Abstract
Background
Hyperglycemia during pregnancy leads to adverse maternal and fetal outcomes. Thus, strict monitoring of blood glucose levels is warranted. This study aims to determine the association of early to mid-pregnancy HbA1c levels with the development of pregnancy complications in women from three countries in South Asia and Sub-Saharan Africa.
Methods
We performed a secondary analysis of the AMANHI (Alliance for Maternal and Newborn Health Improvement) cohort, which enrolled 10,001 pregnant women between May 2014 and June 2018 across Sylhet-Bangladesh, Karachi-Pakistan, and Pemba Island-Tanzania. HbA1c assays were performed at enrollment (8 to < 20 gestational weeks), and epidemiological data were collected during 2–3 monthly household visits. The women were followed-up till the postpartum period to determine the pregnancy outcomes. Multivariable logistic regression models assessed the association between elevated HbA1c levels and adverse events while controlling for potential confounders.
Results
A total of 9,510 pregnant women were included in the analysis. The mean HbA1c level at enrollment was found to be the highest in Bangladesh (5.31 ± 0.37), followed by Tanzania (5.22 ± 0.49) and then Pakistan (5.07 ± 0.58). We report 339 stillbirths and 9,039 live births. Among the live births were 892 preterm births, 892 deliveries via cesarean section, and 532 LGA babies. In the multivariate pooled analysis, maternal HbA1c levels of ≥ 6.5 were associated with increased risks of stillbirths (aRR = 6.3, 95% CI = 3.4,11.6); preterm births (aRR = 3.5, 95% CI = 1.8–6.7); and Large for Gestational Age (aRR = 5.5, 95% CI = 2.9–10.6).
Conclusion
Maternal HbA1c level is an independent risk factor for predicting adverse pregnancy outcomes such as stillbirth, preterm birth, and LGA among women in South Asia and Sub-Saharan Africa. These groups may benefit from early interventional strategies.
Similar content being viewed by others
Background
Hyperglycemia in pregnancy affected around 21.1 million (16.7%) live births in 2021. The majority (80.3%) of these were diagnosed for the first time during pregnancy and went on to be classified as Gestational Diabetes Mellitus (GDM) [1]. The burden is disproportionately higher in low- and middle-income countries (LMICs) where socioeconomic and environmental stressors such as exposure to poor nutrition in early childhood, limited access to healthcare facilities, and a genetic predisposition in certain ethnicities are thought to contribute to the higher burden [2, 3]. Several studies have shown a linear relationship between blood glucose levels during pregnancy with adverse maternal–fetal outcomes and the risk of diabetes mellitus later in life [4]. Increased placental transport of glucose leads to elevated fetal insulin and insulin-like growth factor 1 (IGF-1) levels causing fetal overgrowth or macrosomia [5]. Macrosomia increases the risk of obstructed labor and cesarean delivery [6]. Excess fetal insulin production can contribute to β-cell dysfunction and insulin resistance, increasing the risk of hypoglycemia and brain injury after birth [7]. There is also increased risk of stillbirth and preterm births, due to mechanisms such as oxidative stress, placental dysfunction, pre-eclampsia, and fetal macrosomia [8]. Thus, it is important to screen women for elevated glucose levels to prevent serious complications of pregnancy. The American Diabetes Association (ADA) has recommended fasting blood glucose levels and oral glucose tolerance test (OGTT) as the gold standard diagnostic tests for GDM [9]. However, both of these tests require prolonged fasting and the Oral Glucose Tolerance Test (OGTT) can be practically burdensome in low-resource settings with limited access to healthcare. In contrast, the glycated hemoglobin (HbA1c) is a test which gives average glucose levels during the preceding 90–120 days. It is routinely used for monitoring glycemic control in diabetic patients. An HbA1c percent greater than 6.5 is diagnostic of diabetes mellitus in non-pregnant individuals [10]. In addition, if performed as a point-of-care test, it can improve testing compliance for monitoring hyperglycemia in a single visit. However, there is currently no clear consensus on its use in the screening and management of pregnant women for GDM.
Thus, in this paper, we refer to our experience of performing point of care HbA1c testing as a biomarker of hyperglycemia during early to mid-pregnancy on a large cohort of pregnant women across three countries in Asia and Africa and its association with adverse pregnancy outcomes like stillbirth, preterm birth, large for gestational age and cesarean section [11].
Methods
Study design and setting
We performed a secondary data analysis on a large cohort of pregnant women enrolled as part of the Alliance for Maternal and Child Health Improvement (AMANHI) biorepository study. Between May 2014 and June 2018, the AMANHI study enrolled 10,001 pregnant women between 8—< 20 weeks of gestational age from Bangladesh, Pakistan, and Tanzania. A detailed description of the study sites and characteristics of the cohort has been published previously [11]. Briefly, women were enrolled after confirming pregnancy and gestational age through ultrasound scan, and blood and urine samples were collected using standardized methods across the three sites at the time of enrollment, 24–28 or 32–36 weeks of gestation, at the time of birth and 6 weeks after delivery. Placental tissue and maternal and newborn stool samples were also collected at the time of birth. In addition, a paternal saliva sample was collected. At each contact, trained field workers collected detailed information on the health and care seeking behavior of the pregnant woman using a standardized tool across all sites [11].
For HbA1c testing, trained phlebotomists collected 0.25–0.50 ml of maternal venous blood in a purple top 7.5 ml EDTA tube (S-Monovette). HbA1c level was measured via a monoclonal antibody agglutination reaction using the Siemens DCA Vantage® Analyzer (Siemens, Washington, USA), with controls traceable to the International Federation of Clinical Chemistry (IFCC) reference materials and test methods for measurement of HbA1c. The normal range of this HbA1c level measurement was within 2.5% to 14% units (4 mmol/mol to 130 mmol/mol) according to the manufacturer.
Statistical analysis
The primary exposure variable for this analysis was HbA1c levels measured at enrollment (8 to < 20 weeks of gestation) and categorized based on the ADA guidelines into: less than 5.7%, 5.7–6.4% and ≥ 6.5% [12]. For the outcomes of interest, stillbirths were defined as babies who were born dead after 22 weeks of gestation. Among livebirths, preterm births were defined as livebirths before 37 weeks of gestation; large for gestational age (LGA) births were defined as liveborn with a birthweight above 90th percentile based on INTERGROWTH-21st standards [13]. Mid-upper arm circumference (MUAC) was categorized as severely malnourished < 21 cm, moderately malnourished ≥ 21 cm & < 23 cm, and normal ≥ 23 cm. Body Mass Index (BMI) was categorized as underweight < 18.5, normal ≥ 18.5 & < 25.0, overweight ≥ 25.0and obese ≥ 30.0. The fourth outcome was children born through cesarean section.
For descriptive purposes, all continuous variables were expressed as mean ± SD and categorical variables as frequencies with percentages. Generalized binomial regression was used to estimate crude and adjusted risk ratios for HbA1c levels with the four predefined outcomes. We used stepwise regression with forward selection. The final multivariate model had all variables with a p-value less than 0.05. The model was adjusted for the following covariates: maternal age; education status; wealth quintile; parity; gravidity; MUAC; BMI; smoking and tobacco use; exposure to biomass; history of previous stillbirths, miscarriages, caesarean section, and preterm birth; hypertension; diabetes; anemia; gender of the fetus; place and mode of delivery; and history of antepartum and postpartum hemorrhage. Women with missing HbA1c levels at enrollment, multiple births, abortive outcomes, and those missing outcome information were excluded from the analyses. All analysis was performed using Stata version 15.0.
Patient and public involvement
It was not appropriate or possible to involve patients or the public in the design, conduct, or reporting, or dissemination plans of our research.
Ethics
The AMANHI study received ethical approval from the local and institutional ethics committees of all the three sites. These included Zanzibar Health Research Ethics Committee (formerly ZAMREC) (ZAMREC/0002/OCTOBER/013) for Tanzania, ICDDR, B (PR12073) and John Hopkins University (IRB 00004508) for Bangladesh and Aga Khan University (2790-paeds-ERC-13) for Pakistan. In addition, the protocols for the biorepository study were also approved by the WHO Ethics Review Committee (RPC 532) and continuing approvals were sought yearly. Written informed consent was obtained from study participants in which all study and sample handling and study procedures were explained in detail. HbA1c results were also shared with these participants.
Results
Pregnancy outcomes and maternal characteristics
A total of 10,001 women were enrolled in the study across the three sites from May 2014 and June 2018. HbA1c levels at enrolment were missing for 293 pregnant women; 137 women had multifetal pregnancies; 132 pregnancies ended in abortion or a miscarriage, and outcome information was missing for 61 women. These were excluded from the analysis. The remaining pregnancies (n = 9,378) resulted in 9,039 liveborn babies (96.4%) and 339 stillbirths (3.6%). There were 892 preterm births (9.8%), 892 women underwent a C-Sect. (9.8%), and 532 babies were born large for gestational age (5.9%). The site-wise distribution of these pregnancy outcomes is given in Fig. 1.
Table 1 summarizes the clinical and sociodemographic characteristics of the enrolled women.
Most women were in the 20–29 years age bracket with the lowest mean maternal age found in Bangladesh (23.46 ± 4.44 years). In total 679 (7.1%) women were severely malnourished and 1323 (13%) were moderately malnourished, with the highest percentage of malnourished women in Bangladesh. Pakistan site had the highest proportion of women who had no formal education (52%, n = 1284). History of miscarriage in a previous pregnancy was also highest in Pakistan (30%, n = 735).
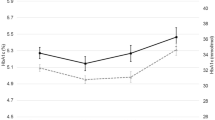
Mean HbA1c levels at enrollment for the whole cohort was 5.2% (± 0.5%). It was highest for Bangladesh (5.31 ± 0.37), followed by Tanzania (5.22 ± 0.49) and then Pakistan (5.07 ± 0.58) (Fig. S1). Using the ADA cutoff values for diabetes mellitus, 8486 number of women (89%) had HbA1c levels below 5.7%, 946 (10%) had HbA1c levels between 5.7 -6.4, and 78 (1%) were above ≥ 6.5%. Tanzania site had the highest number of women 42 (6.5%) with HbA1c levels more than 6.5 (Table 2).
Figure S2a, b and c show the HbA1c levels by categories of maternal Age, BMI and MUAC across all study sites.
Association of HbA1c levels with adverse pregnancy outcomes
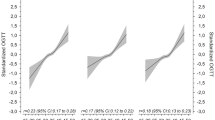
Table 3 and Fig. 2 (a,b,c and d) shows the association between HbA1c levels at less than 20 gestational weeks and adverse pregnancy outcomes across all sites. In the unadjusted model, HbA1c levels ≥ 6.5 were found to be significantly associated with stillbirths (RR = 5.7, 95% CI 3.6,9.1), preterm births (RR = 2.6, 95%CI 1.7,4.1), LGA (RR = 6.0, 95%CI 4.2, 8.6) and C-section deliveries (RR = 2.1, 95%CI 1.3,5.3).
In the multivariate analysis, the adjusted relative risks (aRR) for HbA1c levels 5.7–6.4 were (aRR = 1.2, 95% CI 0.9, 1.7) for stillbirths; (aRR = 1.2, 95% CI 0.9, 1.6) for preterm births; and (aRR = 1.2, 95% CI 0.9, 1.6) for LGA. For HbA1c levels ≥ 6.5, the aRR was (aRR = 6.3, 95% CI 3.4, 11.6) for stillbirths; (aRR = 3.5, 95% CI 1.8, 6.7) for preterm births; and (aRR = 5.5, 95% CI 2.9, 10.6) for LGA. (Table 4).
Discussion
In our study, maternal HbA1c levels during early to mid- pregnancy (8 to < 20 gestational weeks) were associated with stillbirth, preterm birth, and LGA deliveries in Bangladesh, Pakistan and Tanzania. The majority of hyperglycemia during pregnancy remains undiagnosed in sub-Saharan Africa and South Asia [14]. Only half of the pregnant women in these regions receive the minimum recommended four antenatal care visits and most of the births occur at home, typically attended by traditional birth attendants who lack skills to manage the complications of hyperglycemia in pregnancy [15]. In this situation, point-of-care HbA1c testing during early to mid-pregnancy can serve as an optimal biomarker for identifying women at an increased risk of adverse outcomes. The ADA has previously suggested that HbA1c levels below 6.0% (42 mmol/mol) in mid-pregnancy are associated with the lowest risk of maternal complications [16]. In our study, 97.1% of the women had HbA1c levels below this cutoff, suggesting that women above this cutoff could be predisposed to adverse outcomes. We also found the ADA defined category of 6.5 and above for the diagnosis of diabetes mellitus in non-pregnant population to be associated with a higher risk of adverse pregnancy outcomes. Thus, a target of < 5.7% could be optimal during pregnancy in our population, provided it can be achieved without significant hypoglycemia.
There have been several previous attempts to define an optimal HbA1c cut-off for predicting adverse pregnancy outcomes in healthy pregnant women without pre-existing diabetes. The HAPO Study (Hyperglycemia and Adverse Pregnancy Outcomes), enrolled 5000 women across the globe and found that higher HbA1c levels at 24–32 weeks of gestation were associated with an increased risk of primary cesarean delivery, neonatal hypoglycemia, and large-for-gestational-age infants [17]. A longitudinal study from New Zealand conducted by Hughes et al. including 16,122 women predominantly of non-Hispanic white origin, demonstrated that a first trimester HbA1c threshold of 5.9% was associated with an increased risk of adverse pregnancy outcomes, including major congenital anomaly, preeclampsia, perinatal death, large for gestational age and preterm birth [18]. This cut-off is also lower than the ADA-defined cut-off of ≥ 6.0%. Bender et al., reported a cut-off of ≥ 5.7% at the first prenatal visit which could be used to identify women at increased risk for adverse pregnancy outcomes, including preterm birth, small for gestational age infants, and admission to the neonatal intensive care unit [19]. In addition, Antoniou et al. proposed an even lower cut-off of ≥ 5.5% was associated with an increased risk of adverse pregnancy outcomes, including pre-eclampsia, preterm birth, and LGA infants [20]. A large prospective nationwide birth cohort study from Japan with HbA1c < 6.5% (< 48 mmol/mol) reported that every 1% (11 mmol/mol) increase in HbA1c levels measured less than 24 weeks of gestation, were directly associated with a higher risk of adverse pregnancy outcomes [21]. Similarly, another study by Mane et al., in a multiethnic community reported that an early HbA1c level of 5.9%, unrelated to GDM, indicated an increased risk for macrosomia [22].
Our results require cautious interpretation since the HbA1c categories used in our study were developed by ADA for the diagnosis of diabetes in non-pregnant individuals. In women with pre-existing diabetes, early pregnancy HbA1c levels directly correlate with pregnancy outcomes [22,23,24], but this association is still ambiguous in those without diabetes. It is also important to note that the predictive value of HbA1c for adverse outcomes may vary depending on factors such the timing of HbA1c measurement during pregnancy. Carlsen et al. examined the association between HbA1c levels measured during mid-pregnancy and adverse outcomes in women with pre-existing diabetes. The study found that HbA1c levels in the upper quartile (but still within the generally accepted normal range) are at increased risk of preterm delivery and preeclampsia [25]. Similarly, Hong et al. investigated that predelivery HbA1c at term in a healthy pregnant population is a potential predictor for adverse pregnancy outcomes such as c-section deliveries [26]. Nielsen et al. found that HbA1c was lower in early pregnancy and further decreased in late pregnancy compared with age-matched nonpregnant women. A decrease of the upper normal limit of HbA1c from 6.3% before pregnancy to 5.6% in the third trimester of pregnancy was of significant clinical importance [27]. Thus, it may not be possible to compare the studies performed at different time points during pregnancy.
The relationship between HbA1c levels and adverse pregnancy outcomes also varies by ethnicity. Results from a multiethnic cohort study in Barcelona, corresponded to a significant association between high normal range HbA1c and the risk of macrosomia, but no associations between the HbA1c level with preterm birth and LGA could be established after adjustment of potential confounders [22]. These results could in part be attributed to the differences in ethnic origins of the study populations. The research by Hughes et al. was conducted in a relatively low-risk, predominantly white population, whereas the cohort in the current study was characterized by an entirely south Asian or African population hailing from very different socio-economic settings and health conditions [18]. Previous studies reported an interracial variability in HbA1c levels and in pregnancy outcomes [23, 28].
Studies indicate that 70–85% of women diagnosed with GDM according to Carpenter-Coustan or National Diabetes Data Group (NDDG) criteria can effectively control GDM through lifestyle modifications alone and some pregnant women with hyperglycemia may require frequent glucose testing and continuous use of either oral or injectable medications [29,30,31]. Thus, adopting the early to mid-pregnancy point-of-care test HbA1c test in community-settings can enable timely management and targeted pregnancy-focused education for future risk reduction. The costs of identifying a greater number of the pregnant population to be at an increased risk of adverse outcomes could be balanced by the efficient management of the hyperglycemia and avoidance of consequent healthcare costs associated with an LGA or preterm delivery.
We studied a large population-based cohort of women in a setting with universal HbA1c testing in early pregnancy, minimizing the potential for selection bias. We used standardized cut-offs which may cause ease of comparison with other studies. Our study adjusted for systemically identified confounders in a general pregnant population. Our population was well defined, and our sample size appropriately calculated for a multivariable binary logistic regression analysis. Our study population was multiethnic, and we believed our results would be generalizable to a similar population and care setting.
Our study has some limitations. The ADA defined cut-offs were developed specifically for diagnosing diabetes and monitoring blood glucose control in diabetic patients, not for predicting pregnancy outcomes in healthy pregnant women. Therefore, it is possible that these cut-offs may not be optimal for predicting pregnancy outcomes in this population. Although we carefully adjusted for potential confounders, we are unlikely to completely rule out the possibility of vestigial confounding by other undocumented determinants, such as family history of diabetes, diagnosis of GDM in a prior pregnancy, gestational weight gain, dietary nutrition during gestation, and other socioeconomic parameters. Additionally, it is also widely recognized that hemoglobinopathies are more frequent in some nonwhite populations and that their presence might influence HbA1c levels [32]. Furthermore, in this study, pregnant women were not screened for GDM, which meant that it could not be included as a confounder and so an expected influence on results is a rational possibility.
Conclusion
In conclusion, maternal HbA1c level is an independent risk factor for predicting adverse pregnancy outcomes such as stillbirth, preterm birth, and LGA among women in South Asia and Sub-Saharan Africa. These groups may benefit from early interventional strategies. Further research is required to predict the diagnostic accuracy of the test as compared to the gold standard in these settings.
Availability of data and materials
Data are available from the corresponding author upon reasonable request.
References
Federation; ID. IDF DIABETES ATLAS. 10th ed. Brussels; 2021.
Barker DJ. The origins of the developmental origins theory. J Intern Med. 2007;261(5):412–7.
Kanguru L, Bezawada N, Hussein J, Bell J. The burden of diabetes mellitus during pregnancy in low- and middle-income countries: a systematic review. Glob Health Action. 2014;7:23987.
Farrar D. Hyperglycemia in pregnancy: prevalence, impact, and management challenges. Int J Womens Health. 2016;8:519–27.
Jansson T, Cetin I, Powell TL, Desoye G, Radaelli T, Ericsson A, et al. Placental transport and metabolism in fetal overgrowth a workshop report. Placenta. 2006;27(Suppl A):S109–13.
Herzberg S, Kabiri D, Mordechai T, Haj Yahya R, Chill H, Levitt L, et al. Fetal macrosomia as a risk factor for shoulder dystocia during vacuum extraction. J Matern Fetal Neonatal Med. 2017;30(15):1870–3.
Fetita LS, Sobngwi E, Serradas P, Calvo F, Gautier JF. Consequences of fetal exposure to maternal diabetes in offspring. J Clin Endocrinol Metab. 2006;91(10):3718–24.
Ornoy A, Becker M, Weinstein-Fudim L, Ergaz Z. Diabetes during Pregnancy: A Maternal Disease Complicating the Course of Pregnancy with Long-Term Deleterious Effects on the Offspring. A Clinical Review. Int J Mol Sci. 2021;22(6):2965.
Rani PR, Begum J. Screening and Diagnosis of Gestational Diabetes Mellitus, Where Do We Stand. J Clin Diagn Res. 2016;10(4):Qe01–4.
Sherwani SI, Khan HA, Ekhzaimy A, Masood A, Sakharkar MK. Significance of HbA1c Test in Diagnosis and Prognosis of Diabetic Patients. Biomark Insights. 2016;11:95–104.
Aftab F, Ahmed S, Ali SM, Ame SM, Bahl R, Baqui AH, et al. Cohort Profile: The Alliance for Maternal and Newborn Health Improvement (AMANHI) biobanking study. Int J Epidemiol. 2022;50(6):1780–1.
Association AD. Standards of medical care in diabetes—2011. Diabetes care. 2011;34(Supplement_1):S11–61.
Papageorghiou AT, Kennedy SH, Salomon LJ, Altman DG, Ohuma EO, Stones W, et al. The INTERGROWTH-21(st) fetal growth standards: toward the global integration of pregnancy and pediatric care. Am J Obstet Gynecol. 2018;218(2s):S630–40.
Sun H, Saeedi P, Karuranga S, Pinkepank M, Ogurtsova K, Duncan BB, et al. IDF Diabetes Atlas: Global, regional and country-level diabetes prevalence estimates for 2021 and projections for 2045. Diabetes Res Clin Pract. 2022;183: 109119.
WHO. Antenatal care coverage - at least four visits (%). 2020.
Committee ADAPP. 15. Management of Diabetes in Pregnancy: Standards of Medical Care in Diabetes—2022. Diabetes Care. 2021;45(Supplement_1):S232–43.
Lowe LP, Metzger BE, Dyer AR, Lowe J, McCance DR, Lappin TR, et al. Hyperglycemia and Adverse Pregnancy Outcome (HAPO) Study: associations of maternal A1C and glucose with pregnancy outcomes. Diabetes Care. 2012;35(3):574–80.
Hughes RC, Moore MP, Gullam JE, Mohamed K, Rowan J. An early pregnancy HbA1c≥ 5.9%(41 mmol/mol) is optimal for detecting diabetes and identifies women at increased risk of adverse pregnancy outcomes. Diabetes Care. 2014;37(11):2953–9.
Bender W, McCarthy C, Chittams J, Elovitz M, Parry S, Durnwald C. 990: In the absence of diabetes, an early elevated HbA1c is associated with adverse pregnancy outcomes. Am J Obstet Gynecol. 2020;222:S615–6.
Antoniou M-C, Gilbert L, Gross J, Rossel J-B, Fischer Fumeaux CJ, Vial Y, et al. Potentially modifiable predictors of adverse neonatal and maternal outcomes in pregnancies with gestational diabetes mellitus: can they help for future risk stratification and risk-adapted patient care? BMC Pregnancy Childbirth. 2019;19(1):469.
Iwama N, Sugiyama T, Metoki H, Saito M, Hoshiai T, Watanabe Z, et al. Associations between glycosylated hemoglobin level at less than 24 weeks of gestation and adverse pregnancy outcomes in Japan: The Japan Environment and Children’s Study (JECS). Diabetes Res Clin Pract. 2020;169: 108377.
Mañé L, Flores-Le Roux JA, Benaiges D, Rodríguez M, Marcelo I, Chillarón JJ, et al. Role of First-Trimester HbA1c as a Predictor of Adverse Obstetric Outcomes in a Multiethnic Cohort. J Clin Endocrinol Metab. 2017;102(2):390–7.
Bleyer AJ, Hire D, Russell GB, Xu J, Divers J, Shihabi Z, et al. Ethnic variation in the correlation between random serum glucose concentration and glycated haemoglobin. Diabet Med. 2009;26(2):128–33.
Likhari T, Gama R. Glycaemia-independent ethnic differences in HbA(1c) in subjects with impaired glucose tolerance. Diabet Med. 2009;26(10):1068–9.
Carlsen EØ, Harmon Q, Magnus MC, Meltzer HM, Erlund I, Stene LC, et al. Glycated haemoglobin (HbA1c) in mid-pregnancy and perinatal outcomes. Int J Epidemiol. 2022;51(3):759–68.
Hong JGS, Fadzleeyanna MYN, Omar SZ, Tan PC. HbA1c at term delivery and adverse pregnancy outcome. BMC Pregnancy Childbirth. 2022;22(1):679.
Nielsen LR, Ekbom P, Damm P, Glümer C, Frandsen MM, Jensen DM, et al. HbA1c Levels Are Significantly Lower in Early and Late Pregnancy. Diabetes Care. 2004;27(5):1200–1.
Hartland A, Smith J, Clark P, Webber J, Chowdhury T, Dunne F. Establishing trimester-and ethnic group-related reference ranges for fructosamine and HbA1c in non-diabetic pregnant women. Ann Clin Biochem. 1999;36(2):235–7.
Harper LM, Mele L, Landon MB, Carpenter MW, Ramin SM, Reddy UM, et al. Carpenter-Coustan Compared With National Diabetes Data Group Criteria for Diagnosing Gestational Diabetes. Obstet Gynecol. 2016;127(5):893–8.
Practice Bulletin No. 137: Gestational diabetes mellitus. Obstet Gynecol. 2013;122(2 Pt 1):406–16.
National Institutes of Health consensus development conference statement. diagnosing gestational diabetes mellitus, March 4–6, 2013. Obstet Gynecol. 2013;122(2 Pt 1):358–69.
Rafat D, Ahmad J. HbA1c in pregnancy. Diabetes Metab Syndr. 2012;6(1):59–64. https://doi.org/10.1016/j.dsx.2012.05.010.
Acknowledgements
We thank all the mothers and children who participated in the study.
Funding
This work was supported by the Bill & Melinda Gates Foundation through a grant to the World Health Organization, Grant Number (64438). The funders have played no role in the drafting of the manuscript and the decision to submit for publication.
Author information
Authors and Affiliations
Contributions
The study was conceptualized and designed by principal investigators of the three sites (AB (Bangladesh), FJ (Pakistan), and SS (Tanzania)), AM, YS, and RB. All authors from three sites (Bangladesh, Pakistan, and Tanzania) conducted the acquisition of data. MIN, FJ and JK wrote the first draft of the manuscript that was reviewed by all authors. All the authors have read and approved the final manuscript. All authors had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The AMANHI study received ethical approval from the local and institutional ethics committees of all the three sites. These included Zanzibar Health Research Ethics Committee (formerly ZAMREC) (ZAMREC/0002/OCTOBER/013) for Tanzania, ICDDR, B (PR12073) and John Hopkins University (IRB 00004508) for Bangladesh and Aga Khan University (2790-paeds-ERC-13) for Pakistan. In addition, the protocols for the biorepository study were also approved by the WHO Ethics Review Committee (RPC 532) and continuing approvals were sought yearly. Written informed consent was obtained from study participants in which all study and sample handling and study procedures were explained in detail. HbA1c results were also shared with these participants.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Figure S1. Mean Hba1c levels site-wise. Figure S2. HbA1c Levels by (a) Maternal Age, (b) BMI and (c) MUAC.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nisar, M.I., das, S., Khanam, R. et al. Early to mid-pregnancy HbA1c levels and its association with adverse pregnancy outcomes in three low middle-income countries in Asia and Sub-Saharan Africa. BMC Pregnancy Childbirth 24, 66 (2024). https://doi.org/10.1186/s12884-023-06241-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12884-023-06241-w