.5 years. Rural and younger persons on ART should be routinely screened for STIs because high incidence of STIs may undo the preventative effects of ART for all.
Similar content being viewed by others
Background
HIV-related immunosuppression increases susceptibility to other sexually transmitted Infections (STIs) [1, 2]. Co-infection with STIs facilitates HIV acquisition and transmission by disrupting the integrity of genital mucosa, generating inflammatory responses which recruits HIV target cells, inducing cytokine responses which regulate HIV replication and increase HIV shedding [3, 5, 6, 27, 28]. Genital ulcers in women increases male to female HIV transmission 10 to 50-fold [4]. Although, this data is for people living with HIV not on ART, incident STIs in people on ART may thus reduce the preventive benefits of ART [1]. STI incidence can also serve as a marker of risky sexual behavior [7, 8, 14].
STIs are caused by viral, bacterial, protozoa, fungal and parasitic agents and present as abnormal vaginal or urethral discharges and ulcerative or non-ulcerative genital lesions. Because laboratory diagnosis is complex, expensive, and results in a delayed initiation of treatment, WHO recommended a syndromic and case management approach for developing countries [15, 16]. The Uganda Ministry of Health also recommends a syndromic and case management approaches to STIs among people infected with HIV in public health care facilities. STI related history taking, a physical examination, and clinical algorithms are used to diagnose and management the commonest biological causes of STIs. Where possible, syphilis serologic screening is performed [16,17,18].
A limited number of studies have evaluated the incidence of STIs among people on ART in sub-Saharan Africa. A South African study found a 14% six-month incidence of STIs measured as treatment seeking for a new STI after initiating ART and observed that individuals diagnosed with an incident STI using a syndromic approach were more likely to have a detectable viral load [12]. Another South African study observed a seven-fold higher rate of STIs after starting ART compared to before ART [9]. In Uganda, a study using STIs syndromic screening algorithms with high cervical swabs for women eligible for intra-uterine contraception where DNA was extracted from the swabs and PCR assay done to detect Neisseria gonorrhea, Trichomonas vaginalis and Chlamydia trachomatis infections found STIs incidence of 11.1% (95% CI: 7.8–14.4) among women on ART [10]. In China, among the 4510 market vendors evaluated for STIs using a syndromic approach by the physician, compared with laboratory tests as a gold standard found a sensitivity of 36.7% among participants reporting STI symptoms and 5.1% among those without an STI symptom [31]. In India, among patients who attended an STI clinic found a sensitivity of genital discharge syndrome for Neisseria gonorrhea at 96% and Chlamydia at 91% while the specificity was low (76 and 72%, respectively). The sensitivity of genital ulcers syndrome for herpes simplex virus-2 and Treponema palladium was 83 and 81% respectively while its specificity was at 99% [32].
While there is some information on STI in the first year(s) of ART, there is a dearth of information on STI incidence in patients on long-term ART in resource-limited settings. Using a syndromic and case management approach, we evaluated the STI incidence rate and assessed factors associated with STIs incidence in patients on long-term ART in an urban and a rural cohort in Uganda.
Methods
Study design
We performed a secondary analysis of data from two longitudinal cohorts of individuals on long-term ART: the ART cohort of The Infectious Diseases Institute (IDI) of the College of Health Sciences at Makerere University in Kampala, Uganda [24] and the ART cohort of The AIDS Support Organization (TASO) in Jinja, Uganda [26].
Study setting
The IDI urban ART cohort in Kampala
The adult IDI clinic is a center of excellence for HIV care and treatment [23] located in Mulago Teaching Hospital in Kampala-Uganda. The out-patient clinic has over 30,000 patients ever enrolled and cares for people living in five Kampala municipalities. ART is provided free of charge, initially though the Global Fund and later mainly through the US President’s Emergency Plan for AIDS Relief (PEPFAR).
Following written informed consent, adults (age ≥ 18 years) starting ART between April 2004 and April 2005 were enrolled in a cohort study and followed up for 10 years (hereafter referred to as the urban cohort). ART was started in patients with WHO Stage 4 or CD4 count ≤200 cells/ml, (according to national treatment guidelines implemented at that time), and consisted of stavudine (weight-adjusted, but discontinued in 2013 in Uganda), lamivudine and nevirapine (fixed-dose combination) or zidovudine, lamivudine (fixed-dose combination) and efavirenz. A doctor or clinician and adherence counselor evaluated cohort participants at study enrolment and every three months thereafter while they attended the clinic for ART medication refills [24]. At each study visit, a physical examination was performed and information was recorded about HIV status of the partner(s), social support, sexual history in the past month including STIs screening, diagnosis and treatment. At each clinic visit, the study Doctor asked if the participant experienced any of the syndromic symptoms read to the participant since the last visit, a syphilis serology was done for selected participants based on presenting symptoms. ART was monitored every 6 months through viral load (VL) testing. Participants with a VL ≥1000 copies/ml were offered enhanced adherence counseling and support. Patients with two consecutive viral loads ≥1000 copies/ml were eligible for second-line ART.
The TASO rural ART cohort in Jinja
TASO was the first and is one of the largest non-governmental organizations in sub-Saharan Africa (SSA), providing treatment to over 98,000 patients through 11 TASO care facilities in Uganda. Since 2004, TASO Jinja facility has cared for people living with HIV in Jinja district within a radius of 75 km and currently provides ART to over 5000 people. In 2015, A world bank report on development indicators categorized 83.9% of Jinja population as rural. In this study, 81% of the study participants resided outside Jinja municipality.
In June 2012, TASO Jinja initiated a prospective longitudinal cohort study (the Long-Term Outcomes on ART in Uganda Study) of adults who had been receiving first-line ART for a minimum of 4 years (hereafter referred to as the rural cohort) [20, 21]. Between July 1, 2012, and December 31, 2013, all individuals receiving first-line ART for at least 4 years were eligible to participate in the cohort study. From August 2014 until January 2015, enrollment was restricted to patients on ART for at least 4 years with CD4 cell count ≤450 cells/mm3 in order to over-sample participants who may have had virologic failure. All participants continued to receive routine comprehensive HIV care from TASO service providers. All participants received a VL test at enrollment. Participants with a VL ≥1000 copies/ml were offered enhanced adherence counseling and VL was re-assessed after three months.
Patients were followed up for an additional 3–3.5 years. Every six months, cohort participants completed an interviewer-administered standardized questionnaire (adapted from the HAARP study) [25] to collect behavioral and treatment outcomes. Clinical care was provided by doctors and clinicians and included STI syndromic screening and management. At each clinic visit the study nurse asked if the participant experienced lower abdominal pain with abnormal vaginal discharge, sores or pus in the penis and vagina since the last visit. and a syphilis serology done for selected participants based on symptoms. Laboratory monitoring included CD4 counts and VL every 6 months. CD4 counts were performed at the Jinja referral hospital regional laboratory. Plasma samples were stored in liquid nitrogen and shipped to the Medical Research Council/Uganda Virus Research Institute (MRC/UVRI) laboratory in Entebbe, Uganda for VL testing and resistance assays.
Data management and statistical analysis
The urban cohort data were directly collected into an electronic medical record by medical doctors who provided clinical care. Data were periodically validated by a senior Data Manager as part of routine quality control checks. The rural cohort data were double entered using Epi-Info and imported into Microsoft Access for data management and storage. Laboratory test results were transmitted electronically from the MRC laboratory to the data center at TASO Jinja and manually entered into the study database.
For this analysis, data extracted from TASO and IDI database included socio-demographic information, ART start date, ART regimen, sexual behavior, ART adherence at enrolment and at subsequent clinic visits. Clinical data at enrollment and during follow up including information on STI syndromic symptoms and management, CD4 cell counts, and viral load testing were also extracted. Risky sexual behavior was defined as sexual intercourse with ≥2 partners or inconsistent or no condom use in previous 6 months.
In this analysis, baseline was defined as the time of enrollment into the cohort (rural cohort) or the 4-year visit on ART (urban cohort). We described baseline participant characteristics overall and by gender and cohort (urban and rural) using means and frequencies.
The primary outcome of interest was STI incidence rate, defined as the number of new diagnoses per study population at risk during the follow-up (up to additional 3.5 years for both cohorts taking time of enrollment into the cohort (rural cohort) or the 4-year visit on ART (urban cohort) as the baseline. The primary endpoint (STI diagnosis) was defined as syndromic diagnosis (urethral discharge, genital ulcer disease, abnormal vaginal discharge) and a laboratory diagnosis of syphilis. We focused on first STI during follow, only 0.9% of study participants had more than one STI diagnosed during follow up. In time-to-event analysis, all participants contributed person-time from baseline until occurrence of event (STI diagnosis), death, lost to follow up, and transferred out, withdrawal of consent or completion of 3.5 years of follow up, whichever occurred first. A Kaplan-Meier analysis was performed to estimate time to first STI. Using a Cox proportional hazards regression model, we evaluated for associations between STIs and covariates (urban/rural residence, age, CD4 cell count, viral load, gender, education level, marital status, occupation, and time on ART). Covariates were included in the initial Cox model based on prior knowledge and results of the bivariable association and removed using a backward elimination procedure to identify factors independently associated with STI incidence.
Results
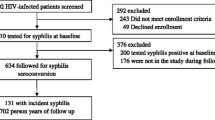
Overall, 1012 individuals on ART for 4 years or longer were included in the analysis. Of these, 402 (39.8%) were from the urban cohort and 610 (60.2%) from the rural cohort. Most patients were female (69.6% urban vs 75.7% rural cohort) and about half (53.3% urban vs 54.4% rural) were not married. At baseline, mean age was 42.8 years (SD 8.5). Slightly over a half (53.5%) of the urban but only 35.3% of the rural participants attained secondary education or higher. At baseline, the most common ART regimen was zidovudine, lamivudine, and nevirapine in the rural cohort and a tenofovir-based regimen in the urban cohort. At baseline, almost all participants (~ 90% in both cohorts) had a CD4 > 200 cells/mm3, but the mean CD4 count was lower in the urban compared to the rural cohort (mean CD4 cell count 426 vs 564 cells/mm3) Table 1. Cohort participants contributed a total follow up time of 32,806 person-years with a mean follow up duration of 51.3 months (SD 15.3). Almost all participants (352 or 87.1% of the urban cohort and 589 or 96.6% rural cohort participants) completed 3.5 years of follow up. Sixteen (3.9%) urban and 4 (1.0%) rural cohort participants were lost to follow up or transferred out; Twenty-one (5.2%) urban participants and 17 (2.9%) rural participants were reported dead and 15 urban participants withdrew study consent during follow up. (Fig. 1).
During follow up, 94 participants were diagnosed with STIs (39 Vaginal discharge syndrome, 29 genital ulcer disease, 13 urethral discharge syndrome and 13 with Syphilis). Of the 94 diagnosed, 84/1012 (8.3%) had at least one STI recorded in the cohort participants and 10/1012 (0.99%) cohort participants had more than one STI, corresponding to an STI incidence rate of 2.8 per 1000-person-years (95% C1:2.3–3.4). Incidence rate was observed among those practicing risky sexual behavior (4.31 vs 2.51 per 1000 person-years), females (3.25 vs 1.47 per 1000 person-years) and rural cohort participants (3.6 vs 1.38 per 1000 person-years). Table 2.
In the Kaplan-Meier failure analysis for cumulative probability of having sexually transmitted infections, we observed a significant difference and higher STI incidence over 3.5 years of follow-up in the rural participants compared to the urban participants (log rank test P < 0.001). (Fig. 2) In the bivariate Cox model, rural residence (hazard ratio [HR] 2.58, 95% CI: 1.52–4.40), risky sexual behavior (HR 1.70, 95% CI: 1.04–2.77), and younger age (HR 2.13, 95% CI: 1.08–4.21 for 18–34 years and HR 1.73, 95% CI: 1.07–2.83 for 35–44 years as compared to > 44 years) were associated with higher incidence of STIs. Being male (HR 0.45, 95% CI. 0.25–0.81) was associated with a lower incidence of STIs. Rural residence (adjusted HR [aHR] 2.82, 95% CI: 1.60–5.00); and younger age (HR 2.13, 95% CI: 1.08–4.21 for 18–34 years and HR 1.73, 95% CI: 1.07–2.83 for 35–44 years as compared to > 44 years) remained associated with higher incidence of STIs in multivariate analysis. Being male (aHR 0.51, 95% CI. 0.28–0.92) remained associated with a lower incidence of STIs (Table 3).
Discussion
In this cohort study of patients on long-term (≥ 4 years) ART, we found an STI incidence rate of 2.8 per 1000 person-years. The lower incidence rate observed in our study could be because we assessed STIs among patients who were already experienced on ART, thus, they received STIs prevention messages during ART initiation and subsequent clinic follow-up. Rural residence, female gender, and younger age were independently associated with a higher STI incidence.
Data on the incidence of STIs in people on ART in sub-Saharan Africa are scarce. In South Africa, one study also found a low incidence rate of STI of 1.29 per 1000 person-years (95% CI 1.24–1.34) in a cohort of 1465 patients followed for 3 years after initiating ART [12] using syndromic diagnoses of STIs. In the South African study, the rate of treatment seeking for new STIs was seven-fold higher (aRR 7.01, 95% CI 4.64 to 10.59) while on ART compared to prior to initiating ART. Due to lack of published data on the STI incidence rate among people on long-term ART, we could not compare our data to other studies in sub-Saharan Africa.
Our findings that rural residence was associated with higher incidence of STIs was also observed in a nationally representative Uganda survey that assessed STI as self-reported STIs and/or associated symptoms in the past 12 months of the general population aged 18–49 [19]. The lower STIs rates observed among the urban participants could be because they continuously received condom promotion messaging and counseling as evidenced by lower condom use (69.5%,146/210) in the rural participants compared to (30.5%, 64/210) in the urban participants at baseline visit) and urban population had greater exposure to HIV prevention messaging.
In the survey of the general Ugandan adult population, having multiple sexual partners was found to be a significant risk factor for STI [9]. In our cohort, participants reporting risky sexual behavior were 50% more likely to have an STI (aHR 1.51), but the association was not statistically significant (95% CI: 0.91, 2.51). Risky sexual behavior has been shown to persist among people on long-term ART [11,12,13,14, 29] and may thus place people on long-term ART at continued risk for STIs and HIV transmission to sexual partners.
The association between female gender and younger age and a high incidence of STIs is consistent with other studies in Uganda and South Africa [11, 19,20,21,22]. In a South African cohort study of 1465 patients followed for 3 years after initiating ART, being female and younger were associated with higher incidence of clinic visits for STI treatment [12]. Our findings are not surprising as younger people are a sexually active group, tend to have multiple sexual partners, and their knowledge and awareness of safer sexual behavior and practices may be lower compared to older adults. Additionally, females tend to have a better health-seeking behavior in issues relating to STIs than men and many vaginal discharge may not be an STI [30].
Our study had several strengths, including its prospective data collection design, the inclusion of a cohort in both a rural and an urban setting, and a relatively large sample size with long follow up. An important limitation of our study is that biological samples were not collected to confirm an STI diagnosis. As per Uganda Ministry of Health guidelines (adapted from WHO STI’s guidelines), and similar to the situation in most developing countries, majority of the STI diagnoses were made through a “syndromic and case management approach” [16, 21]. The failure of the syndromic approach to detect STI among asymptomatic patients [31] was a limitation to the study. Another limitation is that some participants may have received an STI diagnosis and treatment in a primary care clinic in between the three monthly visits at the HIV care and treatment center. This could have resulted in an underestimation of the STI incidence.
Conclusion
In this cohort study of patients on long-term (≥ 4 years) ART, we found STIs incidence rate of approximately 3 per 1000 person-years after 3.5 years of follow-up. Rural and younger persons on ART should be prioritized for routine STIs testing in HIV care clinics to enable early diagnosis and management because if diagnosed late and poorly managed lead to serious complications of their own. Furthermore, they enhance sexual transmission of HIV, therefore, making timely and proper STI diagnosis is of paramount importance.
Abbreviations
- ART:
-
Antiretroviral therapy
- IDI:
-
Infectious Diseases Institute
- MRC:
-
Medical Research Council
- TASO:
-
The AIDS Support Organization
- WHO:
-
World Health Organization
References
Johnson LF, Lewis DA. The effect of genital tract infections on HIV-1 shedding in the genital tract: a systematic review and meta-analysis. Sex Transm Dis. 2000;35(11):946–59. https://doi.org/10.1097/OLQ.0b013e3181812d15.
McClelland RS, Lavreys L, Katingima C, Overbaugh J, Chohan V, Mandaliya K, et al. Contribution of HIV-1 infection to acquisition of sexually transmitted disease: a 10-year prospective study. J Infect Dis. 2005;191(3):333–8.
Anderson BL, Wang C-C, Delong AK, Liu T, Kojic EM, Kurpewski J, et al. Genital tract leukocytes and shedding of genital HIV type 1 RNA. Clin Infect Dis. 2008;47(9):1216–21. https://doi.org/10.1086/592303.
Baeten JM. Antiretroviral pre-exposure prophylaxis for HIV-1 prevention among heterosexual African men and women: the partners PrEP study. Rome: In 6th IAS conference on HIV pathogenesis, treatment and prevention; 2011. p. 1–26.
Mayer KH, Venkatesh KK. Antiretroviral therapy as HIV prevention: status and prospects. Am J Public Health. 2010;100(10):1867–76. https://doi.org/10.2105/AJPH.2009.184796.
Shafer LA, Nsubuga RN, White R, Mayanja BN, Chapman R, O'Brien K, et al. Antiretroviral therapy and sexual behavior in Uganda: a cohort study. AIDS (London, England). 2011:671–8. https://doi.org/10.1097/QAD.0b013e328341fb18.
Msuya SE, Uriyo J, Hussain A, Mbizvo EM, Jeansson S, Sam NE, et al. Prevalence of sexually transmitted infections among pregnant women with known HIV status in northern Tanzania. Reprod Health. 2009;6(4). https://doi.org/10.1186/1742-4755-6-4.
Rogers WH. Regression standard errors in clustered samples. Stata Tech Bull. 1994;3(13):19–23. https://www.researchgate.net/publication/24137031_Regression_Standard_Errors_in_Clustered_Samples.
Naidoo S, Wand H, Abbai NS, Ramjee G. High prevalence and incidence of sexually transmitted infections among women living in Kwazulu-Natal, South Africa. AIDS Res Ther. 2014;11(1):31. https://doi.org/10.1186/1742-6405-11-31.
Kalichman SC, Eaton L, Cherry C. Sexually transmitted infections and infectiousness beliefs among people living with HIV/AIDS: implications for HIV treatment as prevention. HIV Med. 2010;11(8):502–9. https://doi.org/10.1111/j.1468-1293.2009.00818.x.
Kakaire O, Byamugisha JK, Tumwesigye NM. Gammell-Danielsson. Prevalence and factors associated with sexually transmitted infections among HIV positive women opting for intrauterine contraception. PLoS One. 2015;10(4). https://doi.org/10.1371/journal.pone.0122400.
Lurie MN, Kirwa K, Daniels J, Berteler M, Kalichman SC, Mathews C. High burden of STIs among HIV-infected adults prior to initiation of ART in South Africa: a retrospective cohort study. Sex Transm Infect. 2014;90(8):615–9. https://doi.org/10.1136/sextrans-2013-051446.
Kamali A, Kinsman J, Nalweyiso N, Mitchell K, Kanyesigye E, Kengeya-Kayondo JF, et al. A community randomized controlled trial to investigate the impact of improved STD management and behavioral interventions on HIV incidence in rural Masaka, Uganda: trial design, methods and baseline findings. Trop Med Int Heal. 2002;7(12):1053–63.
Kalichman SC, Pellowski J, Turner C. Prevalence of sexually transmitted co-infections in people living with HIV/AIDS: systematic review with implications for using HIV treatments for prevention. Sex Transm Infect. 2011;87(3):183–90. https://doi.org/10.1136/sti.2010.047514.
Bosu WK. The control of sexually transmitted diseases in Ghana: the real issues! Genitourin Med. 1997;73(228):229.
WHO. Management of Patients with Sexually Transmitted Diseases. Technical report series 810. Geneva: World Health Organization; 1991.
Adler MW. Sexually transmitted diseases control in developing countries. Genitourin Med. 1996;72:8388.
Hanson S, Sunkutu RM, Kamanga J, Hojer B, Sandstrom E. STD care in Zambia: an evaluation of the guidelines for case management through a syndromic approach. Int J STD AIDS. 1996;7:324332.
Darj E, Mirembe FM, Råssjö E-B. STI-prevalence and differences in social background and sexual behavior among urban and rural young women in Uganda. Sex Reprod Healthc. 2010;1:111–5.
Anguzu G, Flynn A, Musaazi J, Mujugira A, et al. Socio-economic Disparities and Sexually Transmitted Infections in Uganda. Kigali: Poster abstract INTEREST workshop; 29th-31st May 2018.
Sexually Transmitted Infections treatment guidelines for use by operational level workers in Uganda, 2003.
Marrazzo JM, Dombrowski JC, Mayer KH. Sexually transmitted infections in the era of antiretroviral-based HIV prevention: priorities for discovery research, implementation science, and community involvement. PLoS Med. 2018;15(1):e1002485. https://doi.org/10.1371/journal.pmed.1002485.
Nwaka S, Ochem A, Besson D, et al. Analysis of pan-African Centres of excellence in health innovation highlights opportunities and challenges for local innovation and financing in the continent. BMC Int Health Hum Rights. 2012;12(11). https://doi.org/10.1186/1472-698X-12-11. [published Online First: Epub Date].
Castelnuovo B, Kiragga A, Mubiru F, Kambugu A, Kamya M, Reynolds SJ. First-line antiretroviral therapy durability in a 10-year cohort of naïve adults started on treatment in Uganda. J Int AIDS Soc. 2016;19(1):20773. Published 2016 Jun 17. https://doi.org/10.7448/IAS.19.1.20773.
Birungi J, Min JE, Muldoon KA, Kaleebu P, King R, Khanakwa S, et al. Lack of effectiveness of antiretroviral therapy in preventing HIV infection in serodiscordant couples in Uganda: an observational study. PloS One. 2015;10(7):e0132182. https://doi.org/10.1371/journal.pone.0132182.
Okoboi S, Ding E, Persaud S, Wangisi J, Birungi J, Shergold S, et al. Community-based ART distribution system can effectively facilitate long-term program retention and low-rates of death and virologic failure in rural Uganda. AIDS Res Ther. 2015;12(1):37.
Wasserheit JN. Epidemiological synergy. Interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sex Transm Dis. 1992;19:61–77.
Mayer KH, Venkatesh KK. Interactions of HIV, other sexually transmitted diseases, and genital tract inflammation facilitating local pathogen transmission and acquisition. Am J Reprod Immunol. 2011;65:308–16.
Okoboi S, Castelnuovo B, Moore DM, Musaazi J, Kambugu A, Van Rie A, et al. Long-term risky sexual behavior among patients on antiretroviral therapy in urban and rural cohorts in Uganda: A longitudinal Prospective cohort study. Kigali: Poster abstract INTEREST workshop; 29th-31st May 2018.
Fomundam H. Identifying treatment and healthcare seeking behavior as a means of early HIV/AIDS intervention in Africa. World J AIDS. 2012;2(3):165–73.
Yin YP, Wu Z, Lin C, Guan J, Wen Y, Li L, Detels R, et al. Syndromic and laboratory diagnosis of sexually transmitted infection: a comparative study in China. Intl J STD AIDS. 2009;19(6):381–4.
Choudhry S, Ramachandran VG, Das S, Bhattacharya SN, Mogha NS. Pattern of sexually transmitted infections and performance of syndromic management against etiological diagnosis in patients attending the sexually transmitted infection clinic of a tertiary care hospital. Indian J Sex Transm Dis. 2010;31(2):104–8.
Acknowledgements
We would like to acknowledge The AIDS Support Organization (TASO) and Infectious Diseases Institute for allowing us to access study data as per their respective data access policy and Dr. Andrew Mujugira, Head of IDI Kasangati HIV prevention research centre of excellence for his on spot mentorship. DMM is supported by a Scholar Award from the Michael Smith Foundation for Health Research.
Funding
This sub-study was funded by the Canadian African Preventive Trial network Ph.D. scholarship awarded to SO as part of his Ph.D. program at the University of Antwerp, Belgium through Institute of Infectious Diseases and Molecular Medicine, University of Cape Town, South Africa. The Long-Term Outcomes Study was funded by the Canadian Institutes for Health Research (Grant number MOP-119369). The study funders had no role in the study design, data collection, analysis, interpretation of data and in writing the manuscript.
Availability of data and materials
The study data will be available upon request.
Author information
Authors and Affiliations
Contributions
D.M., B.J., S.O., B.C., and A.K, designed the study. S.O., M.J., B.T., MN, and B.C., supervised data collection of the study. SO, MJ and BT abstracted the data. SO, A.V.R., and M.J. conducted or contributed to the data analysis. S.O., B.C., MN, M.J., and A.V.R., Interpreted the data. S.O. prepared the original manuscripts, all authors contributed to subsequent revisions. All authors read and approved the final manuscript for submission.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The IDI urban cohort study was approved by the Makerere University School of Medicine IRB and the Uganda National Council for Science and Technology.
The Long-Term Outcomes on ART in Uganda was approved by the Research Ethics committee of TASO, the Science and Ethics Committee of the Uganda Virus Research Institute, the Uganda National Council for Science and Technology and the Research Ethics Board of the University of British Columbia. All participants provided written informed consent. Senior management of TASO and IDI approved data access as per their respective institutional data access and sharing policies.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Okoboi, S., Castelnuovo, B., Moore, D.M. et al. Incidence rate of sexually transmitted infections among HIV infected patients on long-term ART in an urban and a rural clinic in Uganda. BMC Public Health 19, 87 (2019). https://doi.org/10.1186/s12889-019-6417-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-019-6417-x