Abstract
Background
The optimal treatment strategy for resectable BRAF V600E mutant colorectal oligometastases (CRM) has not been established due to the rarity and rapid progression of the disease. Since the unresectable recurrence rate is high, development of novel perioperative therapies are warranted. On December 2020, the BEACON CRC triplet regimen of encorafenib, binimetinib, and cetuximab was approved for unresectable metastatic colorectal cancer in Japan.
Methods
The NEXUS trial is a multicenter phase II clinical study evaluating the efficacy and safety of the perioperative use of encorafenib, binimetinib, and cetuximab in patients with previously untreated surgically resectable BRAF V600E mutant CRM. The key inclusion criteria are as follows: histologically diagnosed with colorectal adeno/adenosquamous carcinoma; RAS wild-type and BRAF V600E mutation by tissue or blood; and previously untreated resectable distant metastases. The triplet regimen (encorafenib: 300 mg daily; binimetinib: 45 mg twice daily; cetuximab: 400 mg/m2, then 250 mg/m2 weekly, 28 days/cycle) is administered for 3 cycles each before and after curative resection. The primary endpoint of the study is the 1-year progression-free survival (PFS) rate and the secondary end points are the PFS, disease-free survival, overall survival, and objective response rate. The sample size is 32 patients. Endpoints in the NEXUS trial as well as integrated analysis with the nationwide registry data will be considered for seeking regulatory approval for the perioperative use of the triplet regimen.
Discussion
The use of the triplet regimen in the perioperative period is expected to be safe and effective in patients with resectable BRAF V600E mutant CRM.
Trial registration
jRCT2031220025, April. 16, 2022.
Similar content being viewed by others
Backgrounds
BRAF is a serine/threonine kinase that belongs to the RAF family that was first reported in the early 2000s [1, 2]. It is downstream of RAS in the MAPK signaling pathway, which is involved in the regulation of cellular functions, including cell proliferation. Among the BRAF mutations, V600E mutation can enhance BRAF kinase activity up to 700-fold of that of the wild-type. BRAF V600E mutant metastatic colorectal cancer (mCRC) accounts for 5%–10% of all cases of mCRC and exhibits distinct clinicopathologic features, including a propensity for the right side of the colon, poor histological differentiation, peritoneal dissemination, and high microsatellite instability [3]. Prognosis of unresectable BRAF V600E mutant mCRC is poor compared with that of RAS-mutant and RAS/BRAF wild-type; the median overall survival (OS) is 9.2–14.1 months [4,5,6,7].
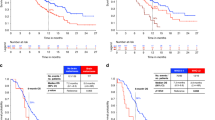
Recently, the BEACON CRC trial, which enrolled patients with previously treated unresectable BRAF V600E mutant mCRC, demonstrated that the triplet regimen of encorafenib (a BRAF inhibitor), binimetinib (an MEK inhibitor), and cetuximab (anti-EGFR antibody) as well as the doublet regimen of encorafenib and cetuximab significantly improved both progression-free survival (PFS) and OS compared with standard chemotherapy (FOLFIRI/irinotecan plus cetuximab) [8, 9]. While the hazard ratios (HR) of the triplet regimen and control groups for PFS and OS were 0.42 (95% CI: 0.33–0.53) and 0.60 (95% CI: 0.47–0.75) (P < 0.001), respectively, those of the doublet regimen and control groups were 0.44 (95% CI: 0.35–0.55) and 0.61 (95% CI: 0.48–0.77). As the triplet regimen did not exhibit significant survival benefits over the doublet regimen (HR: 0.95, 95% CI: 0.74 – 1.21), the doublet combination has become the standard second-line treatment in the United States and European Union. However, the confirmed objective response rate (ORR) was 26.8% for the triplet regimen and 19.5% for the doublet regimen, and the triplet regimen was potentially more effective than the doublet regimen in patients with remaining primary lesions, ≥ 3 organs involved, and high C-reactive protein levels, i.e., those with a greater tumor load. Moreover, the triplet regimen achieved a deeper response than the doublet regimen (p = 0.033). Therefore, both the triplet and doublet regimens have been approved for use in Japan.
The BEACON CRC trial was followed by the ANCHOR CRC trial wherein the effectiveness of the triplet regimen was evaluated in patients with previously untreated unresectable BRAF V600E mutant mCRC. The ORR of the triplet regimen was 47.8% in the ANCHOR CRC trial, which was better than that in the BEACON CRC trial [10]. The efficacy and safety of the doublet regimen are being evaluated in the randomized phase III BREAKWATER trial (NCT04607421), which aims to compare the efficacy of doublet regimen with or without chemotherapy (FOLFOX) with the standard chemotherapy alone (FOLFOX/FOLFOXIRI/CAPOX with or without bevacizumab), in patients with previously untreated unresectable BRAF V600E mutant mCRC [11, 12].
The optimal treatment strategy for resectable BRAF V600E mutant mCRC has not been established due to the rarity (approximately 3%) and rapid progression of the disease [13,14,15,16]. Margonis et al. reported that the median disease-free survival (DFS) and OS after hepatectomy for BRAF V600E mutant colorectal liver metastases were 9.9 and 26 months, respectively [14]. We also reported that 93.9% of patients who underwent hepatectomy for BRAF V600E mutant colorectal liver metastases developed recurrence after a median 5.3 months, and their median OS was 31.1 months [16]. Since the rate of early onset unresectable systemic recurrence was high, we advocated the necessity of developing novel perioperative therapies [17, 18]. Considering that more than 60% of resectable BRAF V600E mutant colorectal liver metastases are metachronous within 1 year after the resection of primary CRC for which patients have mostly received adjuvant oxaliplatin-based chemotherapy [16], the BEACON regimen is considered the optimal regimen of choice for perioperative use. Additionally, the BEACON triplet regimen may even be more preferable to the doublet regimen because 40% of resectable BRAF V600E mutant mCRC is synchronous with the primary CRC and often involves three organs (i.e., liver, lung, and primary CRC) [16], hence the preference for the triplet regimen [9]. Moreover, the deeper response that was offered by the triplet regimen justifies its perioperative use, especially in the neoadjuvant setting.
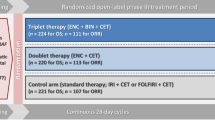
Accordingly, we planned a multicenter phase II clinical study to evaluate the efficacy and safety of the perioperative use of encorafenib, binimetinib, and cetuximab in patients with previously untreated but surgically resectable BRAF V600E mutant colorectal oligometastases (CRM) (NEXUS trial, jRCT2031220025) (Fig. 1) [19]. Because surgically resectable BRAF V600E mutant mCRC is rarer than the unresectable subtype, a randomized trial for this disease is difficult to conduct. In a phase II TRIUMPH study (UMIN000027887), the efficacy and safety of pertuzumab plus trastuzumab were evaluated in patients with previously treated unresectable HER2-positive mCRC [20]. For regulatory approval, we utilized real-world data (RWD) in the regulatory-graded registry (SCRUM-Japan Registry) as an external control [21, 22]. Similarly, a regulatory-graded nationwide clinico-patho-genomic registry of patients scheduled for surgery for resectable CRC was recently established in Japan (GALAXY trial, UMIN000039205) [23, 24]. Therefore, we planned to compare the efficacy and safety of the perioperative use of the triplet regimen with those of the RWD extracted from the registry as an external control.
Methods/Design
Patient screening
Patients with resectable CRM at institutions participating in the NEXUS trial were screened for BRAF V600E by screening their tissue or blood sample using comprehensive genotyping assay using Guardant360 (Guardant Health, Inc., Redwood City, CA, USA) to detect circulating tumor DNA (ctDNA) (PRECISION study, UMIN000042490) [25]. Aside from the institutions participating in the NEXUS trial, more than 140 institutions all over Japan that participated in the GALAXY trial were encouraged to refer eligible patients with BRAF V600E mutant CRM to institutions participating in the NEXUS trial.
Study design and treatment
The NEXUS trial is a multicenter phase II clinical study that will evaluate the efficacy and safety of the perioperative use of encorafenib, binimetinib, and cetuximab (the BEACON triplet regimen) in patients with previously untreated but surgically resectable BRAF V600E mutant CRM. Table 1 shows the eligibility criteria. The key inclusion criteria are as follows: age ≥ 20 years; Eastern Cooperative Oncology Group Performance Status 0 or 1; histologically diagnosed with primary adenocarcinoma or adenosquamous carcinoma of the colon or rectum; RAS (KRAS/NRAS) wild-type and BRAF V600E mutation upon analysis of tumor tissues or blood specimens; and previously untreated distant metastasis for which macroscopic complete resection (R0/1 resection according to the Japanese guidelines for the treatment of CRC [26]) is possible. Patients in whom R0/1 resection is impossible unless tumor shrinkage or elimination is achieved by chemotherapy were excluded. The triplet regimen (encorafenib: 300 mg daily, binimetinib: 45 mg twice daily, cetuximab: 400 mg/m2 of body-surface area as an initial dose, then 250 mg/m2 weekly, 28 days in a cycle), [8] as described in the BEACON CRC trial, is offered for 3 cycles each before and after curative resection.
Endpoints
The primary endpoint is the 1-year PFS rate, and the secondary endpoints are the PFS, DFS, OS, 1-year PFS rate by central image review, ORR, pathological complete response (CR) rate of distant metastatic lesions and the primary lesion as assessed by pathologists at each institution, protocol treatment completion rate, R0 resection rate, incidence of adverse events, and incidence of surgery-related complications. An exploratory endpoint is the analysis of biomarkers related to the efficacy and toxicity of the protocol treatment. Progression is defined as either progressive disease based on diagnostic imaging in the assessment of overall response according to the revised guidelines on the Response Evaluation Criteria in Solid Tumors version 1.1 [27] during the neoadjuvant treatment, macroscopically incomplete resection (R2 resection), recurrence after surgical resection, or death. The 1-year PFS rate is defined as the proportion of patients who developed progression at the 1-year time point as measured from the date of registration.
Sample size and statistical analysis
As the 1-year DFS in patients with BRAF V600E mutant colorectal liver metastases is 24% in Japan, and the HR of triplet therapy for PFS in the final report of the BEACON CRC trial is 0.42 [9, 16], 25% and 50% were set as the threshold and expected values, respectively, for the 1-year PFS rate in this study. Planned patient accrual was set at 32 patients, with the one-sided significance level at 2.5% and statistical power at 80%.
Translational analysis
Multi-omics analysis of both tumor tissues and blood specimens at enrollment, resection, and relapse will be performed to investigate the prognostic factors (MONSTAR-2 study, UMIN000043899) [28]. ctDNA is analyzed before surgery and at 4, 12, 24, 36, 48, 72, and 96 weeks postoperatively to evaluate the value of molecular residual disease using a personalized tumor-informed ctDNA assay, Signatera (Natera, Inc., San Carlos, CA, USA) in this disease setting [23].
Planned regulatory approval
Since the NEXUS trial is a single-arm study, the efficacy and safety data will be compared with those of the RWD in the registry, wherein treatments other than this protocol treatment were administered to the same subjects. PFS, DFS, OS, and incidence of surgery-related complications in the NEXUS trial will be compared with those extracted from the regulatory-graded prospective large-scale nationwide clinico-patho-genomic registry (GALAXY trial) [23, 24]. Endpoints in the NEXUS trial as well as integrated analysis with the registry data will be considered for regulatory approval to expand the indications of the BEACON triplet regimen, including its perioperative use.
Discussion
Since the discovery of the notorious BRAF V600E mutation, many attempts have been made to improve the prognosis of patient with CRC with the said mutation. As its prognosis is, by far, worse in patients with unresectable metastatic disease than in those with locally limited resectable ones, clinical trials focusing on BRAF V600E CRC have been conducted for unresectable metastatic disease. However, because most cases of metastatic disease are found with unresectable tumors, no prospective clinical trials have been conducted for metastatic and resectable cases. To the best of our knowledge, the NEXUS trial is the first and the only trial to investigate the efficacy of perioperative targeted therapy for resectable BRAF V600E mutant CRM.
While survival outcomes of patients with surgically resected BRAF V600E mutant CRM are better than those in medically treated patients [29, 30], upfront resection of resectable BRAF V600E mutant CRM also has a poor prognosis [16, 18]. Patients with BRAF V600E mutant liver metastases developed early systemic and unresectable recurrences within 8 months after surgery, and the OS was almost identical to that after systemic chemotherapy for unresectable cases. Moreover, since BRAF V600E mutant mCRC is a rapidly progressive disease and that causes rapid deterioration of performance status with early relapse after surgery, 20% of patients who underwent upfront hepatectomy could not receive chemotherapy after recurrence. Therefore, the use of neoadjuvant chemotherapy is warranted in this patient cohort [17, 31]. Perioperative chemotherapy might be effective to control micro-metastatic lesions. Amaria et al. conducted a randomized phase II study comparing perioperative doublet therapy with dabrafenib (a BRAF inhibitor) and trametinib (an MEK inhibitor) and surgery followed by adjuvant therapy in patients with stage III or resectable stage IV malignant melanoma with BRAF V600E/K mutation [32]. The study was terminated when statistical evidence of the efficacy was demonstrated in only 21 patients, with the DFS being 19.7 months and 2.9 months for the perioperative doublet therapy and surgery-first groups, respectively (HR: 0.016; 95% CI: 0.00012–0.14). Therefore, the efficacy and safety of the perioperative use of the BEACON regimen are expected in patients with resectable BRAF V600E mutant CRM.
Although two decades have passed since the detrimental impact of BRAF V600E on mCRC was first reported in the early 2000s [1, 2], poor survival outcomes of resectable BRAF V600E mutant CRM has not been resolved, much like two-decades long arduous journey of Odysseus depicted in the Odyssey. We believe that the NEXUS trial is a crucial step in developing an effective and safe treatment for resectable BRAF V600E mutant CRM, which will eventually help end the odyssey.
Availability of data and materials
Data sharing is not applicable to this paper.
Abbreviations
- CRM:
-
Colorectal oligometastases
- CR:
-
Complete response
- ctDNA:
-
Circulating tumor DNA
- DFS:
-
Disease-free survival
- PFS:
-
Progression-free survival
- OS:
-
Overall survival
- ORR:
-
Objective response rate
- HR:
-
Hazard ratio
- mCRC:
-
Metastatic colorectal cancer
References
Davies H, Bignell GR, Cox C, Stephens P, Edkins S, Clegg S, Teague J, Woffendin H, Garnett MJ, Bottomley W, et al. Mutations of the BRAF gene in human cancer. Nature. 2002;417:949–54.
Wan PT, Garnett MJ, Roe SM, Lee S, Niculescu-Duvaz D, Good VM, Jones CM, Marshall CJ, Springer CJ, Barford D, Marais R. Mechanism of activation of the RAF-ERK signaling pathway by oncogenic mutations of B-RAF. Cell. 2004;116:855–67.
Hall RD, Kudchadkar RR. BRAF mutations: signaling, epidemiology, and clinical experience in multiple malignancies. Cancer Control. 2014;21:221–30.
Douillard J-Y, Oliner KS, Siena S, Tabernero J, Burkes R, Barugel M, Humblet Y, Bodoky G, Cunningham D, Jassem J, et al. Panitumumab–FOLFOX4 Treatment and <i>RAS</i> Mutations in Colorectal Cancer. N Engl J Med. 2013;369:1023–34.
Modest DP, Ricard I, Heinemann V, Hegewisch-Becker S, Schmiegel W, Porschen R, Stintzing S, Graeven U, Arnold D, von Weikersthal LF, et al. Outcome according to KRAS-, NRAS- and BRAF-mutation as well as KRAS mutation variants: pooled analysis of five randomized trials in metastatic colorectal cancer by the AIO colorectal cancer study group. Ann Oncol. 2016;27:1746–53.
Stintzing S, Miller-Phillips L, Modest DP, von Fischer Weikersthal L, Decker T, Kiani A, Vehling-Kaiser U, Al-Batran SE, Heintges T, Kahl C, et al. Impact of BRAF and RAS mutations on first-line efficacy of FOLFIRI plus cetuximab versus FOLFIRI plus bevacizumab: analysis of the FIRE-3 (AIO KRK-0306) study. Eur J Cancer. 2017;79:50–60.
Bokemeyer C, Cutsem EV, Rougier P, Ciardiello F, Heeger S, Schlichting M, Celik I, Köhne C-H. Addition of cetuximab to chemotherapy as first-line treatment for KRAS wild-type metastatic colorectal cancer: Pooled analysis of the CRYSTAL and OPUS randomised clinical trials. Eur J Cancer. 2012;48:1466–75.
Kopetz S, Grothey A, Yaeger R, Van Cutsem E, Desai J, Yoshino T, Wasan H, Ciardiello F, Loupakis F, Hong YS, et al. Encorafenib, Binimetinib, and Cetuximab in BRAF V600E-Mutated Colorectal Cancer. N Engl J Med. 2019;381:1632–43.
Tabernero J, Grothey A, Van Cutsem E, Yaeger R, Wasan H, Yoshino T, Desai J, Ciardiello F, Loupakis F, Hong YS, et al. Encorafenib Plus Cetuximab as a new standard of care for previously treated BRAF V600E-mutant metastatic colorectal cancer: updated survival results and subgroup analyses from the BEACON Study. J Clin Oncol. 2021;39:273–84.
Van Cutsem E, Taieb J, Yaeger R, Yoshino T, Maiello E, Elez E, Dekervel J, Ross P, Ruiz Casado A, Graham J, et al. O-10 ANCHOR CRC: results from a single-arm, phase 2 study of encorafenib, binimetinib plus cetuximab in previously untreated BRAF V600E–mutant metastatic colorectal cancer. Ann Oncol. 2021;32:S222.
BRAF V600E-mutant Colorectal Cancer Study of Encorafenib Taken With Cetuximab Plus or Minus Chemotherapy (BREAKWATER) [https://clinicaltrials.gov/ct2/show/NCT04607421].
Kopetz S, Yoshino T, Kim TW, Desai J, Yaeger R, Cutsem EV, Ciardiello F, Wasan HS, Maughan T, Zhang Y, et al. BREAKWATER safety lead-in (SLI): Encorafenib + cetuximab (EC) ± chemotherapy for first-line (1L) treatment (tx) of BRAF V600E-mutant (BRAFV600E) metastatic colorectal cancer (mCRC). J Clin Oncol. 2022;40:134–134.
Gagniere J, Dupre A, Gholami SS, Pezet D, Boerner T, Gonen M, Kingham TP, Allen PJ, Balachandran VP, De Matteo RP, et al. Is Hepatectomy justified for BRAF mutant colorectal liver metastases?: A multi-institutional analysis of 1497 patients. Ann Surg. 2020;271:147–54.
Margonis GA, Buettner S, Andreatos N, Kim Y, Wagner D, Sasaki K, Beer A, Schwarz C, Loes IM, Smolle M, et al. Association of BRAF mutations with survival and recurrence in surgically treated patients with metastatic colorectal liver cancer. JAMA Surg. 2018;153:e180996.
Schirripa M, Bergamo F, Cremolini C, Casagrande M, Lonardi S, Aprile G, Yang D, Marmorino F, Pasquini G, Sensi E, et al. BRAF and RAS mutations as prognostic factors in metastatic colorectal cancer patients undergoing liver resection. Br J Cancer. 2015;112:1921–8.
Kobayashi S, Takahashi S, Takahashi N, Masuishi T, Shoji H, Shinozaki E, Yamaguchi T, Kojima M, Gotohda N, Nomura S, et al. Survival outcomes of resected BRAF V600E mutant colorectal liver metastases: a multicenter retrospective cohort study in Japan. Ann Surg Oncol. 2020;27:3307–15.
Kobayashi S, Takahashi S, Yoshino T, Taniguchi H. ASO author reflections: the moment that BRAF V600E mutation starts evolving into “Precision Oncosurgery” in colorectal liver metastases. Ann Surg Oncol. 2020;27:3316–7.
Kobayashi S, Takahashi S, Nomura S, Kojima M, Kudo M, Sugimoto M, Konishi M, Gotohda N, Taniguchi H, Yoshino T. BRAF V600E potentially determines “Oncological Resectability” for “Technically Resectable” colorectal liver metastases. Cancer Med. 2021;10:6998–7011.
Neoadjuvant and adjuvant chemotherapy with encorafenib, binimetinib plus cetuximab in patients with surgically resectable braf V600E mutant colorectal metastasis (NEXUS study) [https://jrct.niph.go.jp/en-latest-detail/jRCT2031220025].
Nakamura Y, Okamoto W, Kato T, Esaki T, Kato K, Komatsu Y, Yuki S, Masuishi T, Nishina T, Ebi H, et al. Circulating tumor DNA-guided treatment with pertuzumab plus trastuzumab for HER2-amplified metastatic colorectal cancer: a phase 2 trial. Nat Med. 2021;27:1899–903.
Sakamoto Y, Bando H, Nakamura Y, Hasegawa H, Kuwaki T, Okamoto W, Taniguchi H, Aoyagi Y, Miki I, Uchigata H, et al. Trajectory for the regulatory approval of a combination of pertuzumab plus trastuzumab for pre-treated HER2-positive metastatic colorectal cancer using real-world data. Clin Colorectal Cancer. 2023;22:45–52.
Bando H, Ohtsu A, Yoshino T. Therapeutic landscape and future direction of metastatic colorectal cancer. Nat Rev Gastroenterol Hepatol. 2023;20:306–22.
Taniguchi H, Nakamura Y, Kotani D, Yukami H, Mishima S, Sawada K, Shirasu H, Ebi H, Yamanaka T, Aleshin A, et al. CIRCULATE-Japan: Circulating tumor DNA-guided adaptive platform trials to refine adjuvant therapy for colorectal cancer. Cancer Sci. 2021;112:2915–20.
Kotani D, Oki E, Nakamura Y, Yukami H, Mishima S, Bando H, Shirasu H, Yamazaki K, Watanabe J, Kotaka M, et al. Molecular residual disease and efficacy of adjuvant chemotherapy in patients with colorectal cancer. Nat Med. 2023;29:127–34.
Multi-center clinical trial for personalized perioperative chemotherapy based on genetic alteration status for resectable oligometastases from colorectal cancer [https://upload.umin.ac.jp/cgi-open-bin/ctr/ctr_view.cgi?recptno=R000048502].
Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, Hasegawa K, Hotta K, Ishida H, Ishiguro M, et al. Japanese Society for Cancer of the Colon and Rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol. 2020;25:1–42.
Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1). Eur J Cancer. 2009;45:228–47.
A Multicenter Study on Biomarker Development Utilizing AI Multiomics for Patients with Advanced Solid Malignant Tumors [https://center6.umin.ac.jp/cgi-open-bin/ctr_e/ctr_view.cgi?recptno=R000050019].
Javed S, Benoist S, Devos P, Truant S, Guimbaud R, Lievre A, Sefrioui D, Cohen R, Artru P, Dupre A, et al. Prognostic factors of BRAF V600E colorectal cancer with liver metastases: a retrospective multicentric study. World J Surg Oncol. 2022;20:131.
Johnson B, Jin Z, Truty MJ, Smoot RL, Nagorney DM, Kendrick ML, Kipp BR, Grothey A. Impact of Metastasectomy in the multimodality approach for BRAF V600E metastatic colorectal cancer: the mayo clinic experience. Oncologist. 2018;23:128–34.
Newhook TE, Chun YS, Vauthey JN. An Odyssey into the Land of Deleterious Rare Mutations in Colorectal Liver Metastases. Ann Surg Oncol. 2020;27:3115–7.
Amaria RN, Prieto PA, Tetzlaff MT, Reuben A, Andrews MC, Ross MI, Glitza IC, Cormier J, Hwu WJ, Tawbi HA, et al. Neoadjuvant plus adjuvant dabrafenib and trametinib versus standard of care in patients with high-risk, surgically resectable melanoma: a single-centre, open-label, randomised, phase 2 trial. Lancet Oncol. 2018;19:181–93.
Acknowledgements
We are grateful to all participating patients, their families, and all investigators involved in the NEXUS trial.
Funding
The NEXUS trial is funded by the Advanced Research and Development Programs for Medical Innovation of Japan Agency for Medical Research and Development (21lk0201148h0001). Encorafenib and binimetinib were provided by ONO PHARMACEUTICAL CO., LTD., and cetuximab was provided by Merck Biopharma Co., Ltd., Tokyo, Japan, an affiliate of Merck KGaA (CrossRef Funder ID: 10.13039/100009945). The funding bodies do not affect the design of the study, data collection, data analysis, interpretation of data, and writing the manuscript.
Author information
Authors and Affiliations
Contributions
SK, HB, ST, and TY conceived study concepts. SK, HB, AT, TT, ES, MS, HH, KY, KK, NM, TK, YK, MY, EO, RK, MW, ST, TY designed the study protocol. MW is engaged in statistical analysis. All the authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The current study has been approved by the Institutional Review Board of National Cancer Center Hospital East (EPOC2101), and permission for conducting the study has been obtained from the IRB of all participating facilities. All procedures will be performed in accordance with the protocol, Declaration of Helsinki, governmental laws and regulations, and their revisions and related notifications. All patients are required to sign written informed consent.
Consent for publication
Not applicable.
Competing interests
SK reports honoraria from Ono, Johnson & Johnson, and Asahi Surgical Robotics.
HB reports research funding from Takeda, Daiichi Sankyo, and Sysmex, and honoraria from Takeda, Chugai, Taiho, and Eli Lilly.
ES reports honoraria from Takeda, Merck, Eli Lily, and Chugai.
MS reports honoraria from Eli Lilly, Takeda, Taiho, Ono, Yakult, and Merck.
HH reports honoraria from Bayer, Bristol-Myers Squibb, Chugai, Daiichi Sankyo, Kyowa Hakko Kirin, Eli Lilly, Merck, MSD, Ono, Taiho, Takeda, and Yakult, having consulting or advisory roles in Bristol-Myers Squibb, Boehringer Ingelheim, Daiichi Sankyo, Dainippon Sumitomo, MSD, and Ono, and receiving research grants from ALX oncology, Amgen, Astellas, AstraZeneca, Bayer, BeiGene, Boehringer Ingelheim, Bristol-Myers Squibb, Chugai, Daiichi Sankyo, Eisai, Janssen, Merck, MSD, Ono, and Taiho.
KY reports honoraria from Chugai, Daiichi Sankyo, Yakult, Takeda, Bayer, Merck, Taiho, Eli Lilly, Sanofi, Ono, MSD, and Bristol-Myers Squibb.
NM reports honoraria from Merk and research funding from Ono.
YK reports honoraria from Chugai, Eli Lilly, Takeda, Bayer Yakuhin, Taiho, MSD, Ono, Yakult, Merck, and Sanofi.
EO reports research funding from Guardant Health and honoraria from Ono, Takeda, Bayer, Chugai, Taiho, Eli Lilly, and Bristol-Myers Squibb.
ST reports honoraria from Taiho and VIATRIS.
AT, TT, KK, MY, TK, and MW have no conflicts to declare.
TY reports research funding from Novartis Pharma, MSD, Sumitomo Dainippon, Chugai, Sanofi, Daiichi Sankyo, Parexel, and Ono.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kobayashi, S., Bando, H., Taketomi, A. et al. NEXUS trial: a multicenter phase II clinical study evaluating the efficacy and safety of the perioperative use of encorafenib, binimetinib, and cetuximab in patients with previously untreated surgically resectable BRAF V600E mutant colorectal oligometastases. BMC Cancer 23, 779 (2023). https://doi.org/10.1186/s12885-023-11311-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-023-11311-5