Abstract
Background
Circumcision in hemophiliacs is a delicate surgery because of bleeding risks that could be avoided by adequate substitution of coagulation factor. This practice is very challenging in countries where anti hemophilic treatment is inaccessible. The study aimed to evaluate a circumcision protocol in hemophilia A using low quantities of factor concentrates.
Methods
This prospective study included 26 hemophiliacs A who underwent circumcision in 2014. Medical treatment protocol using low quantity of factor concentrates was drafted by physicians of the Hemophilia Treatment Center and the surgical protocol by experienced surgeons. Assessment criteria were: number of hospitalization days, number of exposure days to factor concentrates, delay to healing and occurrence of bleeding events.
Results
Mean age was 9.6 years (1–30). Hemophiliacs patients were classified as severe (n = 8), moderate (n = 9) and mild form (n = 9). Mean number of exposure days to factor VIII concentrates was 6.9 days (5–12) in children and 10.75 days (7–16) in adults (p = 0.0049); mean number of hospitalization days was 3.68 days (2–10) in children and 13.5 days (13–15) in adults (p = 0.0000); delay to healing was 26.47 days (20–35) in children and 25.25 days (22–30) in adults (p = 0.697); five haemophiliacs (19.2%) presented bleeding events after the circumcision. The mean amount of FIII concentrates used per patient was 1743 IU (810–2340).
Conclusion
The study shows treatment protocol using low quantity of factor concentrates is efficient in hemophilia patients who underwent circumcision.
Similar content being viewed by others
Background
Hemophilia is an inherited bleeding disorder related to sex (F8 and F9 gene are located on X chromosome), due to a deficiency of FVIII (hemophilia A) or FIX (hemophilia B) clotting factors. Hemophilia causes internal bleeding (hematoma, hemarthrosis) or spontaneous external bleeding or following minor trauma or surgery [1, 2].
In Africa, hemophilia is often discovered during circumcision that is the first surgery in young healthy boy and consisting of foreskin removal [3].
There are many and various indications for circumcision according to the different culture and civilization [4,5,6]. In some countries, none circumcision is a very difficult resented for both hemophiliacs and their parents who consider circumcision practice as an act of great religious value and social recognition for the young boy [7, 8]. On the other hand, none circumcision installs a social inferiority complex; so that despite the increased risk of excessive bleeding that can be fatal, hemophiliacs want to be circumcised as well as healthy subjects [9,10,11].
Nevertheless its realization constitutes a real controversy in the world especially if there are no medical indications [12, 13].
Circumcision in hemophilia often requires the use of large quantities of clotting factor concentrates to ensure proper hemostasis. For these reasons, some haemophiliacs can’t be circumcised in countries where factor concentrated are unavailable or not easily accessible. This has led some authors to implement substitutive protocols using low quantities of anti hemophilic factor [14,15,16].
In Senegal, circumcision was performed in 61.4% of followed hemophiliacs’ patients and was the first circumstance of diagnosis in 18% of hemophiliacs [17]. Currently, 179 hemophiliacs are regularly followed at Dakar’s hemophilia treatment center and mean per capita Factor VIII and IX use in 2014 was 0.033 IU in Senegal while the World Federation of Hemophilia recommends 1 IU per capita to ensure the needs of hemophiliacs [18].
In this context, the use of low amounts of factors remains an option for the treatment of hemophilia. For this reason we have evaluated this approach in the context of circumcision of hemophilia patients.
Methods
We included 26 haemophiliacs A with or without inhibitor and who underwent circumcision in 2014. Diagnosis of hemophilia is performed on the basis of prolonged aPTT associated with FVIII levels less than 30% (1). Data collected at the beginning of the study are presented in Table 1. Hemophiliacs were monitored regularly at Dakar’s hemophilia treatment center every 4 months. They are received in emergency when they have bleeding.
An inhibitor screening was done when the number of days of exposure to FVIII concentrates reaches 30 days by the Bethesda method. The tests were performed using reagents from Diagnostica Stago (Asnieres, France). None of haemophiliacs had prophylactic treatment.
All uncircumcised hemophiliacs since 2010 were registered and selection of patients was done according to their order of listing. There was no selection criteria based on age, severity of hemophilia, the presence or absence of inhibitors.
This prospective study was conducted at Dakar’s Hemophilia Treatment Center where hemophiliacs are followed. Data were registered in the medical chart, including for each haemophiliac, the treatment history by FVIII concentrates and cumulative number of exposure days to anti hemophilic treatment. Circumcision was realized in the pediatric surgery department of Albert Royer Hospital for infants and in another medical center for adults.
Haemophiliacs and their parents were informed of the organization of a circumcision session through the Senegalese Association of Hemophiliacs. An informed consent form has been signed by patients or their parent if they are under 18 years old.
Medical treatment protocol
The substitutive treatment by FVIII concentrates was as follow: each patient had received 30 IU/kg of FVIII concentrates one hour before surgery. This dose was repeated systematically every 24 h for 48 h. An additional dose was given during occurrence of a persistent bleeding despite compressive dressing with tranexamic acid. Recombinant FVIII concentrates (Refacto or Recombinate) were used for haemophiliacs without anti FVIII inhibitors and bypassing factors such as factor eight inhibitor bypass activity (FEIBA) or activated recombinant factor VII (rFVIIa) for haemophiliacs with inhibitors. FEIBA was used at 80 IU/kg for the first three doses and rFVIIa at a dose of 90 μg/kg every 3 h and intravenous bolus when hemophiliacs had bleeding.
Tranexamic acid (Exacyl®) was administered at 20 mg/kg every 12 h by direct intravenously for three days, and local application during dressings.
Oxacillin (Bristopen®) was administered orally of 50 mg/kg/day for 10 days. An analgesic level one (paracetamol) was administered orally of 15 mg/kg every 6 h in children and 500 mg to 1 g every 8 h for adult if required.
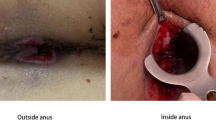
Surgery protocol
Haemophiliac is placed in dorsal recumbency position. After skin disinfection with iodine polyvydone, the pubic symphysis is identified and traction is exerted on the penis.
Local anesthesia is carried out with lidocaïne 1% with a total dose of 2 mg/Kg observed before 5 min after injection. The injection is administered either side of the median line, into under pubis space at 10 and 2 o’clock compared to the root of the penis halfway between the summit of the two folds drew on the penis and lower edge of pubis.
This penile block is completed by subcutaneous anesthesia wreath at the base of the penis. After capping and carefully cleaning the smegma, surgeon carries out an identification of the level of skin section up to the base of the glans through the Kocher clamp. This is then placed perpendicularly to the shaft of the penis after having assured the absence of the glans by bidigital palpation.
A circular cross section of the skin is made at a cold blade then hemostasis using electrocautery is made. The Kocher clamp is placed after dissection at the level of mucosal sheet about 2 mm below the level of skin section and then cut at the cold blade.
The surgeon carries out an additional hemostasis using electrocautery followed by dermo-epidermal sutures using Vicryl wire. After soapy polyvydone toilet and drying with ether, surgeon applies a compressive bandage for 24 h with a swab containing iodized polyvydone wrapped around the glans. Removal of the dressing was made at the first postoperative day. The sore is left open to the air and eosin 2% was applied twice a day.
Clinical evaluation
The outcome measures were: number of hospital days, number of exposure days to FVIII concentrates, healing time and occurrence of bleeding events.
Healing time is defined by the period from the beginning of circumcision to healing. Bleeding event is any haemorrhage that occurs since the release of hemophiliacs in the operating room until healed.
Externally, hemophiliacs were consulted at the hemophilia treatment center twice a week for two weeks then once a week until healed. Control of inhibitors was done in all hemophiliacs after healing.
Statistical analysis
Data collection was done according to a survey sheet. Data was entered into the computer with Epi info version 6 and analyzed with statistical analysis system (SAS). Descriptive analysis was realized with a quantitative study and a qualitative study. Bivariate analysis was carried out by comparing the proportion of two qualitative variables using chi-square test and the comparison of the means by Student’s t test. These tests were performed according to their condition of applicability and significance p (probability of error) was fixed: p ≤ 0.05.
Results
Characteristics of the study population
There were 26 patients with hemophilia A who underwent circumcision included in this study.
Median age was 7.5 years (range 1–30 years); 4 haemophiliacs (15.3%) were aged over 20 years. According to the severity, 8 haemophiliacs (30.8%) had a severe form, 9 patients (34.6%) had a moderate form and 9 patients (34.6%) had a mild form.
Twenty five patients (96%) had been previously treated with FVIII concentrates but only six patients (24%) had more than 10 exposure days to FVIII concentrates.
Four patients (15.3%) had anti FVIII inhibitors. They had low titer inhibitor between 1.5 and 3.8 BU/ml (Table 1).
Clinical evaluation
Mean number of days of FVIII concentrates treatment was 6.9 days (5–12 days) in children and 10.75 days (7–16 days) in adults (p = 0.0049). Mean number of days of hospitalization was 3.68 days (2–10 days) in children and 13.5 days (13–15 days) in adults (P < 0.001). Mean healing time was 26.47 days (20–35 days) in children and 25.25 days (22–30 days) in adults (p = 0.697).
Bleeding events occurred among five haemophiliacs (19.2%). Bleeding occurred spontaneously in one patient who had anti factor VIII inhibitors or during dressings in four patients. In patients without inhibitors, tranexamic acid helped to stop bleeding while in patients with inhibitor, rFVIIa was used to stop bleeding.
We noted that severe haemophiliacs were most exposed to treatment with a higher number of days of hospitalization and a prolonged healing time. Similarly, they had more bleeding events (Table 2).
Characteristics of haemophiliacs with bleeding events
Five haemophiliacs (19.2%) presented bleeding events. This was four severe haemophiliacs and one moderate haemophiliac. Among them, three severe haemophiliacs had developed anti FVIII inhibitors. Mean age of these patients was 15.2 years (6–30 years). Mean number of days of hospitalization was 11.2 days (6–15 days) and mean number of days of treatment was 9.2 days (5–14 days). Mean healing time was 28 days (22–35 days) (Table 3).
Number of doses and total quantity of factor concentrates administered
Total quantity of FVIII concentrates administered was 38350 IU, soit 58.1 IU/kg per patient. Mean dose per patient was 1743 IU (810–2340); 12 haemophiliacs received Refacto (21160 IU) and 10 haemophiliacs received Recombinate (17190 IU) (Table 4)
Total quantity of FEIBA administered was 22320 IU and mean dose per patient was 5580 IU (2640–10800).
Total quantity of rFVIIa was 1656 μg and mean dose per patient was 414 μg (66–810). All haemophiliacs with inhibitors received FEIBA during the first three doses followed by rFVIIa in case of bleeding.
Discussion
Circumcision in hemophilia is a delicate surgery because of bleeding risks. These bleedings can be prevented through proper supplementation of clotting factor concentrates, explaining the challenges in countries where substitutive treatment is not always available. It is demonstrated that using high quantity of factor concentrates in surgery in hemophilia is associated with inhibitor development whose management is more difficult because of using more costly treatments [19].
This study used low quantity of anti FVIII concentrates associated with antifibrinolytic treatment. It aims to reduce the risk of severe bleeding and the risk of developing anti FVIII inhibitors. Substitution therapy in our study consisted to raise FVIII levels around 60% for three days. An additional dose levels is systematically performed in serious bleeding events resistant to local hemostasis with tranexamic acid.
All hemophiliacs received only three doses systematically for increasing the factor level to 60% for three days. The amount of factor concentrates used in our study is less important than those used in Turkish and Moroccan studies [14, 15].
The effectiveness of this protocol was evaluated by comparing our results with those of circumcision in non-hemophiliac population. The criteria of comparison were based on the number of days of exposure to anti FVIII concentrates, the number of hospital days, the healing delay and bleeding complications.
The prolonged healing time in our patients may be explained by the high number of hemophiliacs aged over 15 years. More shortened recovery periods have been described in some studies but these studies were performed in hemophiliacs children aged less than 10 years [20].
Bleeding complications were noted in 19.2% of patients. This result is comparable to hemorrhagic complications of circumcision performed in healthy subjects whose prevalence of bleeding events is estimated between 10 and 35% [21, 22].
Many types of alternative protocols was used in various studies [14, 23, 24]. Al these protocols have the same objectives to reduce or prevent bleeding events of circumcision. These studies show that the absence or decrease in risk of bleeding was not linked to the use of high doses of anti FVIII concentrates but to the number of exposure days to antihemophilic treatment. All studies that have associated tranexamic acid and fibrin glue to strengthen local hemostasis results to a less occurrence of bleeding events [14, 24, 25]. Reduction of bleeding complications during hemophiliac’s circumcision is not only related to the use of large quantities of anti hemophilic factor. Other factors including antifibrinolytic treatment, good local hemostasis using electrocautery and the practice of circumcision by an experienced surgeon [26,27,28] are also implicated. The nursing staff must be qualified in the field of hemophilia management because most bleeding is post traumatic during the dressing [29].
Other surgical devices are newly used for proper local hemostasis such as diathermic knife which has reduced the need for anti FVIII treatment and the cost of circumcision [30].
According to age, it is proven that circumcision performed in newborns and children is easier, less grave and causes fewer complications compared to adults [31] whereas healing is more difficult and prolonged than in adults [32]. This can explain why circumcision is rarely practiced in adults except in hemophilia where circumcision is delayed if the anti hemophilic treatment is inaccessible.
Severe Hemophilia is associated with more morbidity with an upsurge in bleeding complications and a significant risk of inhibitor development. Hemophiliacs with inhibitors had more bleeding complications and a longer period to healing [33, 34].
Conclusion
We show through this study that it is possible to realize circumcision in haemophiliacs in a country with low resources, using low quantities of anti hemophilic factor concentrates. This protocol is adaptable to a country where hemophilia treatment is not available permanently.
References
Claude G. Hemophilia today. Kinesither Rev. 2009;88:32–6.
Boehlena F, Raddatz Müllera P, Brandc B, et al. Hémophilie dans la pratique du médecin de famille. Forum Med Suiss. 2011;11(26):452–7.
Kavakli K, Aledort LM. Circumcision and haemophilia: a perspective. Haemophilia. 1998;4(1):1–3.
Nathanson S. La circoncision : geste rituel et thérapeutique? Méd Enf. 2004;17:415–418.
Siev M, Keheila M, Motamedinia P, Smith A. Indications for adult circumcision: a contemporary analysis. Can J Urol. 2016;23(2):8204–8.
Ademuyiwa AO, Ojewola RW, Elebute OA, Jeje EA, Bode CO. Surgically correctable morbidity from male circumcision: indications for specialist surgical care in lagos. Niger J Surg. 2012;18(2):71–4.
Sahay S, Nagarajan K, Mehendale S, Deb S, Gupta A, Bharat S, et al. Community and healthcare providers’ perspectives on male circumcision: a multi-centric qualitative study in India. PLoS One. 2014;9(3):912–3.
Hromadko M, Fatović-Ferencić S. Circumcision: cultural entity and medical controversy. Lijec Vjesn. 2007;129(6–7):241–6.
Moslemi MK, Abedinzadeh M, Aghaali M. Evaluation of epidemiology, safety, and complications of male circumcision using conventional dissection surgery: experience at one center. Open Access J Urol. 2011;3:83–7.
Elalfy MS, Elbarbary NS, Eldebeiky MS, El Danasoury AS. Risk of bleeding and inhibitor development after circumcision of previously untreated or minimally treated severe hemophilia A children. Pediatr Hematol Oncol. 2012;29(5):485–93.
Sasmaz I, Antmen B, Leblebisatan G, Şahin Karagün B, Kilinç Y, Tuncer R. Circumcision and complications in patients with haemophilia in southern part of Turkey: Çukurova experience. Haemophilia. 2012;18(3):426–30.
Paranthaman K, Bagaria J, O’Moore E. The need for commissioning circumcision services for non-therapeutic indications in the NHS: lessons from an incident investigation in Oxford. J Public Health (Oxf). 2011;33(2):280–3.
Perera CL, Bridgewater FH, Thavaneswaran P, Maddern GJ. Safety and efficacy of nontherapeutic male circumcision: a systematic review. Ann Fam Med. 2010;8(1):64–72.
Yilmaz D, Akin M, Ay Y, Balcan C, Celik A, Erqun O, et al. A single centre experience in circumcision of haemophilia patients: Izmir protocol. Haemophilia. 2010;16(6):888–91.
Nafil H, Tazi I, Mahmal L. Circumcision in patients with hemophilia A in the Marrakech region (Morocco)]. Med Sante Trop. 2013;23(1):111–2.
Haghpanah S, Ardeshiri R, Zahedi Z, Golzadeh MH, Silavizadeh S, Karimi M. Attitudes and practices with regard to circumcision in haemophilia patients in Southern Iran. Haemophilia. 2013;19(3):177–8.
Diop S, Seck M, Sy-Bah D, Faye BF, Sow-Ndoye A, Gueye YB, et al. Implementing haemophilia care in Senegal, West Africa. Haemophilia. 2014;20(1):73–7.
The World Federation of Hemophilia’s Sixth Global Forum. On the Safety and Supply of Treatment Products for Bleeding Disorders. September 24–25, 2009, Montreal, Canada. Consulted October 3, 2016. www.wfh.org
Shima M, Lillicrap D, Kruse-Jarres R. Alternative therapies for the management of inhibitors. Haemophilia. 2016;22(5):36–41.
Kearney S, Sharathkumar A, Rodriguez V, Chitlur M, Valentino L, Boggio L, et al. Neonatal circumcision in severe haemophilia: a survey of paediatric haematologists at United States Hemophilia Treatment Centers. Haemophilia. 2015;21(1):52–7.
Galukande M, Kahendehe C, Buuza E, Sekavuga DB. A rare but important adverse event associated with adult voluntary medical male circumcision: prolonged bleeding. Int J Emerg Med. 2015;8:8.
Joseph A. Circumcision. Br J Gen Pract. 2010;60(572):214–5.
Rodriguez V, Titapiwatanakun R, Moir C, Schmidt KA, Pruthi RK. To circumcise or not to circumcise?Circumcision in patients with bleeding disorders. Haemophilia. 2010;16:272–6.
Avanogmacr lu A, Celik A, Ulman I, Ozcan C, Kavakli K, Nişli G, et al. Safer circumcision in patients with haemophilia: the use of fibrin glue for local haemostasis. BJU Int. 1999;83(1):91–4.
Tazi I. Fibrin glue, hemophilia, and circumcision in low-income countries. J Pediatr Surg. 2011;46(2):428–9.
Hutcheson JC. Male neonatal circumcision: indications, controversies and complications. Urol Clin North Am. 2004;31(3):461–7.
Moosa FA, Khan FW, Rao MH. Comparison of complications of circumcision by « Plastibell device technique » in male neonates and infants. J Pack Med Assoc. 2010;60(8):664–7.
Senel FM, Demirelli M, Pekcan H. Mass circumcision with a novel plastic clamp technique. Urology. 2011;78(1):174–9.
Lujan M, Gamarra M, Mora JR, Lopez MC, Pascual C, Martin C, et al. Outpatient urologic surgery office conducted by nursing staff. A process integrated in a total quality strategy. Arch Esp Urol. 2013;66(9):841–50.
Karaman MI, Zulfikar B, Ozturk MI, Koca O, Akyüz M, Bezgal F. Circumcision in bleeding disorders: improvement of our cost effective method with diathermic knife. Urol J. 2014;11(2):1406–10.
Weiss HA, Larke N, Halperin D, Schenker I. Complications of circumcision in male neonates, infants and children : a systematic rewiew. BMC Urol. 2010;10(1):2–3.
Shittu OB, Shokunbi WA. Circumcision in haemophiliacs: The Nigerian experience. Haemophilia. 2001;7:534–6.
Leblebisatan G, Saşmaz I, Antmen B, Klnç Y, Aridoğan IA. Serial urological interventions including circumcision in a hemophilic child with inhibitors. Blood Coagul Fibrinolysis. 2011;22(6):547–8.
Balkan C, Karapinar D, Aydogdu S, Ozcan C, Ay Y, Akin M, et al. Surgery in patients with haemophilia and high responding inhibitors: Izmir experience. Haemophilia. 2010;16(6):902–9.
Acknowledgements
We thank the members of Hemophiliacs Association of Senegal, the pediatric surgery staff of Albert Royer hospital and the staff of Dakar hemophilia treatment center.
Funding
No funding was available for this study.
Availability of data and materials
Data analyzed in this study are available from the corresponding author on request.
Authors’ contributions
MS: Study design, medical protocol drafting, data analyzes, article drafting. AS: Surgical protocol drafting, realization of circumcision, reading and correction of the final version of the article. MSG: Hemostasis tests, Collecting and analyzing data, reading and correction of the final version of the article. BFF: Article drafting, reading and correction of the final version of the article. DS: Hemostasis tests, medical protocol drafting, reading and correction of the final version of the article. SAT: Article drafting, reading and correction of the final version of the article. AS: Drafting, reading and correction of the final version of the article. AOT: Reading and correction of the final version of the article. SD: Study design, medical protocol drafting, correction of the final version. All authors read and approved the final manuscript.
Authors’ information
MS: Assistant of clinical hematology, Cheikh Anta Diop University of Dakar, Senegal.
AS: Assistant of pediatric surgery, Cheikh Anta Diop University of Dakar, Senegal.
MSG: Student in thesis year, Cheikh Anta Diop University of Dakar, Senegal.
BFF: Assistant of clinical hematology, Cheikh Anta Diop University of Dakar, Senegal.
DS: Specialist in clinical haemostasis at Dakar Hemophilia Treatment Center.
SAT: Doctor at Dakar Hemophilia Treatment Center.
AS: Assistant of biological hematology, Cheikh Anta Diop University of Dakar, Senegal.
AOT: Professor of biological hematology, Cheikh Anta Diop University of Dakar, Senegal.
SD: Professor of clinical hematology, Cheikh Anta Diop University of Dakar, Senegal.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Not applicable.
Ethics approval and consent to participate
This study was approved by the National Ethics Committee for Health Research in Senegal (Reference: Protocol 0230/2017/CER/UCAD). An informed consent form has been signed by each parent for minors or by the adult hemophiliacs before the start of the study.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Seck, M., Sagna, A., Guéye, M.S. et al. Circumcision in hemophilia using low quantity of factor concentrates: experience from Dakar, Senegal. BMC Hematol 17, 8 (2017). https://doi.org/10.1186/s12878-017-0080-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12878-017-0080-1