Abstract
Background
Hepatitis B infection due to poor practices can result in prolonged hospital stays, long-term disability, increased microbial resistance, financial burdens and death. There has been no comprehensive study assessing the practice level of hepatitis B virus infection prevention in Ethiopia despite the high risk of exposure. Thus, this review aimed to assess practice on hepatitis B virus infection prevention in Ethiopia.
Methods
For published studies, we conducted a thorough search of the PubMed, African Journal Online, Science Direct, Cochrane Library and Google Scholar databases. The data were exported to STATA version 11 (STATA Corp LLC) for meta-analysis. Heterogeneity between the results of the primary studies was assessed using Cochran’s Q chi-square test and quantified with I2 statistics. A random effect model, specifically the DerSimonian and Laird pooled estimate method, was used due to the presence of heterogeneity between the included articles.
Results and conclusions
Initially, 1738 articles were retrieved through electronic database searching. Of these, 910 were from Google Scholar, 4 from PubMed, 378 from Science Direct, 421 from African Journal Online and 25 from the Cochrane Library. The pooled estimate showed that 41.54% (95% CI: 33.81–49.27, P < 0.001) of individuals had a good practice towards hepatitis B virus infection prevention. Good knowledge of HBV infection prevention (POR = 1.13, 95% CI: (0.28–4.46) and urban residence (POR = 4.27, 95% CI: 1.17–15.49) were factors significantly associated with practices aimed at preventing hepatitis B virus infection. Based on the findings of the current study, most of the participants reported poor practices for hepatitis B virus infection prevention. Residence and knowledge of hepatitis B virus prevention were significantly associated with practices aimed at preventing hepatitis B virus infection. The Ministry of Health should collaborate with the health bureau for continual awareness about the mode of transmission and preventive measures of HBV.
Similar content being viewed by others
Introduction
As per the World Health Organization (WHO) in 2019, around 296 million people were living with chronic HBV infection, with 1.5 million new cases annually, leading to 1.3 million deaths from liver cancer and cirrhosis [1, 2]. Globally, hepatitis B infection poses a significant public health challenge for roughly two-thirds of the global population residing in regions with high transmission risks [3]. Without swift and coordinated intervention, the impact of hepatitis B viral infection is expected to worsen, potentially resulting in an estimated 20 million deaths from 2015 to 2030 [4]. A meta-analysis conducted in 2018 found that just 25% of healthcare workers in Africa had received complete vaccination against the hepatitis B virus as part of preventive measures [5]. A systematic review and meta-analysis conducted in Africa revealed that approximately one in fifteen healthcare workers were infected with HBV, and more than one in twenty were infected with HCV. The substantial prevalence of HBV and HCV infections continues to be a significant issue among healthcare workers in Africa [6].
Liver disease advancing to severe stages and the onset of hepatocellular carcinoma (HCC) place substantial burdens on low-income countries. Furthermore, political and socioeconomic challenges often hinder or prevent efforts to prevent, manage, and treat HBV infection and its associated conditions [7]. In the poorest countries with high infection rates, challenges remain due to the cost of vaccines and insufficient implementation of preventive measures. Moving forward, a significant challenge will be addressing social and economic obstacles to sustain and improve global prevention efforts aimed at reducing the worldwide impact of the disease [8].
Both symptomatic and asymptomatic individuals can spread the infection to others, making chronic carriers a continual risk across all demographic groups [9]. Hepatitis B virus (HBV) infection spreads easily from infected individuals to healthy individuals through various means: contact with blood, needle-stick injuries, transmission from mother to fetus during pregnancy, unsafe sexual practices, sharing of personal care equipment like barbershop and beauty salon tools. Additionally, HBV can be transmitted through injection drug use, tattooing, ear piercing, acupuncture, and during dialysis procedures, all of which heighten the risk of infection. [10, 11].
Hepatitis B viral infection poses significant public health risks due to inadequate decontamination and sterilization practices of equipment, as well as poor management of healthcare waste, much of which is hazardous and can lead to various health hazards [12]. All populations face a high risk of hepatitis B viral infection due to frequent exposure to blood and other body fluids, particularly healthcare providers during clinical activities such as administering medications, collecting laboratory samples, and disposing of waste [13]. An updated systematic review and meta-analysis in Ethiopia the pooled prevalence of HBV was high in Ethiopia and it is a major public health threat [14]. Strengthening the scope of the existing vaccination program and the establishment of prevention methods is highly recommended. In addition, it will be better if the existing infection prevention program is revised and target specific task force should be organized at different levels of health facilities [15].
Increased hepatitis B infection burden in Ethiopia resulting from poor practices can lead to prolonged hospital stays, long-term disability, increased microbial resistance, financial strain, and death. Inadequate adherence to hepatitis B virus prevention measures such as improper use of personal protective equipment, needle-stick injuries, and lack of vaccination, particularly in healthcare settings, can contribute to the virus’s high contagiousness and increased prevalence. Despite the global decrease in HBV burden due to widespread immunization campaigns, the current infection rates, especially in developing countries, remain a significant public health concern for the future. Enhancing worldwide prevention policies is essential to mitigate the global impact of this disease.
In Ethiopia, although the risk of Hepatitis B Virus (HBV) infection is notably high, there has yet to be a thorough study evaluating current preventive practices. Conducting such research is essential for informing intervention strategies and will offer important insights for stakeholders focused on diminishing the HBV infection burden. The results will be especially beneficial for program managers and health planners as they design vaccination and other preventive initiatives. Hence, this review was conducted to evaluate the practices related to the prevention of HBV infection in Ethiopia.
Materials and methods
The protocol of this systematic review and meta-analysis was designed according to the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols (PRISMA-P 2015) Guidelines (Supplementary file S1). The Prospero registration number is CRD42024573994
Study setting
The review was conducted using primary studies in Ethiopia.
Search strategy for articles
For published studies, we conducted a thorough search of PubMed, African journals online, Science Direct, the Cochrane Library and Google Scholar using a combination of keywords and Boolean operators (AND & OR) on relevant primary articles reporting the level of practice of hepatitis B virus infection prevention HIV-infected patients in Ethiopia from February 10th to April 10 2024. The keywords used to search the mentioned databases were “prevention practice of hepatitis B virus”, “practice towards hepatitis B virus prevention ”, “hepatitis B virus prevention practice”, “HBV prevention practice”, “hepatitis B surface antigen prevention practice”, “HBsAg prevention practice”, “viral liver disease prevention practice”, “viral hepatitis prevention practice”, and “Ethiopia”. According to the database requirements, the search string was customized for each database. Moreover, a snowball search was used to search the citation lists of included studies. The search incorporated studies articles up to the 10th of April 2024. EndNote (version X7) reference management software was used to download, organize, review, and cite related articles. To identify potentially suitable papers, the two reviewers (WCT and AMZ) blindly examined the titles, abstracts, and full-text search results. Likewise, the whole text of selected papers was thoroughly reviewed in light of the inclusion criteria. For duplicate studies, the first version or the one with all the necessary data was used. Disagreements that occurred during screening were settled by consensus. The qualifying standards for this review were established using the modified Population, Intervention, Comparison, Outcome, and Type of study/context (PICOT) framework Table 1.
Eligibility criteria
Inclusion criteria
Studies were eligible only if they were primary study full-text articles published in peer-reviewed journals, published in the English language, and conducted in Ethiopian settings. In addition, observational studies that reported the prevalence of HBV prevention practices were included.
Exclusion criteria
Studies that did not report the prevalence of HBV prevention practices and studies with poor methodological quality were excluded from the analysis. Other exclusion criteria include studies that are duplicate, unavailable full texts, abstract-only papers containing no extracted data or information, clinical trials, case reports, case series studies, or conference proceedings.
Outcome of interest
The outcome of the review was the practice level, which is defined in primary studies as Good practice: when the study participants were at least able to answer 70% or more practice items on the questionnaire correctly. Malpractice: when the participants were unable to answer 70% of practice items correctly. The practice questions including the following items (always use glove other protective materials while handling different body fluids, always properly dispose needle/ sharps, had a history of needle-stick injury, always report for needle-stick injury, have you ever screened for hepatitis B or C?, have you got yourself vaccinated against hepatitis B?, always keep my hand hygiene before and after all patient contact and have you ever involved in an unsafe sex [16]?
Article selection and data extraction
All the articles retrieved from the abovementioned electronic databases were exported to EndNote X7, and duplicate articles were removed. After removing duplications, two authors (AMZ & YAF) independently screened and excluded ineligible articles. Data extraction was performed using a tool developed by the 2014 Joanna Brings Institute Reviewers’ Manual data extraction format by two authors (AMZ & YAF). The data were extracted by two independent authors (AMZ and YAF) using a data extraction format prepared in a Microsoft Excel spreadsheet. When studies lacked sufficient methodological information or the substance was unclear, the principal authors were approached for clarification via an official email address or phone number. The following data were extracted: the first author’s name, publication year, region, design, sample size, sampling method, prevalence of hepatitis B prevention practice, and factors associated with their odds ratios.
Quality appraisal
Quality assessment was performed using the Joanna Briggs Institute (JBI) critical appraisal checklist for cross-sectional studies using 9 criteria. The critical appraisal tool included nine parameters: yes, no, unclear and not applicable options: (1) appropriate sampling frame, (2) proper sampling technique, (3) adequate sample size, (4) study subject and setting description, (5) sufficient data analysis, (6) use of valid methods for the identified conditions, (7) valid measurement for all participants, (8) appropriate statistical analysis, and (9) adequate response rate. Operationally, a score of 1 was assigned for a yes response, whereas a score of 0 was assigned for no and unclear responses. For each question, a score was assigned (0 for ‘not reported or not appropriate’ and 1 for ‘yes’); the scores were summarized across the items to obtain a total quality score that ranged from 0 to 9. Studies were then classified as having low, medium or high quality when the summed points reached 0–4, 5–7 or 7–9, respectively.
Statistical analysis
Heterogeneity test
The extracted data were exported to STATA version 11 (STATA Corp LLC) for meta-analysis. Heterogeneity between the results of the primary studies was assessed using Cochran’s Q chi-square test and quantified with I2 statistics. A p value of less than 0.05 was considered to indicate statistically significant heterogeneity. Based on the I² statistics, values less than 25% indicated low heterogeneity, values between 50 and 75% indicated medium heterogeneity, and values greater than 75% indicated high heterogeneity. Thus, a random effect model was used to pool the prevalence of good practice since the studies were found to be heterogeneous. A random effect model, specifically the DerSimonian and Laird (D + L) pooled estimate method, was used due to the presence of heterogeneity between the included articles. This model we assumes a distribution with some central value and some degree of variability. As one of the handling mechanisms of heterogeneity, we performed subgroup analysis for the pooled estimate of hepatitis B virus infection prevention practice by sampling technique. Sensitivity analysis was conducted to assess the role of each study in the final result by excluding each study one by one.
Publication bias
Publication bias was assessed by visual inspection of a funnel plot based on the shape of the graph (subjective assessment). The funnel plot graph was symmetrical, which suggested the absence of publication bias. On the other hand, quantitatively (objective assessment), Egger’s regression tests were used to assess publication bias, with a p value less than 0.05 considered indicative of a statistically significant publication bias.
Results
Study selection
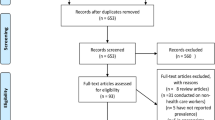
Initially, 1738 articles were retrieved through electronic database searching. Of these, 910 were from Google Scholar, 4 from PubMed, 378 from Science Direct, 421 from African Journal Online and 25 from the Cochrane Library. Of these, 840duplicate articles were removed from EndNote X7. After screening the remaining 898 articles, we excluded 870 articles because their titles were not similar to those of our study and were unrelated to the current study. The full texts of the remaining 28 articles were assessed for eligibility. Additionally, some articles were excluded because their outcomes were not reported or because they were conducted outside of Ethiopia. Finally, the remaining 10 studies fulfilled the inclusion criteria and were enrolled in the study (Fig. 1).
Baseline characteristics of the included articles
Ten published articles were included in this systematic review and meta-analysis. The number of participants in each study ranged from 200 to 422 participants. The included studies utilized cross-sectional methods to assess practices related to hepatitis B virus infection prevention. The included articles were published between 2013 and 2022. Seven of the included studies were from the Amhara region [17,18,19,20,21,22,23], 2 were from Oromia [24, 25], and the remaining were from the South region [26]. All the articles were published in peer-reviewed journals Table 2.
Quality of the included articles
Based on the quality assessment results, nine articles (90%) were of high quality, with scores ranging from 7 to 9, and one study was of medium quality. The quality of each of the included studies was evaluated using the nine items of the Joanna Briggs Institute (JBI) critical appraisal checklist. A detailed assessment of the quality of the studies is provided in the supplementary file (Supplementary file S2).
Meta-analysis
The pooled estimate showed that 41.54% (95% CI: 33.81–49.27, P < 0.001) of individuals had a good practice towards hepatitis B virus infection prevention. The analysis showed that there was medium heterogeneity between the included articles (I²=72.2%, P < 0.001). As a result, random effect models, specifically the DerSimonian and the Laird (D + L) pooled method was used to estimate the pooled prevalence of good practice (Fig. 2).
Subgroup analysis
Since there was a medium level of heterogeneity in this systematic review, subgroup analysis was performed based on the sampling procedure and region. The results of the subgroup analysis based on the sampling procedure showed that a higher prevalence of good practices on hepatitis B prevention was reported in articles that used systematic random sampling (43.98% CI: 33.13, 54.83), and a lower prevalence was reported in articles that used simple random sampling (37.19% CI: 22.82, 51.56) (Fig. 3). The results of the subgroup analysis based on the region showed that a higher prevalence of good practices on hepatitis B prevention was reported in articles that were conducted in South Region (50.30% CI: 36.48, 64.12) (Fig. 4).
Sensitivity analysis
Due to the presence of heterogeneity in the review, a sensitivity analysis was also performed by applying a random effects model. The analysis was performed to evaluate the influence of each study on the pooled prevalence by excluding each study step-by-step. The results showed that the omitted studies did not have a significant influence on the pooled prevalence of good practices aimed at preventing hepatitis B virus infection.
Study omitted | Estimate | [95% Conf. Interval] |
|---|---|---|
Demsiss et al. | 1.126183 | 0 0.28447133, 4.458405 |
Teshome Gebremeskel et al. | 0.55966002 | 0.3721172, 2.84172225 |
Amdehiwot Aynalem et al. | 2.27868531 | 0.4631519, 3.5487819 |
Debaka Belete et al. | 1.126183 | 0.28447133, 4.458405 |
Abdela et al. | 1.126183 | 0.28447133, 4.458405 |
Mesfin, Kibret | 1.126183 | 0.28447133, 4.458405 |
M.D. Allene, G.G. Delelegn | 1.126183 | 0.28447133, 4.458405 |
Habtemu J. Hebo et al. | 1.126183 | 0.28447133, 4.458405 |
Teklay Gebrecherkos et al. | 1.126183 | 0.28447133, 4.458405 |
Yazie et al. | 1.126183 | 0.28447133, 4.458405 |
Combined | 1.1261831 | 0.28447132, 4.4584049 |
Publication bias
We used a funnel plot and Egger’s regression test to check for evidence of publication bias. Visual inspection of the funnel plot indicated a symmetrical distribution (Fig. 5), which was not statistically significant according to the Egger test (P value = 0.091), indicating that there was no significant publication bias among the included studies.
Associated factors of good practice
The pooled estimate of two studies showed that there is a significant association between knowledge of and good practices on hepatitis B virus infection prevention. Those who had good knowledge of HBV infection prevention (POR = 1.13, 95% CI: (0.28–4.46) were 1.13 times more likely to have good practices than those who had poor knowledge of HBV infection prevention. In the random-effects model, heterogeneity was observed among studies (I² = 95.2%) (Fig. 6).
In a meta-analysis of two studies, urban residence was found to be significantly associated with practices for hepatitis B prevention. Participants who lived in urban areas were 4.27 times more likely to practice well than those who lived in rural areas (POR = 4.27, 95% CI: 1.17– 15.49). There was high heterogeneity between studies in the analysis (I² = 92.9%) (Fig. 7).
Discussion
Exposure to hepatitis B virus infection remains a major occupational hazard to the majority of the population, especially in countries where hepatitis B virus infection is prevalent. In Ethiopia, there are no systematic reviews or meta-analyses concerning the prevention of hepatitis B virus infection practice and its associated factors. This study revealed practices for preventing hepatitis B virus infection and its associated factors in Ethiopia. Despite the wide variation of the study participants, this study revealed that 41.54% (95% CI: 33.81– 49.27, P < 0.001) of the study participants practiced HBV infection prevention well. The result of this study is comparable to those of a study conducted in Saudi Arabia, which indicated that 47.2% of the study participants had good practices for HBV infection prevention [27].
However, the findings of this study are greater than those of a study conducted in Nepal, which showed that only 14.2% of the study respondents had good practices [28], and in Honiara, Solomon Islands, which showed that 26.3% of study participants had good practices [29]. The finding from the current study is lower than those from a study conducted in Egypt, in which 68.1% of the participants had good practices, and a study performed in Tamil Nadu, India, in which 76.59% of the study participants had good practices for hepatitis B virus infection prevention [30, 31]. It is still a burden that represents an additional challenge for the national health system which is already fighting with the different infectious and noninfectious disease. This may be due to differences in resource allocation and the perceptions of participants in the area. In the current study, a lack of resources was the main reason for the low prevalence of hepatitis B virus prevention. Unawareness of the vaccine, expensiveness of the vaccine, fear or perceived high risk of HBV infection through occupational exposure, fear of contracting hepatitis from the vaccine, doubt about the efficacy of the vaccine, and absence of post-exposure prophylaxis might be reasons for the low prevalence of clinical practice.
Those who had good knowledge of HBV infection prevention were more likely to practice well than those who had poor knowledge of HBV infection prevention. This finding is consistent with a study performed in Malaysia [32]. Knowledge about prevention methods plays an important role in controlling the risk of hepatitis B infections. Therefore, education should be given regarding the transmission and prevention of HBV with particular emphasis to needle-stick injury and post exposure prophylaxis for every population. This may be because when participants’ knowledge of HBV prevention increases, their practice of preventing hepatitis B virus infection will also increase. Participants who lived in urban areas were more likely to practice well than those who lived in rural areas. Similar results were reported in America [33]. This might be due to the adequate availability of healthcare, high awareness about the availability of vaccines, and the importance of screening for HBV prevention and control through different media for participants living in urban areas.
Limitations
Although this systematic review and meta-analysis provides up-to-date evidence regarding the practice of preventing hepatitis B virus infection, there are several limitations that need to be considered in future research. First, this study lacks studies from some regions of Ethiopia (Afar, Benishangul Gumuz, Somalia, and Tigray), and other regions have a limited number of studies (SNNPR has one study); therefore, it may be difficult to generalize the findings to the national level. Finally, we identified significant heterogeneity across the included studies; thus, the results must be interpreted carefully.
Conclusion and recommendation
Based on the findings of the current study, most of the participants had poor practices for preventing HBV infection. Residence and knowledge of HBV prevention were significantly associated with practices aimed at preventing hepatitis B virus infection. The Ministry of Health should collaborate with the health bureau for continual awareness about the mode of HBV transmission and preventive measures, as well as for providing personal protective equipment and improving the knowledge of communities and good practices to prevent HBV infection, with a focus on rural residents. Therefore, strengthening the scope of the existing vaccination program and the establishment of new sensitive screening methods is highly recommended. In addition, it will be better if the existing infection prevention program is revised and target specific task force should be organized at different levels of health facilities in order to increase the awareness of the community. Control efforts should be scaled up countrywide and novel approaches including screen-and-treat could be implemented to reduce the burden of the disease in Ethiopia. Further political will and strong community awareness will be key to effectively tackling the burden of HBV problem in Ethiopia.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- HBV:
-
Hepatitis B Virus
- IBCS:
-
Institutional-Based Cross-Sectional Study
- POR:
-
Pooled odds ratio
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis
References
Ginzberg D, Wong RJ, Gish R. Global HBV burden: guesstimates and facts. Hep Intl. 2018;12:315–29.
Mansour-Ghanaei R, Joukar F, Souti F, Atrkar-Roushan Z. Knowledge and attitude of medical science students toward hepatitis B and C infections. Int J Clin Exp Med. 2013;6(3):197.
Lavanchy D, Kane M. Global epidemiology of hepatitis B virus infection. Hepatitis B virus in human diseases. 2016:187–203.
Organization WH. Global health sector strategy on viral Hepatitis 2016–2021. Towards ending viral hepatitis. World Health Organization; 2016.
Auta A, Adewuyi EO, Kureh GT, Onoviran N, Adeloye D. Hepatitis B vaccination coverage among health-care workers in Africa: a systematic review and meta-analysis. Vaccine. 2018;36(32):4851–60.
Atlaw D, Sahiledengle B, Tariku Z. Hepatitis B and C virus infection among healthcare workers in Africa: a systematic review and meta-analysis. Environ Health Prev Med. 2021;26(1):61.
Zampino R, Boemio A, Sagnelli C, Alessio L, Adinolfi LE, Sagnelli E, et al. Hepatitis B virus burden in developing countries. World J Gastroenterol. 2015;21(42):11941.
Franco E, Bagnato B, Marino MG, Meleleo C, Serino L, Zaratti L, Hepatitis B. Epidemiology and prevention in developing countries. World J Hepatol. 2012;4(3):74.
Engelkirk PG, Harvey RA, Champe PC, BDF-L W. Microbiology for the health sciences: Lippincott; 2000.
Bosch FX, Ribes J, Cléries R, Díaz M. Epidemiology of hepatocellular carcinoma. Clin Liver Dis. 2005;9(2):191–211.
Parkin DM. The global health burden of infection-associated cancers in the year 2002. Int J Cancer. 2006;118(12):3030–44.
Velvzhi G, Senthil K, Sucilathangam G, Revathy C. Knowledge and attitude of medical students towards hepatitis B infection. Int J Curr Microbiol Appl Sci. 2016;5(6):570–6.
Al-Hazmi A. Knowledge, attitudes, and practice of medical students regarding occupational risks of hepatitis B virus in College of Medicine, Aljouf University. Annals Med Health Sci Res. 2015;5(1):13–9.
Deuffic-Burban S, Delarocque-Astagneau E, Abiteboul D, Bouvet E, Yazdanpanah Y. Blood-borne viruses in health care workers: prevention and management. J Clin Virol. 2011;52(1):4–10.
Yazie TD, Tebeje MG. An updated systematic review and meta-analysis of the prevalence of hepatitis B virus in Ethiopia. BMC Infect Dis. 2019;19:1–13.
Shalaby S, Kabbash I, El Saleet G, Mansour N, Omar A, El Nawawy A. Hepatitis B and C viral infection: prevalence, knowledge, attitude and practice among barbers and clients in Gharbia governorate, Egypt. EMHJ-Eastern Mediterranean Health Journal, 16 (1), 10–17, 2010. 2010.
Demsiss W, Seid A, Fiseha T, Hepatitis B. Seroprevalence, knowledge, practice and associated factors among medicine and health science students in Northeast Ethiopia. PLoS ONE. 2018;13(5):e0196539.
Gebremeskel T, Beshah T, Tesfaye M, Beletew B, Mengesha A, Getie A. Assessment of knowledge and practice on hepatitis B infection prevention and associated factors among health science students in Woldia University, Northeast Ethiopia. Advances in preventive medicine. 2020;2020.
Belete D, Wondale D, Kiros T, Demissie B, Knowledge. Attitude, Practices, and Associated Factor towards Hepatitis B Virus Infection among Health Care Professionals at Tibebe Ghion Specialized Hospital, Bahir Dar, Northwest Ethiopia, 2021: A Cross Sectional Study. International Journal of Hepatology. 2022;2022.
Allene MD, Delelegn GG. Assessment of knowledge, practices and associated factors toward prevention of hepatitis B virus infection among students of medicine and health sciences in Debre Berhan University, NorthShewa, Ethiopia: a cross-sectional study. Int J Surg Open. 2020;24:79–84.
Abdela A, Woldu B, Haile K, Mathewos B, Deressa T. Assessment of knowledge, attitudes and practices toward prevention of hepatitis B virus infection among students of medicine and health sciences in Northwest Ethiopia. BMC Res Notes. 2016;9:1–7.
Gebrecherkos T, Girmay G, Lemma M, Negash M. Knowledge, attitude, and practice towards Hepatitis B virus among pregnant women attending antenatal care at the University of Gondar comprehensive specialized hospital, Northwest Ethiopia. International journal of hepatology. 2020;2020.
Yazie TD, Sharew GB, Abebe W. Knowledge, attitude, and practice of healthcare professionals regarding infection prevention at Gondar University referral hospital, northwest Ethiopia: a cross-sectional study. BMC Res Notes. 2019;12:1–7.
Yonatan Moges Mesfin YMM, Kelemu Tilahun Kibret KTK. Assessment of knowledge and practice towards hepatitis B among medical and health science students in Haramaya University, Ethiopia. 2013.
Hebo HJ, Gemeda DH, Abdusemed KA. Hepatitis B and C viral infection: prevalence, knowledge, attitude, practice, and occupational exposure among healthcare workers of Jimma University Medical Center, southwest Ethiopia. The Scientific World Journal. 2019;2019.
Aynalem A, Deribe B, Ayalew M, Mamuye A, Israel E, Mebratu A et al. Practice towards hepatitis B virus infection prevention and its associated factors among undergraduate students at Hawassa University College of Medicine and Health Sciences, Hawassa, Sidama, Ethiopia, 2021: cross-sectional study. International Journal of Hepatology. 2022;2022.
Saquib S, Ibrahim W, Othman A, Assiri M, Al-Shari H, Al-Qarni A. Exploring the knowledge, attitude and practice regarding hepatitis B infection among dental students in Saudi Arabia: a cross-sectional study. Open Access Macedonian J Med Sci. 2019;7(5):805.
Bhattarai S, Gyawali M, Sapkota S, Karki D, Lamsal S. Knowledge, attitude and practice of hepatitis B vaccination among clinical medical students at a medical college in Nepal. Europasian J Med Sci. 2020;2(2):17–23.
Islands S. Second generation surveillance of antenatal women and youth. Solomon Islands Ministry of Health; 2008.
Atlam SA, Elsabagh HM, Shehab NS, Eldeen N. Knowledge, attitude and practice of Tanta University medical students towards hepatitis B and C. Int J Res Med Sci. 2016;4(3):749–56.
Thote SR, Soyam GC, Dhakate MA. Hepatitis B vaccination status and knowledge, attitude, and practice of hepatitis B among medical students at a medical college in central India. Int J Community Med Public Health. 2023;10(3):1244.
Ahmad A, Munn Sann L, Abdul Rahman H. Factors associated with knowledge, attitude and practice related to hepatitis B and C among international students of Universiti Putra Malaysia. BMC Public Health. 2016;16:1–8.
Charlotte A, Steven Y, Samuel K, Ellen T. Hepatitis B and liver cancer knowledge and preventive practices among Asian americans in the San Francisco Bay Area, California. Asian Pac J Cancer Prev. 2007;8:127–34.
Acknowledgements
The authors thank all the authors of the studies included in this systematic review and meta-analysis.
Funding
The authors received no funding from any specific organization for the study.
Author information
Authors and Affiliations
Contributions
WCT: Writing – review & editing, Writing – original draft, Visualization, Validation, Supervision, Software, Resources, Project administration, Methodology, Investigation, Funding acquisition, Formal analysis, Data curation, Conceptualization. SSW, AMZ and YAF conceived the idea and participated in the data extraction, analysis, and draft writing. WCT, AMZ and YAF participated in the analysis, manuscript preparation, and manuscript revision. All the authors have read and approved the final version of the manuscript to be considered for publication.
Corresponding author
Ethics declarations
Ethical approval
Not applicable since the study used a systematic review and meta-analysis method.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Tassew, W.C., Ferede, Y.A., Zeleke, A.M. et al. Practice on hepatitis B virus infection prevention and associated factors in Ethiopia: systematic review and meta-analysis. BMC Infect Dis 24, 869 (2024). https://doi.org/10.1186/s12879-024-09751-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09751-w