Abstract
Background
Previous studies have shown that pesticide bans were associated with reduced fatal pesticide self-poisoning cases in high, and low-and-middle-income countries. We aimed to investigate the characteristics of pesticide poisoning patients admitted to two Malaysian hospitals and the early impact of the national paraquat ban implemented on 1st January 2020 in a culturally heterogenous South-East-Asian upper-middle-income setting.
Methods
Data were collected from an East (Bintulu) and a West (Ipoh) Malaysian hospital medical records in 2015–2021 and 2018–2021, respectively. Logistic regression analyses were conducted to investigate the association of aspects such as socio-demographic and clinical characteristics, paraquat ban with the types of pesticides involved (paraquat versus non-paraquat versus unknown) ,and the outcomes (fatal versus non-fatal).
Results
From the study sample of 212 pesticide poisoning patients aged 15 years or above, the majority were self-poisoning cases (75.5%) with a disproportionate over-representation of Indian ethnic minority (44.8%). Most pesticide poisoning cases had socio-environmental stressors (62.30%). The commonest stressors were domestic interpersonal conflicts (61.36%). 42.15% of pesticide poisoning survivors had a psychiatric diagnosis. Paraquat poisoning accounted for 31.6% of all patients and 66.7% of fatalities. Case fatality was positively associated with male gender, current suicidal intent, and paraquat poisoning. After the paraquat ban, the proportion of pesticide poisoning cases using paraquat decreased from 35.8 to 24.0%, and the overall case-fatality dropped slightly from 21.2 to 17.3%.
Conclusions
Socio-environmental stressors in specific domestic interpersonal conflicts, seemed more prominent in pesticide poisoning compared to psychiatric diagnosis. Paraquat accounted for the majority of pesticide-associated deaths occurring in hospitals in the study areas. There was preliminary evidence that the 2020 paraquat ban led to a fall in case fatality from pesticide poisoning.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Background
More than 700,000 people die by suicide every year globally, with more than three-quarters of these deaths (79%) occurring in low- and middle-income countries (LMICs) [1]. Pesticide self-poisoning accounts for up to 1 in 5 suicides worldwide [1], with an estimated 110,000 to 168,000 deaths per year, with more than 95% of these deaths occurring in LMIC settings [1, 2].
The pesticides used in acts of self-poisoning are the products most readily available in the house, regardless of their toxicity [3, 4]. Thus, the type of pesticide available during a suicide crisis plays a crucial role in determining the outcome of pesticide poisoning, as pesticides with the same agricultural indication may have marked differences in toxicity/case fatality [5]. In keeping with this, regulating access to highly hazardous pesticides with a national ban was found to be the most effective means to reduce deaths by pesticide poisoning [6].
Paraquat is a highly hazardous herbicide with no known antidotes and it is associated with high case fatality following ingestion [7]. Numerous studies had shown that restricted use of such highly hazardous pesticides and substitution with less toxic pesticides can prevent deaths by suicide, without reducing crop yields [8,9,10].
Malaysia is an upper-middle-income country. Agriculture contributes to 7.4% of its GDP [11, 12]. Pesticide suicides are the second most common suicide method (13%) in Malaysia [13]. A systematic review [14] has estimated the national suicide rate as 6–8 per 100,000 population. Among pesticide poisoning, herbicides are the most commonly used pesticide with glyphosate and paraquat ranked as the first and second most common herbicides used in poisoning [15]. Malaysia has 14 states (12 in the west peninsular and 2 in the east peninsular) and 3 federal territories (2 in the west peninsular and 1 in the east peninsular). Perak state has highest pesticide poisoning burden in Malaysia based on the national poison centre database [15].
Sarawak also has a more significant pesticide poisoning burden in East Malaysia compared to the majority of West Malaysian states and federal territories [15]. Public hospitals under the Ministry of Health are the main referral centres for pesticide poisoning cases that present to healthcare services in Malaysia.
In 2002, a paraquat ban was announced in Malaysia with all uses to be phased out by June 2005. This move resulted in a slight drop in the incidence of paraquat poisoning [16]. However, due to challenges in identifying viable alternatives for the farming industry, this initial ban was rescinded in 2006 and replaced by regulations requiring the dilution of paraquat products in an attempt to reduce their toxicity [16]. Subsequently, there was a five-fold increase in the number of paraquat poisoning cases reported to the National Poison Centre and a total paraquat ban was re-implemented on the 1st January 2020. However, the use of the pre-existing stock of paraquat in the plantation sector appeared to be exempted from any legal penalty until 31st December 2020 [17].
Study aim
Our study aimed to [1] investigate the characteristics and trends in fatal and non-fatal pesticide poisoning, and [2] evaluate the effectiveness of a national paraquat ban in reducing fatal pesticide poisoning in a dual-centred Malaysian hospital-based sample in two agricultural states of Perak and Sarawak.
Methods
Study design and setting
We conducted a retrospective medical record-based study of pesticide poisoning patients presenting to the Bintulu Hospital (HB) in Sarawak State, East Malaysia (from 1st January 2015 to 31st December 2021), and the Raja Permaisuri Bainun Hospital (HRPB), Ipoh, in Perak State, West Malaysia (from 1st January 2018 to 31st December 2021). HB is a major tertiary hospital serving the Bintulu division and provides specialist support to Mukah and northern Kapit divisions in Sarawak state. The estimated population size in these regions was 441,400 people in 2020. HB had a total of 302 beds during the study period. HRPB is the state specialist hospital which provides tertiary services within the state of Perak, mainly for the catchment area of the Kinta district (population = 888,767). HRPB had a total of 990 beds during the study period. HB and HRPB are both public hospitals governed by the Ministry of Health in which both hospitals serve a specific catchment area of the respective local populations. To date, there have been no changes in the hospital catchment areas within-and inter-state, and before and after the national paraquat ban. The World Health Organization’s case definition matrix for acute pesticide poisoning was employed to identify pesticide poisoning patients [18]. In HB, cases were searched in the electronic health records system and identified using the International Classification of Diseases, Tenth Revision (ICD-10) code T60 (pesticide poisoning). In HRPB, the ICD-10 coding system was not fully implemented, and thus cases were identified by searching in the electronic clinical documentation system maintained by the medical records office. Search terms used include pesticide, self-harm, paraquat, suicide, and overdose. Patients were excluded if there was no documented evidence of pesticide exposure, no documented signs and symptoms commonly found in pesticide poisoning. Signs and symptoms include but not limited to nausea, vomiting, abdominal pain, diarrhoea,miosis, seizures, and bradycardia or respiratory difficulties [19, 20]. Patients were also excluded if there is no evidence of a clear relationship between the documented pesticide exposure and the patients’ presenting signs and symptoms. Data of patients hospitalized for pesticide poisoning were available in documented case records done by the medical and psychiatry units after admission. Forensic data for brought-in-dead cases in HB and the state forensic death registries in the catchment areas of HRPB were reviewed to ensure the identification of all fatal pesticide poisoning cases, including cases of pesticide poisoning deaths that were not sent to either hospital.
Characteristics and description of study materials
Data were collected from the medical records for the following patient characteristics: socio-demographic characteristics, current suicidal intent, past suicide attempt, clinical diagnosis of psychiatric disorders based on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) and socio-environmental stressors (e.g., interpersonal conflicts, financial problems, etc.), the type of pesticide involved (paraquat versus non-paraquat pesticides versus unknown pesticides), and the outcomes at discharge (non-fatal versus fatal). We included only patients aged 15 years or above in our analysis. Age group was defined using 20-year bands (15–34, 35–54, and 55 + years). Ethnic groups were categorised as: Indian, Malay, Chinese, foreigners, and others. ‘Others’ category includes Malaysian indigenous people, and people of other minority ethnic groups. Occupation was categorised as: agricultural worker, non-agricultural worker, unemployed, and unknown.
Statistical analysis
We used descriptive statistics (number and percentage) to examine the characteristics in the whole sample and the characteristics were stratified by the type of pesticide ingested. We also calculated the number and percentage of patients who received the psychiatric assessment. Among assessed patients, we presented the number and percentage of patients with a past suicide attempt and different psychiatric diagnoses. We excluded two variables (DSM-5 diagnosis of psychiatric disorders and past suicide attempt) in the inferential statistical analysis as data were only available for a subgroup of patients who survived and were referred by the primary clinical team for a psychiatric assessment (n = 167, 78.8%). These variables would be negatively associated with fatality due to the selection effect. A p value of < 0.05 was set as the standard for statistical significance. Multinomial logistic regression models were used to investigate the association between the patients’ characteristics (i.e., the independent variables) and the type of pesticides involved (i.e., the dependent variable, with three categories: paraquat versus non-paraquat pesticides versus unknown pesticides). Logistic regression models were used to investigate the association between the patients’ characteristics (i.e., the independent variables) and outcomes at discharge (i.e., the dependent variables, with two categories: non-fatal versus fatal outcomes). Using logistic regression, we calculated the odds ratios (ORs) and sex-age-adjusted ORs and their 95% confidence intervals for the type of pesticides involved and outcomes (i.e., the independent variables in separate models) in relation to the periods before (2015–2019) and after (2020–2021) the 2020 paraquat ban (i.e., the dependent variable: pre-ban versus post-ban) in Malaysia. IBM SPSS Statistics for Windows, version 27 (IBM Corp., Armonk, N.Y., USA), was used for data analysis.
Results
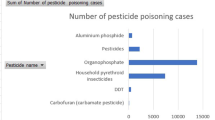
Two hundred and twelve cases of pesticide poisoning from age 15 years and above were identified in the two study hospitals with 42 of these resulted in death (case fatality 19.8%). There were no additional pesticide poisoning deaths identified from state forensic records apart from those identified in hospital-based medical records. Two-thirds (67.5%) were men, 50% were aged 15–34 years, and just under half (44.8%) were people of Indian ethnicity. Agricultural workers comprised slightly over a quarter (27.8%) of cases (Table 1). The majority of cases comprised intentional poisoning (160/212 = 75.5%). Three-quarters (120/160 = 75%) of self-poisoning cases were classified as a suicide attempt. Paraquat accounted for about a third (31.6%) of all pesticide poisonings, while non-paraquat pesticides were involved in approximately half (50.5%) of all cases, with unidentified pesticides (17.9%) used in the remaining cases. (Table 1).
Table 1 shows the comparison of poisonings using paraquat versus non-paraquat versus unknown pesticides. Compared with poisonings using non-paraquat pesticides, paraquat poisoning was associated with agricultural work. Paraquat poisoning had much higher fatality (41.8%) than non-paraquat pesticide poisoning i.e. glyphosate, organophosphate and rodenticide,(12.1%) and unknown pesticide poisoning (2.6%). Compared with non-paraquat pesticide poisoning, the adjusted odds ratio (aOR) of fatality was 6.70 (95% confidence interval [CI] 2.65, 16.92; p < 0.001) for paraquat poisoning. No association was found between the type of pesticides involved and sex, age, ethnicity, current suicidal intent, or acute stressful life events.
Table 2 shows the comparison of non-fatal versus fatal pesticide poisonings. In the fully adjusted analysis, fatality was positively associated with male gender (aOR = 3.88, 95% CI 1.28, 11.76; p = 0.016), current suicidal intent (aOR = 3.69, 95% CI 1.25, 10.84; p = 0.018), and paraquat poisoning (aOR = 7.50, 95% CI 2.83–19.87; p < 0.001). Paraquat was the leading pesticide associated with mortality. It accounted for 66.7% of fatal poisoning cases, while it constituted only 31.6% of all patients (Table 1).
Table 3 shows the comparison of pesticides involved and outcomes at discharge in pesticide poisonings before and after the 2020 paraquat ban. The percentage of paraquat poisoning reduced from 35.8% before the ban to 24.0% after the ban (sex-age-adjusted OR = 0.50, 95% CI 0.26–0.98; p = 0.043). The percentage of fatal poisoning dropped slightly from 21.2% in the pre-ban period to 17.3% in the post-ban period, although there was no statistical evidence for a difference (sex-age-adjusted OR = 0.72, 95% CI 0.34, 1.51; p = 0.38).
Table 4 shows the subgroup of patients who survived and received a psychiatric assessment (167/212 = 78.8%). Among them, 11.4% had previously attempted suicide prior to the index hospital presentation of pesticide poisoning. 42.51% of the patients were diagnosed with a psychiatric disorder. The commonest diagnoses were depressive disorders (39.43%), followed by disorders related to substance and addiction (30.99%).
Table 5 shows that socio-environmental stressors were identified in 62.30% of all cases of pesticide poisoning. The commonest socio-environmental stressors were related to domestic interpersonal conflicts (61.36%), particularly marital conflict (28.79%). Financial problems (13.63%) were the second leading socio-environmental stressors.
Discussion
In a sample of 212 pesticide poisoning case presentations to two hospitals in Malaysia, the overall case fatality was approximately one-fifth. Paraquat was the main pesticide accounting for the burden of mortality. It was involved in less than one-third of poisoning cases while contributed to two-thirds of fatal cases. Paraquat poisoning was associated with a much higher fatality rate (42%). It was very similar to that reported in a very large prospective Sri Lankan cohort [5], than non-paraquat poisoning (12%); as well as agricultural-related work. The overall (paraquat and non-paraquat) pesticide fatality was positively associated with male gender, current suicidal intent, and particularly in paraquat ingestion. Our study demonstrated that the national paraquat ban was associated with a 50% decreased odds of paraquat poisoning. In addition, we found a reducing pesticide poisoning fatality trend in pre- and post- paraquat ban, but we lacked power to detect clinically important effects.
Comparison with previous studies and real-world implementational implications
Pesticide self-poisoning is a major global cause of morbidity and mortality [21]. This phenomenon is particularly significant in agriculture-based low-and middle-income countries in Asia. In contrast, self-poisoning in Western high-income countries are more commonly caused by illicit drugs and medically prescribed drugs [22]. Our findings are consistent with the current global evidence base. It underscores the rationale of national bans of highly toxic pesticides as an effective upstream policy strategy in the prevention of fatal pesticide self-harm and suicide [23]. The timeline and impact of varying levels of paraquat restriction in Malaysia illustrates the challenges of real-world implementation of a total national ban on highly hazardous pesticides. Prior to our study, [16] research has already demonstrated the increase in morbidity of paraquat poisoning at national level when an initial total paraquat ban was reversed. Paraquat use was permitted for selective use and was restricted to four types of agricultural crops, i.e. palm oil, rubber, pineapple, and hill paddy plantation in Malaysia. This was due to concerns on the availability of substitutes for pest control from the end-users in the plantation sector, e.g. farmers and agricultural corporations. Such phenomenon highlights the tension between balancing the seemingly different priorities from a health versus agro-economic perspective.
Nevertheless, it is evident that both priorities are not mutually exclusive - crop yield was not negatively impacted after paraquat bans in South Korea [24] and Taiwan [25]. In low-and-middle-income countries, uncompromised agricultural output has also been shown after national bans of other highly hazardous pesticides such as monocrotophos, methamidophos, and endosulfan in Sri Lanka [26] and India [27]. In Bangladesh, pesticide bans were significantly associated with a reduction of pesticide suicide death rate, albeit with a slight increase in hanging suicides which may suggest a possible substitution of suicide methods. Nevertheless, the number of overall unnatural deaths declined from 14/100,000 to 10.5/100,000 [21]. In Sri Lanka, import controls of highly hazardous pesticides have reduced pesticide suicides [28]. In addition, Lee et al. (2021) [29] showed that bans of highly hazardous pesticides are highly cost-effective in low-and-middle-income countries, particularly in countries with a greater proportion of suicides attributable to pesticide poisoning such as Malaysia. Pesticide suicides are the 2nd most common method of suicide accounting for 13.11% of national suicide deaths [30]. Collaborative approach across sectors such as agriculture, economy, and public health can potentially be highlighted in policy advocacy and stakeholder engagement for the sustainable implementation of national pesticide bans. The public health gains of reduced premature mortality from pesticide suicides is aligned with the United Nations’ 3rd Sustainable Development Goals (SDG) target indicator of reducing suicide rate [31]. The target indicator is implemented in the context of prioritizing limited resources in suicide prevention efforts within the global majority of developing nations. At the same time, the agricultural community’s concerns of maintaining crop productivity and food security for the general public can be addressed by building their awareness and capacity. A whole society approach i.e. public, industry and non-governmental organizations can be taken to support sustainable access to alternatives of highly hazardous pesticides for safe and effective pest-control. For instance, the Malaysian-based Pesticide Action Network Asia Pacific (PANAP) organized an innovative capacity-building program to empower local farmers in Cameron Highlands, a major Malaysian agricultural community, with the knowledge of biological solutions and other environmentally-friendly, non-pesticide and economically-viable agricultural methods in 2016 [32].
Such initiatives are crucial to reduce the market demand for illegal paraquat in tandem with enforcement by pesticide regulators. The enforcement was in place amidst reports of failed paraquat smuggling attempts in 2021, a year after the paraquat ban was announced [33]. After the implementation of the national paraquat ban, it is crucial for continuous and sustainable surveillance nationally and regionally in South-East-Asia to ensure that any access to illegal paraquat, including the pre-existing stock prior to the ban, is completely removed. For example, the Department of Agriculture investigates reports of paraquat poisoning after the paraquat ban including tracing the illegal source of paraquat i.e. sales site(s). However, such enforcement procedures depend on the awareness and act of reporting at the community level. Bottom-up and top-down approaches are critical in ensuring the success of real-world implementation of the paraquat ban.
A previous study from India (n = 7753) suggested that centralized pesticide storage in locked boxes was feasible and may play a role in preventing rural pesticide suicides [34] Such study, of note was a relatively small study and indicated that many pesticide users opted not to use the facility. However, a more recent and larger (n = 223,861) randomized controlled trial of household lockable pesticide storage in rural Sri Lanka did not show any evidence of reduction in pesticide suicide deaths [35]. In Malaysian context, it is implausible that improved storage of pesticides would significantly reduce rates of fatal pesticide self-poisoning due to the place of storage. Pesticides in rural farming communities are usually stored in or within the vicinity of longhouses that typically accommodates multiple households in one of our study sites, Bintulu town. Longhouse accommodation is a norm in the state of Sarawak. Effective restriction of access to lethal pesticides via pesticide safe storage appears impractical in such communal communities [36].
Further research with reliable surveillance by the National Suicide and Fatal Injury Registry Malaysia (NSFIRM) is currently being developed by the Malaysian Ministry of Health and relevant stakeholders. NSFIRM is expected to be fully implemented by 2023 [37]. NSFIRM would be utilized to monitor future trends of suicide rates and ascertain whether findings from our current study that showed a 50% reduction of paraquat pesticide poisonings, as well as the suggestion of a reducing trend in fatal pesticide poisonings, are reflective of a national reduction in pesticide poisonings. The current global evidence base suggests that paraquat bans also reduce overall suicide deaths on top of pesticide suicide deaths across high-income nations such as Korea [38] and Taiwan, albeit only in the elderly Taiwanese population [25]; as well as low-and-middle-income settings in Sri Lanka [10]. Whether or not Malaysia will experience reduced overall suicide rates in anticipation of a reducing trend of fatal pesticide self-poisoning post-paraquat ban, or any shift in terms of method substitution in the longer term, remains to be ascertained in larger-scale and more comprehensive studies in the future.
Our study has also highlighted the possibility of an evolving sociodemographic landscape associated with the risk of morbidity and mortality from pesticide poisoning. Male gender was four times more significantly associated with the fatal outcome of pesticide poisoning compared to female gender in our study sample which is consistent with recent local studies [39, 40]. This is in contrast with Maniam et al’s, 1988 study in Cameron Highlands, a major agricultural community in West Malaysia. The study highlighted the higher rate of suicidal and non-suicidal fatal pesticide self-poisoning deaths among young women compared to men before the turn of the 21st century. Our study findings converge with an emerging epidemiological shift of a gender “re-reversal” of higher female to male ratio of suicide rates in Asian LMICs such as China [41] and India [42]. It is mainly contributed by high rates of fatal pesticide self-poisoning deaths in young rural women; to an overall higher male to female suicide ratio which is currently found in more recent Chinese [43] and Indian [44, 45] studies. This phenomenon appears to gravitate towards a more Western, HIC pattern of gender suicide ratio. It can be attributed to an interplay of multiple factors such as urbanization, modernisation, improved socio-economic empowerment of women due to female rural-urban migration accompanied by a more rapid reduction of female suicide rates, especially due to rural pesticide self-poisoning [46, 47] in tandem with gradually increasing male-to-female ratio of suicide deaths [48].
The Malaysian agricultural workforce is currently male-dominated at 79.2% in 2019 [49]. The manually labour-intensive task of herbicide application was primarily carried out by men (92.8%) instead of women in farming families in the state of Perak. This highlights the higher access and exposure of men to pesticides in agricultural-work settings [50]. Furthermore, concurrent with Malaysia’s rapid economic growth and urbanization [51], the female labour force participation has increased, particularly in the manufacturing and services sector. Only a minority of women (22%) worked in the agricultural sector [52]. Thus, such gender demographics in the Malaysian agricultural sector may contribute to the increased vulnerability of pesticide poisoning fatalities in men.
Although ethnicity was not found to be significantly associated with the type and outcome of pesticide poisoning, Indian ethnicity was markedly over-represented (44.8%) in our study sample as the Indian ethnic composition in Malaysia was much lower at 7.3% nationally, 11.3% in Perak and < 0.6% in Sarawak [53]. Previous studies have consistently shown that Indian ethnicity was significantly associated with higher rates of suicidal behaviour (ideation, fatal and non-fatal suicide attempt) in Malaysia [14, 54, 55], in particular among Indians of the Hindu faith [56]. Some authors have postulated that Malaysian Indians are more vulnerable to socioeconomic inequalities and political marginalization as a minority ethnic group in a multicultural society, thus increasing the risk of suicide in this population [57,58,59,60]. In addition, Hinduism, the religion professed by the majority (80%) of Malaysian Indians, arguably adopts a more ambivalent stance in terms of suicide acceptability [57, 60, 61]. Therefore, Hindusim has been viewed as possibly less suicide-protective compared to the other religions practiced by the Indian diaspora i.e. Buddhism-Taosim, Christianity, and Islam.
Findings from our study suggest that socio-environmental stressors may play a bigger role in pesticide poisonings compared to diagnosable psychiatric disorders. 62% of pesticide poisoning cases experienced some form of socio-environmental stressor. Domestic interpersonal conflict, especially marital, was the most common followed by financial problems. These findings are congruent with socio-environmental precipitants of pesticide self-poisoining in China and South Asia [62, 63]. Furthermore, less than half (42.5%) of pesticide poisoining cases referred for a psychiatric assessment in our study sample were diagnosed with any psychiatric disorder. Our findings resonate with previous research that showed a lower rate of psychiatric disorders with regards to suicidal behaviour in LMIC compared to HIC populations [64]. In addition, depressive disorders were the commonest type of psychiatric disorder in our sample with a proportion (39.4%); albeit at a lower rate compared to the higher prevalance of depression (67.8%) among pesticide self-poisoining patients in Taiwan [65]. Further research is warranted to elucidate the complex interplay between cultural heterogeneity, national income-status, accesibility to mental health services and social determinants of mental health as risk and protective factors in the context of upstream and downstream targets of pesticide self-poisoining prevention.
Our study showed that suicidal intent (intent to kill oneself) was present in the majority (75%) of patients with pesticide self-poisoning, in contrast with the view that most fatal cases of pesticide self-poisoning in LMICs were likely to be non-suicidal acts of self-harm (intentional pesticide poisoining without intent to die) [66, 67]. Morover, other studies from Morroco [68], Nepal (Gyenwali et al., 2017) and Uganda [69] have also found that the majority of pesticide poisoning cases were suicidal in nature. Thus, beyond universal strategies such as banning lethal pesticides and improving social protection at the population level, a comprehensive and holistic approach in pesticide suicide prevention can be employed. It includes the identification of suicidal ideation as a proximal target for intervention in at risk individuals who may not necessarily have a diagnosable psychiatric disorder. Randomized-controlled trials are currently being piloted in Sri Lanka to test the effectivenessness of interventions aimed at reducing pesticide self-poisoning attempts at the community level via gatekeeper training for pesticide vendors [70], as well as hospital-level, nurse-led, single-session counseling for non-fatal self-poisoining patients that focuses on building coping strategies to ameriolate interpersonal conflict-related psychological distress [71].
Strengths and limitations
To the best of our knowledge, this is the first Malaysian study evaluating the impact of a national paraquat ban on fatal and non-fatal outcomes of pesticide poisoning among a culturally heterogenous clinical population. Furthermore, we comprehensively captured all pesticide poisoning deaths within our study sites’ catchment areas by utilising state-wide forensic data that potentially included patients who were dead at discovery but were not sent to hospitals (although none were detected).
Our study was limited by a relatively small sample size which increases the risk of type II error. Although we included hospitals from two different Malaysian states in West and East Malaysia respectively, limitations still arise in terms of the generalizability and national representativeness of our findings to the other 11 states and 3 federal territories in Malaysia. We faced constraints with regards to data validity in terms of the risk of misclassification due to coding errors based on our retrospective clinical medical records-based study design, in particular from our West Malaysian state hospital data in which ICD-10 classification was not fully implemented. In addition, psychiatric diagnoses were designed based on clinical assessment according to the DSM-5 criteria rather than validated research tools, thus raising the possibility of missed diagnosis by the frontline, non-mental health clinicians, particularly in the proportion of patients (21.2%) who were not referred for psychiatric assessment, either due to being too ill or not having survived. When interpreting our study findings, it is important to understand that the impact of the national paraquat ban may not have been fully captured within our relatively short study period due to the timeline of the ban’s implementation. 1 year of sales ban (2020) was implemented followed by another year of total usage ban (2021). Existing stock of paraquat might have still been accessible in year 2020. In view of our study duration spanning the period before and during the COVID-19 pandemic, another unstudied confounding variable is the effect of lock-down measures on the accessibility to pesticides as a means of self-poisoning pre- and post- paraquat ban.
We recognize our study’s limitation of not including length of stay in our analysis. We appreciate the importance of length of stay as a potentially significant variable in this study. However, due to the multiple confounders that affect the length of stay i.e. volume and amount of pesticide ingested and time from ingestion to hospital presentation whereby reliable data were not available due to the retrospective nature of the study, we focused instead on the type of pesticide (paraquat versus non-paraquat) which differed in the lethality as a more objective variable in examining the outcome of pesticide poisoning. In addition, we also acknowledge the lack of data on the comparison of pesticide poisoning methods (i.e. route of exposure of ingestion/inhalation/skin) as a study limitation. Nevertheless, previous literature has shown that ingestion is the most common route of exposure for intentional pesticide poisoning [72].
Conclusions
Our data showed that paraquat was the leading pesticide associated with pesticide poisoning mortality in a Malaysian sample. Males and agricultural workers appear to be potential at-risk target groups for focused strategies to prevent fatal pesticide poisoning. Suicidal intent was predominant in majority of cases. This highlights the need for identification and early psycho-social interventions of suicidal crisis in the context of more commonly occurring socio-environmental stressors such as interpersonal conflicts and financial problems instead of merely focusing on the medical treatment of diagnosable psychiatric disorders which were less prevalent compared to HIC settings. Our data demonstrated that the 2020 Malaysian national paraquat ban was significantly associated with the preliminary finding of a reduction in the percentage of paraquat poisoning. In addition, we found a reducing trend in the overall fatality of pesticide poisoning. These findings add further evidence to the global data in terms of the effectiveness of high-level national policy change in reducing pesticide poisoning morbidity and mortality. Future research is required to evaluate the long-term implementational sustainability and impact of the national paraquat ban on overall rates (including non-pesticide methods) of fatal self-harm and suicide in Malaysia.
Data Availability
The datasets generated and/or analysed during the current study are not publicly available due confidentiality and privacy purposes but are available from the corresponding author on reasonable request.
Abbreviations
- HB:
-
Bintulu Hospital
- HRPB:
-
Raja Permaisuri Bainun Hospital
- LMIC:
-
Low-and-middle-income countries
- HIC:
-
High-income-countries
- NSFIRM:
-
The National Suicide and Fatal Injury Registry Malaysia
References
World Health Organization. Preventing suicide: a resource for pesticide registrars and regulators. World Health Organization (WHO); 2019. p. 36.
Mew EJ, Padmanathan P, Konradsen F, Eddleston M, Chang S-S, Phillips MR, et al. The global burden of fatal self-poisoning with pesticides 2006-15: systematic review. J Affect Disord. 2017;219:93–104.
Eddleston M, Karunaratne A, Weerakoon M, Kumarasinghe S, Rajapakshe M, Rezvi Sheriff M, et al. Choice of poison for intentional self-poisoning in rural Sri Lanka. Clin Toxicol. 2006;44(3):283–6.
Jiang C, Li X, Phillips MR, Xu Y. Matched case-control study of medically serious attempted suicides in rural China. Shanghai archives of psychiatry. 2013;25(1):22.
Buckley NA, Fahim M, Raubenheimer J, Gawarammana IB, Eddleston M, Roberts MS, et al. Case fatality of agricultural pesticides after self-poisoning in Sri Lanka: a prospective cohort study. The Lancet Global Health. 2021;9(6):e854–e62.
Gunnell D, Knipe D, Chang SS, Pearson M, Konradsen F, Lee WJ, et al. Prevention of suicide with regulations aimed at restricting access to highly hazardous pesticides: a systematic review of the international evidence. Lancet Glob Health. 2017;5(10):e1026–e37.
Elenga N, Merlin C, Le Guern R, Kom-Tchameni R, Ducrot Y-M, Pradier M et al. Clinical features and prognosis of paraquat poisoning in french Guiana: a review of 62 cases. Medicine. 2018;97(15).
Cha ES, Chang S-S, Gunnell D, Eddleston M, Khang Y-H, Lee WJ. Impact of paraquat regulation on suicide in South Korea. Int J Epidemiol. 2015;45(2):470–9.
Chang S-S, Lin C-Y, Lee M-B, Shen L-J, Gunnell D, Eddleston M. The early impact of paraquat ban on suicide in Taiwan. Clin Toxicol. 2021:1–5.
Knipe DW, Chang SS, Dawson A, Eddleston M, Konradsen F, Metcalfe C, et al. Suicide prevention through means restriction: impact of the 2008–2011 pesticide restrictions on suicide in Sri Lanka. PLoS ONE. 2017;12(3):e0172893.
Hirschmann R. Palm oil industry in Malaysia - statistics & facts Statista: Statista; 2022 [updated 22 March 2022. Available from: https://www.statista.com/topics/5814/palm-oil-industry-in-malaysia/#dossierContents__outerWrapper.
The World Bank. World Bank Open Data - Data - Malaysia worldbank.org: The World Bank Group; 2021 [Available from: https://data.worldbank.org/country/MY.
Nor Hayati Ali NN, Yushada Budiman NH, Arif. Sharifah Suziah Syed Mokhtar, Mohd Shah Mahmood, Bhupinder Singh, Zahari Noor, Nurliza Abdullah, Khairul Anuar Zainun, Nurul Kharmila Abdullah, Abdul Muneer Hamid Badi’ah Yahya, Norliza Che Mi, Salina Aziz, Riana Abdul Rahim, Uma Visvalingam, Selvasingam Ratnasingam. National Suicide Registry Malaysia Annual Report. In: Registry NS, editor.: Ministry of Health Malaysia; 2009.
Armitage CJ, Panagioti M, Rahim WA, Rowe R, O’Connor RC. Completed suicides and self-harm in Malaysia: a systematic review. Gen Hosp Psychiatry. 2015;37(2):153–65.
Kamaruzaman NA, Leong Y-H, Jaafar MH, Mohamed Khan HR, Abdul Rani NA, Razali MF, et al. Epidemiology and risk factors of pesticide poisoning in Malaysia: a retrospective analysis by the national poison centre (NPC) from 2006 to 2015. BMJ Open. 2020;10(6):e036048.
Leong YH, Ariff AM, Khan HRM, Rani NAA, Majid MIA. Paraquat poisoning calls to the Malaysia National poison centre following its ban and subsequent restriction of the herbicide from 2004 to 2015. J Forensic Leg Med. 2018;56:16–20.
Fatimah Zainal ALaHS. Sale of paraquat illegal from January. The Star. 2019.
Thundiyil JG, Stober J, Besbelli N, Pronczuk J. Acute pesticide poisoning: a proposed classification tool. Bull World Health Organ. 2008;86(3):205–9.
Prevention CfDCa. Environmental Hazards and Health Effects.
Prevention CfDCa. Facts about Paraquat. Centers for Disease Control and Prevention; 2018.
Chowdhury FR, Dewan G, Verma VR, Knipe DW, Isha IT, Faiz MA, et al. Bans of WHO class I pesticides in Bangladesh—suicide prevention without hampering agricultural output. Int J Epidemiol. 2018;47(1):175–84.
Albano GD, Malta G, La Spina C, Rifiorito A, Provenzano V, Triolo V, et al. Toxicological findings of self-poisoning suicidal deaths: a systematic review by countries. Toxics. 2022;10(11):654.
Gunnell D, Knipe D, Chang S-S, Pearson M, Konradsen F, Lee WJ, et al. Prevention of suicide with regulations aimed at restricting access to highly hazardous pesticides: a systematic review of the international evidence. The Lancet Global Health. 2017;5(10):e1026–e37.
Cha ES, Chang S-S, Gunnell D, Eddleston M, Khang Y-H, Lee WJ. Impact of paraquat regulation on suicide in South Korea. Int J Epidemiol. 2016;45(2):470–9.
Chang S-S, Lin C-Y, Lee M-B, Shen L-J, Gunnell D, Eddleston M. The early impact of paraquat ban on suicide in Taiwan. Clin Toxicol. 2022;60(1):131–5.
Manuweera G, Eddleston M, Egodage S, Buckley NA. Do targeted bans of insecticides to prevent deaths from self-poisoning result in reduced agricultural output? Environ Health Perspect. 2008;116(4):492–5.
Bonvoisin T, Utyasheva L, Knipe D, Gunnell D, Eddleston M. Suicide by pesticide poisoning in India: a review of pesticide regulations and their impact on suicide trends. BMC Public Health. 2020;20(1):1–16.
Gunnell D, Fernando R, Hewagama M, Priyangika W, Konradsen F, Eddleston M. The impact of pesticide regulations on suicide in Sri Lanka. Int J Epidemiol. 2007;36(6):1235–42.
Lee Y, Chisholm D, Eddleston M, Gunnell D, Fleischmann A, Konradsen F, et al. The cost-effectiveness of banning highly hazardous pesticides to prevent suicides due to pesticide self-ingestion across 14 countries: an economic modelling study. The Lancet Global Health. 2021;9(3):e291–e300.
Nor Hayati Ali NN, Yushada Budiman NH, Arif. Sharifah Suziah Syed Mokhtar, Mohd Shah Mahmood, Bhupinder Singh, Zahari Noor, Nurliza Abdullah, Khairul Anuar Zainun, Nurul Kharmila Abdullah, Abdul Muneer Hamid Badi’ah Yahya, Norliza Che Mi, Salina Aziz, Riana Abdul Rahim, Uma Visvalingam, Selvasingam Ratnasingam. National Suicide Registry Malaysia Annual Report Ministry of Health Malaysia. 2009.
Platform GSI. Global SDG Data & Indicators At Year Five. Global SDG Indicator Platform. 2020.
Naguran M. Cameron Highlands Farmer Field School for Pesticide-free food. Gaia Discovery; 2016.
Hilmy I. Agriculture Dept foils attempt to smuggle in 17,600kg of banned pesticide. The Star. 2021.
Vijayakumar L, Jeyaseelan L, Kumar S, Mohanraj R, Devika S, Manikandan S. A central storage facility to reduce pesticide suicides-a feasibility study from India. BMC Public Health. 2013;13(1):1–10.
Pearson M, Metcalfe C, Jayamanne S, Gunnell D, Weerasinghe M, Pieris R, et al. Effectiveness of household lockable pesticide storage to reduce pesticide self-poisoning in rural Asia: a community-based, cluster-randomised controlled trial. The Lancet. 2017;390(10105):1863–72.
Whittle B, Rengam SV. Communities in peril: asian regional report on community monitoring of highly hazardous pesticide use. PANAP; 2010.
Lew B, Kõlves K, Lester D, Chen WS, bt Ibrahim N, bt Khamal NR et al. Looking into recent suicide rates and trends in Malaysia: a comparative analysis. Front Psychiatry. 2021;12.
Kim J-W, Kim D-S. Paraquat: toxicology and impacts of its ban on human health and agriculture. Weed Sci. 2020;68(3):208–13.
Tan J-T, Letchuman Ramanathan G, Choy M-P, Leela R, Lim B. Paraquat poisoning: experience in hospital taiping (year 2008-october 2011). Med J Malaysia. 2013;68(5):384–8.
Kamaruzaman NA, Leong Y-H, Jaafar MH, Khan HRM, Rani NAA, Razali MF, et al. Epidemiology and risk factors of pesticide poisoning in Malaysia: a retrospective analysis by the national poison centre (NPC) from 2006 to 2015. BMJ open. 2020;10(6):e036048.
Phillips MR, Li X, Zhang Y. Suicide rates in China, 1995–99. The Lancet. 2002;359(9309):835–40.
Mayer P, Ziaian T. Suicide, gender, and age variations in India: are women in indian society protected from suicide? Crisis: The Journal of Crisis Intervention and Suicide Prevention. 2002;23(3):98.
Jiang H, Niu L, Hahne J, Hu M, Fang J, Shen M, et al. Changing of suicide rates in China, 2002–2015. J Affect Disord. 2018;240:165–70.
Anil R, Nadkarni A. Suicide in India: a systematic review. Shanghai archives of psychiatry. 2014;26(2):69.
Arya V, Page A, River J, Armstrong G, Mayer P. Trends and socio-economic determinants of suicide in India: 2001–2013. Soc Psychiatry Psychiatr Epidemiol. 2018;53(3):269–78.
Wang C-W, Chan CL, Yip PS. Suicide rates in China from 2002 to 2011: an update. Soc Psychiatry Psychiatr Epidemiol. 2014;49(6):929–41.
Wu KC-C, Chen Y-Y, Yip PS. Suicide methods in Asia: implications in suicide prevention. Int J Environ Res Public Health. 2012;9(4):1135–58.
Tong Y, Phillips MR, Yin Y, Lan Z. Relationship of the high proportion of suicidal acts involving ingestion of pesticides to the low male-to-female ratio of suicide rates in China. Epidemiol psychiatric Sci. 2020;29.
Malaysia DoS. Selected Agricultural Indicators, Malaysia 2021.
Ahmad A, Ismail N. Gender roles in malysian agriculture: implications for extension planning. J Int Agricultural Ext Educ. 1998;2(1):17–25.
Qinfen M. Female labour force participation in Malaysia: timeseries evidence. South East Asia Journal of Contemporary Business Economics and Law. 2017;14(3):1–7.
Shaharudin A, Rahim M. Agriculture Exodus? Insights from youth aspirations. Kuala Lumpur, Khazanah Research Institute; 2020.
Malaysia DoS. Demographics Statistics Third Quarter 2021. 2021.
Maniam T, Marhani M, Firdaus M, Kadir A, Mazni M, Azizul A, et al. Risk factors for suicidal ideation, plans and attempts in Malaysia—Results of an epidemiological survey. Compr Psychiatr. 2014;55:121–S5.
Ali NH, Zainun KA, Bahar N, Haniff J, Hamid AM, Bujang MAH, et al. Pattern of suicides in 2009: data from the national suicide Registry M alaysia. Asia-Pacific Psychiatry. 2014;6(2):217–25.
Maniam T, Chinna K, Lim C, Kadir A, Nurashikin I, Salina A, et al. Suicide prevention program for at-risk groups: pointers from an epidemiological study. Prev Med. 2013;57:45–S6.
Chan LF, Thambu M. Cultural factors in suicide prevention. The international handbook of suicide prevention. 2016:541 – 55.
Lian KF. The political and economic marginalization of Tamils in Malaysia. Race, Ethnicity, and the State in Malaysia and Singapore: Brill; 2006. p. 121 – 67.
Khalid MA, Yang L. Income inequality among different ethnic groups: the case of Malaysia. LSE Business Review; 2019.
Singh K. Challenges to the rights of Malaysians of indian descent. E-International Relations. 2013;6:1–17.
Vijayakumar L, John S. Is Hinduism ambivalent about suicide? Int J Soc Psychiatry. 2018;64(5):443–9.
Kumar RS, Hashim U. Characteristics of suicidal attempts among farmers in rural South India. Industrial psychiatry journal. 2017;26(1):28.
Zhu R-T, Ma Z, Jia C, Zhou L. Suicide means used by the older adults in rural China: a comparison between those using pesticides and other means. J Geriatr Psychiatr Neurol. 2019;32(6):319–26.
Knipe D, Williams AJ, Hannam-Swain S, Upton S, Brown K, Bandara P, et al. Psychiatric morbidity and suicidal behaviour in low-and middle-income countries: a systematic review and meta-analysis. PLoS Med. 2019;16(10):e1002905.
Tu C-Y, Yen T-H, Chang C-M, Chen H-Y, Yen Y-C, Guo M-C, et al. Characteristics and psychopathology of 1,086 patients who self-poisoned using pesticides in Taiwan (2012–2019): a comparison across pesticide groups. J Affect Disord. 2022;300:17–26.
Mannekote Thippaiah S, Shankarapura Nanjappa M, Gude JG, Voyiaziakis E, Patwa S, Birur B, et al. Non-suicidal self-injury in developing countries: a review. Int J Soc Psychiatry. 2021;67(5):472–82.
Sun L, Zhang J. Characteristics of chinese rural young suicides: who did not have a strong intent to die. Compr Psychiatr. 2015;57:73–8.
Nabih Z, Amiar L, Abidli Z, Windy M, Soulaymani A, Mokhtari A et al. Epidemiology and risk factors of voluntary pesticide poisoning in Morocco (2008–2014). Epidemiol health. 2017;39.
Odakha JA, Harborne D, Chen H. Predictors of mortality in emergency centre patients with acute pesticide poisoning in Uganda. Afr J Emerg Med. 2022;12(3):242–5.
Weerasinghe M, Pearson M, Turner N, Metcalfe C, Gunnell DJ, Agampodi S, et al. Gatekeeper training for vendors to reduce pesticide self-poisoning in rural South Asia: a study protocol for a stepped-wedge cluster randomised controlled trial. BMJ open. 2022;12(4):e054061.
De Silva A, Dawson AH, Gawarammana IB, Tennakoon S, Rajapakse T. Study protocol: a pilot randomized controlled trial to evaluate the acceptability and feasibility of a counseling intervention, delivered by nurses, for those who have attempted self-poisoning in Sri Lanka. Pilot and feasibility studies. 2018;4(1):1–9.
Rajapakse T, Griffiths KM, Christensen H, Cotton S. Non-fatal self-poisoning in Sri Lanka: associated triggers and motivations. BMC Public Health. 2015;15(1):1–7.
Acknowledgements
The authors wish to thank Professor Emeritus David Gunnell (University of Bristol) for his expert advice and review of this article. We would like to thank the Director of General Ministry of Health Malaysia for his permission to publish this article.
Funding
This research was supported by a grant from the Centre for Pesticide Suicide Prevention, University Of Edinburgh (Grant number: FF-2020-307) to Lai Fong Chan (primary investigator).
Author information
Authors and Affiliations
Contributions
L.F.C.: conceptualization, methodology, formal analysis, resources, data curation, writing original draft, review and editing, supervision, project administration, funding acquisition S.J.C.: formal analysis, investigation, data curation, writing original draft, review and editing, project administrationT.H.L.: conceptualization, methodology, resources, data curation, writing: review and editing, supervision, project administrationR.R.P.: conceptualization, methodology, resources, data curation, writing: review and editing, supervision, project administrationS.S.C.: conceptualization, methodology, formal analysis, resources, data curation, writing original draft, review and editing, supervision, funding acquisition H.Y.C.: formal analysis, resources, data curation, writing original draft, review and editing, A.R.M.: formal analysis, investigation, data curation, writing review and editing, project administrationF.H.A.R.: formal analysis, investigation, data curation, writing review and editing, project administrationL.U.: conceptualization, methodology, formal analysis, resources, writing review and editing, supervision, project administration, funding acquisition M.E.: conceptualization, methodology, formal analysis, resources, writing review and editing, supervision, project administration, funding acquisition All authors approved the final version of the article.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Ethics approval and consent to participate
We confirm that all experiments were performed in accordance with relevant guidelines and regulations (such as the Declaration of Helsinki). Ethics approval for this study was obtained from Medical Research Ethics Committee, Ministry of Health, Malaysia (MREC: NMRR-20-892-54891), and the National University of Malaysia Ethics Committee (FF-2020-307). The need for informed consent to participate in the study was waived by the National University of Malaysia Ethics Committee, and the Medical Research Ethics Committee, Ministry of Health; as the data collection was based on hospital medical records and did not involve any human study participants.
Consent for publication
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
12888_2023_4974_MOESM1_ESM.docx
Supplementary Material 1 Annual number of pesticide poisoning patients by pesticides involved and outcome in Bintulu Hospital (HB) and Raja Permaisuri Bainun Hospital (HRPB), Malaysia.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Chan, L.F., Chin, S.J., Loo, T.H. et al. Surveillance of pesticide poisoning in an East and a West Malaysian hospital: characteristics of pesticide poisoning and the early impact of a national Paraquat ban. BMC Psychiatry 23, 472 (2023). https://doi.org/10.1186/s12888-023-04974-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12888-023-04974-8