Abstract
Background
Lung recruitment is a maneuver used to decrease the length of intubation in preterm neonates. This study aimed to compare the therapeutic efficacy of lung recruitment plus intubation-surfactant-extubation (INSURE) procedure and INSURE alone for the preterm neonates with respiratory distress syndrome.
Methods
From 2017 to 2019, 184 preterm neonates (gestational age 24–32 weeks) with respiratory distress syndrome were enrolled and randomized into the lung recruitment group receiving lung recruitment (25 cm H2O, 15 s) plus INSURE and the control group receiving INSURE only. The primary outcome was the need for mechanical ventilation (MV) within 72 h after extubation. The secondary outcomes included duration of MV, noninvasive ventilation, total oxygen therapy, hospitalization time, and complications.
Results
Compared to the control group, the lung recruitment group had a significantly lower proportion of preterm neonates requiring MV within 72 h after extubation (23% vs. 38%, P = 0.025) and pulmonary surfactant administration, as well as a shorter MV duration. There was no significant difference in the incidences of complications (all P > 0.05) and in-hospital mortality (2% vs. 4%, P = 0.4) between the lung recruitment group and control group. Multivariate logistic regression analysis demonstrated that the control group had a 2.17-time higher risk of requiring MV than the lung recruitment group (AOR: 2.17, 95% CI: 1.13–4.18; P = 0.021). Compared with infants with a normotensive mother, infants with a hypertensive mother have a 2.41-time higher risk of requiring MV (AOR: 2.41, 95% CI: 1.15–5.05; P = 0.020).
Conclusion
Lung recruitment plus INSURE can reduce the need for MV within 72 h after extubation and did not increase the incidence of complications and mortality.
Trial registration
Chinese Clinical Trial Registry ChiCTR1800020125, retrospectively registered on December 15, 2018.
Similar content being viewed by others
Background
Neonatal respiratory distress syndrome (RDS) is a leading cause of morbidity in preterm neonates, which is caused by pulmonary surfactant insufficiency and pulmonary structural immaturity [1]. The purpose of the management of RDS is to maximize survival and minimize potential adverse effects. According to the European Consensus Guidelines for the Management of RDS, preterm infants should receive Continuous positive airway pressure (CPAP) of at least 6 cm H2O via mask or nasal prongs to stabilize spontaneously breathing [2]. Persistently apneic or bradycardic infants should be given gentle positive pressure lung inflation with peak inspiratory pressure of 20–25 cm H2O [2]. The European Consensus Guideline also suggests that INSURE strategy should be considered for infants who failed in CPAP treatment [3]. The INSURE technique consists of an INtubation-SURfactant-Extubation procedure, which can reduce the need for mandatory ventilation (MV) and, the duration of respiratory support in preterm infants with RDS [4].
Lung recruitment is a maneuver with a peak pressure of 25–30cmH2O for 10–20 s [5]. It is used for preterm infants with respiratory failure and RDS to ensure early and effective creation of functional residual capacity (FRC) to prevent lung damage [6, 7]. Previous animal studies have shown that lung inflation can provide more stable tidal volume and uniform lung ventilation with improved FRC than intermittent ventilation [8, 9]. Clinical trials also demonstrate that preterm infants with RDS receiving lung recruitment at birth can decrease the need for MV [9,10,11,12]. Nevertheless, contradicting these findings, some trials reported that lung inflation has no superior effect [13, 14]. A review by Bruschettini et al. suggests that there is no evidence supporting that lung inflation is superior to IPPV in terms of MV requirement and other important respiratory outcomes [15]. On the other hand, in China, lung recruitment has not been extensively applied in clinical practice.
To further evaluate the therapeutic efficacy and safety of lung recruitment, this study aimed to compare the therapeutic efficacy of lung recruitment plus INSURE and INSURE alone in preterm neonates with RDS.
Methods
Participants and study design
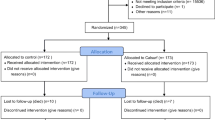
This was a prospective randomized controlled trial. Between 2017 and 2019, 184 preterm neonates with RDS treated in the Department of Neonatology in Dongguan Maternal and Child Health Hospital were enrolled and randomized into the lung recruitment group and the control group. This trial was registered at the Chinese Clinical Trial Registry (ChiCTR1800020125). The trial flow diagram was shown in Fig. 1.
Inclusion criteria were: 1) infants with gestational age from 24 to 32 weeks; 2) birth weight less than or equal to1800 g; 3) definite diagnosis of RDS by clinical syndrome and X-ray findings; 4) failure in CPAP treatment within 24 h after the parent’s consent. The infants with severe congenital malformation or required endotracheal intubation in the delivery room were excluded. This study was approved by the institutional review board of our hospital. Written informed consent was obtained from the parents. Our study adheres to CONSORT guidelines.
Sample size calculation
We hypothesized that lung recruitment with INSURE could reduce the probability of mechanical ventilation after conventional INSURE therapy from 50 to 30%. The sample size was increased to 184 cases to achieve a power of 80% (a = 0.05).
Randomization and treatment
The sequence numbers were kept in opaque sealed envelopes that were opened just before infants meet the inclusion criteria but not the exclusion criteria by a person not involving in the management of the infants. The infants in the lung recruitment group were intubated, and then received lung recruitment (25 cmH2O, 15 s) by a T-piece resuscitator and pulmonary surfactant (200 mg/Kg, as an early rescue therapy). The infants in the control group were intubated and then received pulmonary surfactant (200 mg/Kg). After the catheter was removed, the infants received CPAP therapy (6–8 cmH2O). Infants who failed in CPAP treatment after INSURE therapy were switched to mechanical ventilation with endotracheal intubation. A failure in CPAP treatment was defined as any of the following conditions: 1) inspired oxygen (FiO2) was equal to 0.4 or greater to maintain SpO2 at 88–94% for at least 30 min; 2) arterial blood gas analysis revealed respiratory acidosis: pCO2 > 65 mmHg (8.5 kPa), pH < 7.20; 3) more than 4 apneas per hour, or more than 2 severe apneas requiring positive pressure ventilation with a bag valve mask. The ventilator conditions were set as follows: PIP20-22cmH2O, PEEP5-6cmH2O, RR30–40 beats/min to maintain VT4–6 ml/kg pCO2 40–60 mmHg. Mechanical ventilation can be stopped when the infants reached the following conditions: FiO2 ≤ 0.3, MAP≤8 cmH2O, pCO2 ≤ 55 mmHg, pH ≥7.25, SpO2 ≥ 88% for more than 8 h, and hemodynamics were stable. After extubation, the infants received CPAP (6–8 cmH2O). In the control group, all infants also received INSURE and endotracheal intubation, but not lung recruitment. The other procedures were the same as the intervention group. All infants meeting the CPAP failure criteria again within 12–24 h after extubation were given a second dose of surfactant (100 mg/kg) by the same methods in both the lung recruitment or control group.
Outcome measures
The following data were recorded: durations of MV, noninvasive ventilation, total oxygen therapy, and hospitalization and the complications, including pneumothorax, intraventricular hemorrhage (IVH), necrotizing enterocolitis (NEC), retinopathy of prematurity (ROP), patent ductus arteriosus (PDA), persistent pulmonary hypertension (PPHN), bronchopulmonary dysplasia (BPD) and death. The IVH was defined as a spectrum of hemorrhage brain injury most typically occurring in the first week of life in very preterm babies according to the NIH Consensus Development Conference [16]. BPD was defined according to the oxygen requirement as follows: Mild BPD- a need for supplemental oxygen (O2) for ≥28 days but not at 36 weeks’ postmenstrual age (PMA) or discharge; moderate BPD- a need for supplemental O2 for 28 days plus treatment with< 30% O2 at 36 weeks’ PMA; severe BPD- a need for supplemental O2 for ≥28 days plus ≥30% O2 and/or positive pressure at 36 weeks’ PMA [17]. Meanwhile, blood samples were collected from the radial artery for blood gas analysis before extubation, as well as 1, 6, 12, 24, 48, and 72 h after extubation.
Statistical analysis
Statistical data were analyzed by using Student’s t-test for parametric and the Mann–Whitney U test for non-parametric continuous variables; and χ2 test or Fisher’s exact test (if any expected value < 5 was found) for categorical variables. Repeated measurement data were used in the General Linear Model. Univariate and multivariate logistic regression was used to investigate risk factors of requiring MV within 72 h after extubation. The variables significant in univariate results would be entered into a multivariate model, and the variables significant in multivariate results would be considered as an independent factor associated with the primary outcome. The statistical significance level was set at a P-value < 0.05. All analyses were performed using IBM SPSS Version 20 (SPSS Statistics V20, IBM Corporation, Somers, New York).
Results
Patients’ demographic and clinical characteristics
A total of 184 preterm neonates with RDS were randomized into the lung recruitment group which received lung recruitment plus INSURE and the control group which received INSURE only (n = 92 for each group). Patients’ demographic and clinical characteristics were summarized in Table 1. Both the lung recruitment group and the control group had a mean gestational age of around 29.7 weeks and a mean birth weight of around 1.30 kg. There was no significant difference in infants at birth including gestational age, birth weight, gender, and rate of cesarean section (all P > 0.05). There was no significant difference in the mother’s mean age between the lung recruitment group and the control group (29.74 ± 5.19 vs. 30.71 ± 5.27 years, P = 0.211). The mothers of neonates in the control group had a higher incidence of gestational diabetes mellitus than those in the lung recruitment group (P = 0.005, Table 1).
Therapeutic outcomes and complications
Therapeutic outcomes were compared between the two groups. As shown in Table 2, the lung recruitment group had significantly fewer preterm neonates requiring MV within 72 h after extubation as compared with the control group (23% vs. 38%, P = 0.025). In addition, the MV duration, the averaging times of using pulmonary surfactant and the maximum FiO2 were significantly reduced in the lung recruitment group than in the control group (all P < 0.05, Table 2). Nevertheless, no other secondary outcomes were significantly different between the two groups (all P > 0.05, Table 2).
The 4 parameters of blood gas were compared between the two groups, including pH value (Fig. 2A), pCO2 (Fig. 2B), pO2 (Fig. 2C), and Base Excess (BE, Fig. 2D). No significant difference was observed between the two groups (P > 0.05).
As shown in Table 3, there was no significant difference in the incidences of complications between the lung recruitment and control groups (all P > 0.05), including BPD (33% vs. 40%), IVH (9% vs. 19%), pneumothorax (2% vs. 3%), NEC (11% vs. 16%), PDA (23% vs. 26%), ROP (21% vs. 15%), and PPHN (2% vs. 4%). Two cases (2%) in the lung recruitment group and 4 (4%) cases in the control group died because their parents gave up treatment due to financial considerations or possible serious complications (P = 0.4).
Independent factors associated with the need for MV within 72 h after extubation
To further investigate the risk factor of requiring MV within 72 h after extubation, univariate, and multivariate logistic regression models were performed. As shown in Table 4, the control group had a 2.17-time higher risk of requiring MV than the lung recruitment group (adjusted odds ratio [AOR]: 2.17, 95% CI: 1.13–4.18; P = 0.021). Compared with infants with a normotensive mother, infants with a hypertensive mother have a 2.41-time higher risk of requiring MV (AOR: 2.41, 95% CI: 1.15–5.05; P = 0.020).
Discussion
In this study, we compared the therapeutic efficacy of lung recruitment plus INSURE and INSURE alone for the preterm neonates with RDS. The results showed that compared to the control group, the lung recruitment group had a significantly lower proportion of preterm neonates requiring MV within 72 h after extubation (23% vs. 38%, P = 0.025) and pulmonary surfactant administration, as well as a shorter MV duration. Nevertheless, there were no significant differences in other secondary outcomes, 4 parameters of blood gas, and the incidence of complications between the two groups. Multivariate logistic regression analysis demonstrated that the control group had a 2.17-time higher risk of requiring MV than the lung recruitment group (AOR: 2.17, 95% CI: 1.13–4.18; P = 0.021). Compared with infants with a normotensive mother, infants with a hypertensive mother have a 2.41-time higher risk of requiring MV (AOR: 2.41, 95% CI: 1.15–5.05; P = 0.020).
Lista et al. conducted a clinical trial in which preterm infants with RDS treated with sustained lung inflation (25 cm H2O, sustained for 15 s) at birth and concluded that preterm infants with RDS received sustained lung inflation at birth may decrease the need for MV and did not induce adverse effects as compared with a historical control group [18]. Therefore, the condition of 25 cm H2O for 15 s was used in this study. Consistent with Lista et al.’s observation, our results suggested that lung recruitment can effectively reduce the need for MV but did not increase the adverse effects. In addition, both MV duration and the number of pulmonary surfactant administration were significantly reduced in the lung recruitment group as compared with the control group, which were in line with previous findings [11, 12, 18,19,20]. The lung recruitment technique might positively affect the clearance of lung fluid and allows a more even distribution of air throughout the lungs, thus facilitating the formation of FRC [21]. Therefore, the beneficial effects may be attributed to lung recruitment, subsequent FRC achievement and inflation-induced alveolar expansion.
BPD is a major complication of preterm birth [22] and has a complicated pathogenic mechanism. Immature lung development, acute lung injury, and abnormal repairment after injury are key points leading to BPD [23]. One of the most important pathogenic factors of BPD is ventilator-induced lung injury [24]. In this study, the incidence of BPD was lower in the lung recruitment group than in the control group (33% VS 40%), but the difference did not reach statistical significance. The incidence of different severe BPDs was also not significantly different between the two groups. This result suggested that lung recruitment did not increase the incidence of BPD. In this study, lung recruitment did not increase the incidences of adverse effects, including IVH, NEC, PDA, ROP, which is in agreement with previous studies [13, 14, 18, 25].
In this study, neonates of hypertensive mothers had a higher risk of the need for MV within 72 h after extubation than those of normotensive mothers. It has been shown that gestational hypertension can promote maternal production of soluble fms-like tyrosine kinase-1 (sFlt-1), an anti-angiogenic factor that can block vascular endothelial growth factor (VEGF) signaling [26, 27]. Since VEGF signaling is essential for the growth of pulmonary blood vessels and the production of surfactants, sFlt-1 may lead to increased incidence and severity of RDS in preterm neonates with hypertensive mothers. Lung recruitment seemed did not help these patients, and the underlying mechanism is needed to be further investigated.
In this study, two cases had pneumothorax in the lung recruitment group and three cases had pneumothorax in the control group, suggesting that lung recruitment did not increase the risk of pneumothorax. This result is consistent with previous reports [10, 14, 15, 25]. By contrast, Lista et al. have reported that patients with lung inflation treatment have a 4.57-time high risk of pneumothorax than the control patients [11]. The discrepancy might be attributed to different study subjects, and the effect of lung recruitment on pneumothorax should be further investigated.
In this study, no difference in mortality was found between the two groups. Two cases of death in the lung recruitment group because their parents gave up treatment rather than pneumothorax or other severe complications. This result suggested lung recruitment did not increase mortality. The comparison in the blood gas parameters between the two groups showed no significant difference, suggesting that lung recruitment did not impact the circulation and the rate of acidosis. This may be due to the comprehensive influence of ventilation improvement.
There are still some limitations to this study. First, the study was not a double-blind design. The staffs performing the study also cared for the infants later, which might affect the outcomes. We tried to minimize this bias by strictly following the trial protocol during the whole trial. In addition, this was a single-center trial and the sample size was still relatively small. In the future, a large multicenter trial should be conducted to validate the findings of this study.
Conclusion
Our study found that lung recruitment plus INSURE can effectively reduce the need for MV within 72 h after extubation and did not increase the incidence of complications and mortality.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- RDS:
-
Respiratory distress syndrome
- CPAP:
-
Continuous positive airway pressure
- MV:
-
Mandatory ventilation
- FRC:
-
Functional residual capacity
- IVH:
-
Intraventricular hemorrhage
- NEC:
-
Necrotizing enterocolitis
- ROP:
-
Retinopathy of prematurity
- PDA:
-
Patent ductus arteriosus
- PPHN:
-
Persistent pulmonary hypertension
- BPD:
-
Bronchopulmonary dysplasia
- PMA:
-
Postmenstrual age
References
Reuter S, Moser C, Baack M. Respiratory distress in the newborn. Pediatr Rev. 2014;35:417–29.
Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Te Pas A, et al. European consensus guidelines on the Management of Respiratory Distress Syndrome - 2019 update. Neonatology. 2019;115:432–50.
Sweet DG, Carnielli V, Greisen G, Hallman M, Ozek E, Plavka R, et al. European consensus guidelines on the Management of Respiratory Distress Syndrome - 2016 update. Neonatology. 2017;111:107–25.
Chen CM. Nasal CPAP or INSURE for RDS. Pediatr Neonatol. 2015;56:75–6.
Foglia EE, te Pas AB. Sustained lung inflation: physiology and practice. Clin Perinatol. 2016;43:633–46.
Lista G, La Verde PA, Castoldi F. Sustained inflation and its role in the delivery room Management of Preterm Infants. Neonatology. 2016;109:366–8.
Lista G, Maturana A, Moya FR. Achieving and maintaining lung volume in the preterm infant: from the first breath to the NICU. Eur J Pediatr. 2017;176:1287–93.
Te Pas AB, Siew M, Wallace MJ, Kitchen MJ, Fouras A, Lewis RA, et al. Establishing functional residual capacity at birth: the effect of sustained inflation and positive end-expiratory pressure in a preterm rabbit model. Pediatr Res. 2009;65:537–41.
Te Pas AB, Siew M, Wallace MJ, Kitchen MJ, Fouras A, Lewis RA, et al. Effect of sustained inflation length on establishing functional residual capacity at birth in ventilated premature rabbits. Pediatr Res. 2009;66:295–300.
Te Pas AB, Walther FJ. A randomized, controlled trial of delivery-room respiratory management in very preterm infants. Pediatrics. 2007;120:322–9.
Lista G, Boni L, Scopesi F, Mosca F, Trevisanuto D, Messner H, et al. Sustained lung inflation at birth for preterm infants: a randomized clinical trial. Pediatrics. 2015;135:e457–64.
El-Chimi MS, Awad HA, El-Gammasy TM, El-Farghali OG, Sallam MT, Shinkar DM. Sustained versus intermittent lung inflation for resuscitation of preterm infants: a randomized controlled trial. J Matern Neonatal Med. 2017;30:1273–8.
Jiravisitkul P, Rattanasiri S, Nuntnarumit P. Randomised controlled trial of sustained lung inflation for resuscitation of preterm infants in the delivery room. Resuscitation. 2017;111:68–73.
Harling AE, Beresford MW, Vince GS, Bates M, Yoxall CW. Does sustained lung inflation at resuscitation reduce lung injury in the preterm infant? Arch Dis Child Fetal Neonatal Ed. 2005;90:F406–10.
Bruschettini M, O’Donnell CP, Davis PG, Morley CJ, Moja L, Zappettini S, et al. Sustained versus standard inflations during neonatal resuscitation to prevent mortality and improve respiratory outcomes. Cochrane Database Syst Rev. 2017;7:CD004953.
Cole FS, Alleyne C, Barks JDE, Boyle RJ, Carroll JL, Dokken D, et al. NIH consensus development conference: inhaled nitric oxide therapy for premature infants. NIH Consens State Sci Statements. 2010;27:1–34.
Ehrenkranz RA, Walsh MC, Vohr BR, Jobe AH, Wright LL, Fanaroff AA, et al. Validation of the National Institutes of Health consensus definition of bronchopulmonary dysplasia. Pediatrics. 2005;116:1353–60.
Lista G, Fontana P, Castoldi F, Cavigioli F, Dani C. Does sustained lung inflation at birth improve outcome of preterm infants at risk for respiratory distress syndrome? Neonatology. 2011;99:45–50.
Buyuktiryaki M, Kanmaz HG, Okur N, Bezirganoglu H, Ozer Bekmez B, Simsek GK, et al. Sustained lung inflation at birth via short binasal prong in very low birth weight preterm infants: a retrospective study. Pediatr Pulmonol. 2018;53:1407–13.
Grasso C, Sciacca P, Giacchi V, Carpinato C, Mattia C, Palano GM, et al. Effects of sustained lung inflation, a lung recruitment maneuver in primary acute respiratory distress syndrome, in respiratory and cerebral outcomes in preterm infants. Early Hum Dev. 2015;91:71–5.
Vyas H, Milner AD, Hopkin IE, Boon AW. Physiologic responses to prolonged and slow-rise inflation in the resuscitation of the asphyxiated newborn infant. J Pediatr. 1981;99:635–9.
Michael Z, Spyropoulos F, Ghanta S, Christou H. Bronchopulmonary dysplasia: an update of current pharmacologic therapies and new approaches. Clin Med Insights Pediatr. 2018;12:1179556518817322.
Cutz E, Chiasson D. Chronic lung disease after premature birth. N Engl J Med. 2008;358:743–6.
Van Marter LJ, Allred EN, Pagano M, Sanocka U, Parad R, Moore M, et al. Do clinical markers of barotrauma and oxygen toxicity explain interhospital variation in rates of chronic lung disease? Pediatrics. 2000;105:1194–201.
Lindner W, Högel J, Pohlandt F. Sustained pressure - controlled inflation or intermittent mandatory ventilation in preterm infants in the delivery room? A randomized, controlled trial on initial respiratory support via nasopharyngeal tube. Acta Paediatr Int J Paediatr. 2005;94:303–9.
Wen YH, Yang HI, Chou HC, Chen CY, Hsieh WS, Tsou KI, et al. Association of Maternal Preeclampsia with neonatal respiratory distress syndrome in very-low-birth-weight infants. Sci Rep. 2019;9:13212.
Shin SH, Shin SH, Kim SH, Kim YJ, Cho H, Kim EK, et al. The Association of Pregnancy-induced Hypertension with bronchopulmonary dysplasia – a retrospective study based on the Korean neonatal network database. Sci Rep. 2020;10:5600.
Acknowledgements
None declared.
Funding
The study was supported by the Dongguan Social Science and Technology Development (Key) Project (201750715007468) in the aspect of study design and data analysis.
Author information
Authors and Affiliations
Contributions
We declare that all the listed authors have participated actively in the study and all meet the requirements of the authorship. Dr. LM designed the study and wrote the protocol, Drs. YW, RM and ZL acquired and collected the data, Dr. SJ and DH interpret the data and undertook the statistical analysis, Dr. YY wrote the first draft of the manuscript and mainly revised the manuscript. All authors approved the final version of this manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the institutional review board of Dongguan Maternal and Child Health Hospital [2016 [21]]. Written informed consent was obtained from the parents.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, Y., Yan, W., Ruan, M. et al. Lung recruitment improves the efficacy of intubation-surfactant-extubation treatment for respiratory distress syndrome in preterm neonates, a randomized controlled trial. BMC Pediatr 22, 14 (2022). https://doi.org/10.1186/s12887-021-03096-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-021-03096-y