Abstract
Background
Melnick-Needles syndrome (MNS) is an extremely rare osteochondrodysplasia caused by a mutation of FLNA, the gene encoding filamin A. MNS is inherited in an X-linked dominant manner. In this study, we describe three members of the same family with MNS, who exhibited different phenotypic severity despite having an identical FLNA gene mutation.
Case presentation
The patient was 16 months old, with a history of delayed physical development, multiple upper respiratory infections and otitis media episodes. She was referred to our orthopedic clinic because of bowed legs and an abnormal plain chest radiograph. Both upper and lower extremities were bowed. Plain X-rays showed thoracolumbar kyphoscoliosis, with anterior and posterior vertebral scalloping, and thin, wavy ribs. Hypoplasia of the pubis and ischium, with bilateral coxa valga, were also noted. Target exome sequencing revealed a heterozygous mutation of FLNA, c.3578 T > C, p.Lys1193Pro, which confirmed the diagnosis of MNS. Her older sister and mother had minimal deformities of the axial and extremity skeleton, but genetic analyses revealed the same FLNA mutation as the patient. The mutation identified in this family has not been previously reported.
Conclusion
This report illustrates the potential inherited nature of MNS and the phenotypic variability of clinicoradiologic characteristics. In patients with traits suggestive of MNS, a careful medical and family history should be obtained, and genetic testing should be performed for the patient, as well as all family members.
Similar content being viewed by others
Background
Melnick-Needles syndrome (MNS, OMIM: #309350) is an extremely rare osteochondrodysplasia [1,2,3]. To date, less than 70 cases of MNS have been reported worldwide [4]. MNS is caused by gain-of-function mutations in the FLNA gene (OMIM: #30017) which encodes filamin A. Patients with MNS typically have unusual facial features, short ribbon-like ribs, scoliosis, bowing of the long bones, and vertebral scalloping [5]. Intelligence is not impaired. In more severe cases, affected individuals die in the second or third decade of life from respiratory failure secondary to the chest wall abnormalities [4].
MNS is a member of a group of five X-linked diseases with overlapping clinical phenotypes, known collectively as otopalatodigital syndrome (OPS) spectrum disorders [6]. Other members of the group are OPS type 1 (OMIM: #311300), OPS type 2 (OMIM: #304120), frontometaphyseal dysplasia (FMD, OMIM: #305620), and terminal osseous dysplasia with/without pigmentary defects (TODPD, OMIM: #300244). MNS is found almost exclusively in females, as the syndrome is lethal during gestation or the perinatal period in almost all affected males [7]. In males that do survive to term, the phenotype is clinically indistinguishable from that of OPS type 2 [8]. Females with MNS have characteristic clinical and radiologic diagnostic findings. Table 1 shows details of the clinical features of patients with MNS reported in the past 15 years [9,10,11,12,13,14].
Because MNS is extremely rare and some cases are lethal, mostly it is detected as de novo condition, but once it is developed, it is inherited in an X-linked dominant manner [15, 16]. However, previous reports did not describe the familial characteristics of the disease in detail. In this case report, we describe a family with MNS who exhibited variable severity of phenotypic changes despite having an identical FLNA gene mutation.
Case presentation
A 16-month-old female was referred to our orthopedic department because of bowed legs and an abnormal chest X-ray. She was 80 cm (50th percentile) tall and weighed 9.7 kg (25th percentile). Her past medical history was positive for delayed physical development, as well as recurrent respiratory tract infections and episodes of otitis media. Examination revealed several facial characteristics of MNS, including prominent eyes, supraorbital hyperostosis, full cheeks, and micrognathia (Fig. 1). Plain radiographs revealed a number of abnormalities.
X-ray showed thoracolumbar kyphoscoliosis and anterior and posterior vertebral scalloping; humerus cortical irregularity with bowing; thin wavy ribs; pelvis hypoplasia of the pubis and ischium and bilateral coxa valga; bilateral bowed leg deformities, with normal epiphyses and metaphyses. The bone age estimated from X-rays of the hand was 1.5 years, which was similar with the patient’s chronological age (Fig. 2).
Plain radiographs of the patient at age 16 months. Overall, the patient’s bones were curved and thin. Bone age was not delayed, but her bones did not have normal alignment or cortical bone maturity and showed osteodysplasia. a, b, red arrow The patient had a thoracolumbar kyphoscoliosis with a humeral cortical irregularity and thin, wavy ribs. c, red circle Bilateral bowed leg deformities with Erlenmeyer flask deformity were observed. d, e The pubis and ischium were hypoplastic, and coxa valga was present bilaterally. f The ulna and radius were curved. g Bone age was normal, according to the hand radiographs
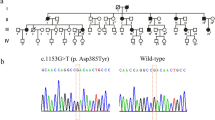
To confirm the clinical impression of MNS, we performed genetic analyses. Target exome sequencing revealed a heterozygous mutation in the FLNA gene, c.3578 T > C, p.L1193P, which confirmed the diagnosis. Subsequently, the patient continued to have repeated respiratory tract infections and otitis media episodes. She died at the age of 6 years of a cardiac arrest, the direct cause of which was undetermined.
Target exome sequencing was also performed for all available family members. Her mother and older sister were found to have the exact same mutation, although they exhibited less severe MNS phenotypes. Her mother had full cheeks (like the patient) and lumbar scoliosis, but she had minimal leg deformities (Fig. 3). Her older sister had essentially no MNS facial characteristics, but she did exhibit coxa valga deformities (Fig. 4). When initially assessed, the sister’s spinal alignment was normal, but thoracolumbar kyphoscoliosis was observed at 9 years of age.
Photographs and plain radiographs of the patient’s mother. Overall, the patient’s mother had relatively mild deformities, when compared with the patient. a, b Like the patient, she had full cheeks and micrognathia,which were mild. c, d, e She also had mild lumbar scoliosis, kyphosis, and minimally bowed legs bilaterally
Photographs and plain radiographs of the patient’s older sister. a, b The patient’s older sister had a nearly normal-appearing face. c, d At 6 years of age, plain radiographs revealed normal spine alignment. e However, bilateral coxa valga and Erlenmeyer flask deformities were noted at 6 years of age. f, g At age 9 years, thoracolumbar kyphoscoliosis was apparent. h The coxa valga and Erlenmeyer flask deformities were still present
Discussion and conclusions
The locus associated with MNS is the FLNA gene, which encodes the cytoskeletal protein filamin A. FLNA comprises 48 exons and encodes a modular protein with an N-terminal actin-binding domain and a tail of 24 structurally homologous repeats [4]. Cellular functions mediated by filamin include linking signal transduction events to modulation of the actin cytoskeleton and gene transcription [17]. In 2003, Robertson et al. reported that MNS is caused by gain-of-function mutations in the FLNA gene and has an X-linked pattern of inheritance. They also noted that FLNA mutations are responsible for OPS type 1, OPS type 2, FMD, and TODPD (Table 2) [6, 12, 18].
The pathogenesis of MNS has not been established. Some researchers have reported increased skeletal collagen content, which could explain the sclerosing bone process [9]. Fryns et al. suggested that MNS was a generalized connective tissue disorder because of the hyperlaxity of skin and joints [19]. Urological, pulmonary, and cardiac involvement is also common in patients with MNS [20, 21]. Although diverse phenotypes may occur [22], affected females are usually short and may have delayed motor development, osteoarthritis, a hoarse voice, and urethral stenosis (leading to hydronephrosis), in addition to the main abnormalities [1].
It is not yet known why phenotypes may differ between females with MNS. Skewed X-inactivation and somatic mutation have been suggested as potential mechanisms [23, 24]. For example, Robertson et al. reported monozygotic twin sisters, only one of whom had MNS [24]. In our case, although phenotypic severity differed between female family members, they all had the same heterozygous FLNA mutation (c.3578 T > C, p.L1193P). Interestingly, the mutations identified in this family have not been previously reported in the National Center for Biotechnology Information’s ClinVar. As mentioned earlier, pathogenesis of MNS has not been established well. Further research is also needed to determine pathogenicity of this mutation among these families with MNS.
It should be noted that the patient with MNS would demonstrate the typical bone deformity in the distal femur, which was called as the Erlenmeyer flask deformity like Camurati-Engelmann disease (CED, OMIM: #131300). CED is another rare genetic skeletal disorder caused by tumor growth factor-β1 mutation, which is characterized by limb pain, muscle emaciation and weakness, cortical thickening of the diaphysis of long bones, and also Erlenmeyer flask deformity [25, 26].
Although MNS is rare, physicians should be aware of the disorder, including its variable manifestations, because of the potential lethality of severe disease. A possible hereditary mutation should be suspected even when family members have an almost normal appearance. Thus, in patients exhibiting traits suggestive of MNS, imaging studies and genetic testing should be performed for both the patient and all family members.
Informed consent statement
Informed written consent was obtained. It contains publication of this report and the accompanying images, including photographic rights of patient, her mother and her sister (Use of medical information for academic purposes, including the portrait rights shown in Figs. 1, 3 and 4). For the patient, her mother and her sister, written consent was obtained from the father and mother for all teaching and academic purposes, including publication of this case report.
Availability of data and materials
The datasets used and/or analyzed during the current report are available from the corresponding author on reasonable request.
Abbreviations
- MNS:
-
Melnick-Needles syndrome
- OPS:
-
Otopalatodigital syndrome
- FMD:
-
Frontometaphyseal dysplasia
- TODPD:
-
Terminal osseous dysplasia with/without pigmentary defects
- CED:
-
Camurati-Engelmann disease
References
Santos HH, Garcia PP, Pereira L, Leao LL, Aguiar RA, Lana AM, Carvalho MR, Aguiar MJ. Mutational analysis of two boys with the severe perinatally lethal Melnick-Needles syndrome. Am J Med Genet Part A. 2010;152a(3):726–31.
Coste F, Maroteaux P, Chouraki L. Osteodysplasty (Melnick and Needles syndrome). Report of a case. Ann Rheum Dis. 1968;27(4):360–6.
Melnick JC, Needles CF. An undiagnosed bone dysplasia. A 2 family study of 4 generations and 3 generations. Am J Roentgenol Radium Therapy, Nucl Med. 1966;97(1):39–48.
Bandyopadhyay SK, Ghosal J, Chakrabarti N, Dutta A. Melnick- needles osteodysplasty presenting with quadriparesis. J Assoc Physicians India. 2006;54:248–9.
Unal VS, Derici O, Oken F, Turan S, Girgin O. Fibular lengthening procedure: treatment for lateral instability of the ankle caused by fibular insufficiency in Melnick-Needles syndrome. J Pediatr Orthop B. 2004;13(2):88–91.
Robertson SP. Otopalatodigital syndrome spectrum disorders: otopalatodigital syndrome types 1 and 2, frontometaphyseal dysplasia and Melnick-Needles syndrome. Eur J Hum Genet. 2007;15(1):3–9.
Donnenfeld AE, Conard KA, Roberts NS, Borns PF, Zackai EH. Melnick-Needles syndrome in males: a lethal multiple congenital anomalies syndrome. Am J Med Genet. 1987;27(1):159–73.
Robertson S, Gunn T, Allen B, Chapman C, Becroft D. Are Melnick-Needles syndrome and Oto-palato-digital syndrome type II allelic? Observations in a four-generation kindred. Am J Med Genet. 1997;71(3):341–7.
Svejcar J. Biochemical abnormalities in connective tissue of osteodysplasty of Melnick-Needles and dyssegmental dwarfism. Clin Genet. 1983;23(5):369–75.
Lykissas MG, Crawford AH, Shufflebarger HL, Gaines S, Permal V. Correction of spine deformity in patients with Melnick-needles syndrome: report of 2 cases and literature review. J Pediatr Orthop. 2013;33(2):170–4.
Harper D, Bloom DA, Rowley JA, Soubani A, Smith WL. The high-resolution chest CT findings in an adult with Melnick-Needles syndrome. Clin Imaging. 2006;30(5):350–3.
Albuquerque do Nascimento LL, Salgueiro Mda C, Quintela M, Teixeira VP, Mota AC, de Godoy CH, Bussadori SK. Maxillofacial Changes in Melnick-Needles Syndrome. Case Rep Dent. 2016;2016:9685429..
O'Connell JE, Bourke B, Kearns GJ. Orthognathic surgery in Melnick-Needles syndrome: a review of the literature and report of two siblings. Int J Oral Maxillofac Surg. 2018;47(6):738–42.
Jung S, Wermker K, Joos U, Kleinheinz J. Orthognathic surgery in Melnick-Needles-syndrome. Case report and review of the literature. Int J Oral Maxillofac Surg. 2012;41(3):309–12.
Kustrzycka D, Mikulewicz M, Pelc A, Kosior P, Dobrzyński M. Craniofacial and dental manifestations of Melnick–Needles syndrome: literature review and orthodontic management. Case Rep Pediatr. 2018;2018:5891024.
Foley C, Roberts K, Tchrakian N, Morgan T, Fryer A, Robertson S, Tubridy N. Expansion of the Spectrum of FLNA mutations associated with Melnick-Needles syndrome. Mole Syndromol. 2010;1(3):121–6.
Stossel TP, Condeelis J, Cooley L, Hartwig JH, Noegel A, Schleicher M, Shapiro SS. Filamins as integrators of cell mechanics and signalling. Nat Rev Mol Cell Biol. 2001;2(2):138–45.
Robertson S. Otopalatodigital spectrum disorders. In: GeneReviews®. Seattle: University of Washington; 2013.
Fryns J, Schinzel A, Van den Berghe H. Reynolds JFJAjomg: Hyperlaxity in males with Melnick-Needles syndrome. Am J Med Genet. 1988;29(3):607–11.
Klint RB, Agustsson MH, McAlister WH. Melnick-Needles osteodysplasia associated with pulmonary hypertension, obstructive uropathy and marrow hypoplasia. Pediatr Radiol. 1977;6(1):49–51.
LaMontagne AE. Urological manifestations of the Melnick-Needles syndrome: a case report and review of the literature. J Urol. 1991;145(5):1020–1.
Akin L, Adal E, Akin MA, Kurtoglu S. Melnick-Needles syndrome associated with growth hormone deficiency: a case report. J Clin Res Pediatr Endocrinol. 2009;1(5):248–51.
Kristiansen M, Knudsen GP, Soyland A, Westvik J, Orstavik KH. Phenotypic variation in Melnick-Needles syndrome is not reflected in X inactivation patterns from blood or buccal smear. Am J Med Genet. 2002;108(2):120–7.
Robertson SP, Thompson S, Morgan T, Holder-Espinasse M, Martinot-Duquenoy V, Wilkie AO, Manouvrier-Hanu S. Postzygotic mutation and germline mosaicism in the otopalatodigital syndrome spectrum disorders. Eur J Hum Genet. 2006;14(5):549–54.
Faden MA, Krakow D, Ezgu F, Rimoin DL, Lachman RS. The Erlenmeyer flask bone deformity in the skeletal Dysplasias. Am J Med Genet A. 2009;149A(6):1334–45.
Yuldashev AJ, Shin CH, Kim YS, Jang WY, Park MS, Chae JH, Yoo WJ, Choi IH, Kim OH, Cho TJ. Orthopedic manifestations of type I Camurati-Engelmann disease. Clin Orthop Surg. 2017;9(1):109–15.
Acknowledgements
We thank Drs. Tae Joon Cho and Ok Hwa Kim for assisting with the data analysis and image interpretation.
Funding
This research was supported by the Bio & Medical Technology Development Program of the National Research Foundation (NRF) funded by the Ministry of Science & ICT (number 2016M3A9E8941667). This work was also supported by an NRF grant funded by the Korea government (MSIT) (number 2019R1C1C1004017). These sponsors did not participate in determining the study design or in analyzing or interpreting the data. They also did not contribute to writing the report.
Author information
Authors and Affiliations
Contributions
CHO contributed to the conception and design of the study, as well as the manuscript writing. CHL contributed to the conception and design of the study and interpreted the otorhinolaryngological findings. SYK contributed to writing the manuscript. SYL reviewed the literature and drafted the manuscript. HHJ reviewed the literature and drafted the manuscript. SL contributed to the conception and design of the study, analyzing the data, interpreting the imaging findings, writing the manuscript, and preparing and submitting the final manuscript. All authors have read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the CHA Bundang Medical Center institutional review board (number 2018–01-042).
Consent for publication
Written informed consent was obtained for publication of this case report and all accompanying images. A copy of the written consent is available for review. In this study, we received a consent form to provide medical information, including photographic rights from parents of the patient. These procedures were approved by our institutional review board.
Competing interests
The authors declare no competing interests. They have no potential, perceived, or real conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Oh, C.H., Lee, C.H., Kim, S.Y. et al. A family of Melnick-Needles syndrome: a case report. BMC Pediatr 20, 391 (2020). https://doi.org/10.1186/s12887-020-02288-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-020-02288-2