Abstract
Introduction
In 2016, the Chinese government officially scaled up family doctor contracted services (FDCS) scheme to guide patients’ health seeking behavior from tertiary hospitals to primary health facilities.
Methods
This study evaluated the overall gate-keeping effects of this scheme on healthcare utilization of rural residents by using a difference-in-differences (DiD) design. The analysis was based on Shandong Rural Elderly Health Cohort 2019 and 2020. Participants who contracted FDCS in second round and were not contracted with a family doctor in the first round were regarded as treatment group. In total, 310 respondents who have used medical care were incorporated for final study.
Results
Participants who contracted FDCS (treatment group) experienced a significant decline in the mean level of first-contact health-care facilities, decreasing from 2.204 to 1.981. In contrast, participants who did not contract FDCS (control group), showed an increasing trend in the mean level of first-contact health-care facilities, rising from 2.128 to 2.445. Our results showed that contracting FDCS is associated with approximately 0.54 extra lower mean level of first-contact health-care facilities (P = 0.03, 95% CI: -1.03 to 0.05), which suggests an approximately 24.5% reduction in the mean first-contact health-care facility level for participants compared with contracted FDCS than those who did not.
Conclusions
The study suggested primary healthcare quality should be strengthened and restrictive first point of contact policy should be enacted to establish ordered healthcare seeking behavior among rural residents.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Introduction
Enhancing the accessibility and affordability of health care ranks a top priority to reach universal health coverage (UHC) and is central to the Chinese health agenda [1,2,3]. Family doctors have been proved to be effective in gate-keeping secondary health-care utilization, as well as contributing to patient health by offering better accessibility, continuity, and comprehensive care [4, 5]. Having a regular family doctor has been suggested to improve the overall wellbeing [6]. However, China’s health system has encountered pronounced challenges of medical expenditure escalation and maldistribution of health-care resources among primary and secondary health-care facilities [7]. Moreover, residents were unrestricted to access to hospitals which led to patients increasingly bypass primary health care centers (PHCs) and went to tertiary hospitals [8, 9]. This further worsen the accessibility and continuity of essential health-care and intensify the unbalanced distribution of medical resources [10].
Starting from 2006, family doctor scheme has been introduced and piloted by Chinese government in several megacities of China, with the vision to strengthen primary health care as well as forge a hierarchical medical system [11]. In 2016, the Chinese government officially scaled up family doctor contracted services (FDCS) scheme across the country, as a means to guide residents’ health seeking behavior by providing comprehensive, continued, preventive health management, and eventually improve primary health care quality [12]. Under this guideline, family doctors are contracted to provide essential medical services, public health services, and individualized health management to contracted residents [13, 14]. This gatekeeping policy is proposed to channel residents to their family doctors as their first point of contact [13]. In addition, government put forward a series of programs to guarantee and better the quality of health care provided by family doctors, including adjusting benefit packages to optimize individualized health management for older adults and residents with chronic diseases, investing enormously to strengthen the capacity of PHCs, and incentivize utilization of family doctor services by health insurance reimbursement policy [15].
Investigating the impact of family doctors on health care users’ behaviors is important. There is now a considerable international study indicated that family doctors have significant effects on residents’ health care utilization, heath behaviors, and health outcomes [16,17,18,19]. In terms of gatekeeping effect, extending working hours of family physicians would reduce emergency department service utilization [20]. Family doctors have been proved to play a more important role in mobilizing population to utilize preventative services [17]. Additionally, free and universal general practice has been demonstrated to enhance psychological health of older adults as well as facilitating access to primary services [21, 22]. However, empirical research on the impact of FDCS on health care utilization in rural China is less common, and the evidence drown from theses research is mixed. A series studies conducted in urban cities suggested that contracted residents have higher proportion of primary visits than non-contractors, so family doctors may improve willingness to visit PHCs as their first contact [23, 24]. However, the effects of FDCS for rural residents was ambiguous, as the role of family doctors on gatekeeping rural residents has been reported insignificant [25, 26].
To date, previous research on the assessment of FDCS policy has been concentrated on cross-sectional analysis conducted in community health care, and there has been comparatively little research on the rural residents. In this study, we extend these analyses, applying a quasi-experimental design, difference-in-differences (DiD), to exam the impact of the introduction of FDCS policy on the gate-keeping effects in healthcare utilization [27]. Focusing on the core vision of FDCS policy, and taking the various auxiliary policy into account, we provided a crucial analysis on the current patterns of healthcare utilization and highlighting the extent to which the policy leads to barriers of gatekeeping effects. We inform policymakers whether current FDCS have been effective to attract contracted residents’ preference to primary health facilities and better health behaviors.
Methods
Data collection
Data were collected from one cohort study conducted in rural Shandong province of east China from the period May 2019 to August 2020. The first round of the Shandong Rural Elderly Health Cohort (SREHC) was performed in May 2019, and the second round of this study was performed in August 2020. Information including socio-economics status, physical and mental health, health behaviors of the older adults aged over 60 was collected through face-to-face surveys.
The study participants were selected using a stratified multi-stage sampling method. Firstly, we have randomly selected three cities according to GDP per capita, geographic locations, and medical resource distributions. The three study cities were Ru Shan city (east Shandong, with a medium high level of GDP per capita), Qu Fu city (west Shandong, with a medium level of GDP per capita), and Lao Ling city (north Shandong, with a low level of GDP per capita). Moreover, the distribution of medical resources was also considered among these cities. The number of health care institutions across different levels and number of medical personnel per thousand people in the three study cities are shown in figure S2 and figure S3 (see supplementary figure file). Rushan city has the highest total number of health institutions, hospitals, and primary health institutions. As shown in figure S3, Laoling city has the lowest number of beds, licensed doctors, and registered doctors per thousand people among the three study cities, and also lower than Shandong province. Whereas Qufu city and Rushan city outperform Shandong province. Rushan city has the highest licensed doctors and registered nurses per thousand people among the three study cities. Therefore, we believe the study cities are representative of Shandong province. Next, 5 townships were randomly selected in each county and 4 villages were selected within each township. Finally, 60 older adults in each village were randomly recruited as study participant in the baseline survey.
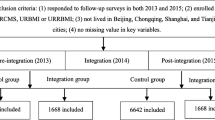
The sample selection process was shown in Fig. 1. There were 3243 participants recruited in the first wave of this study in 2019. The exclusion criterion was as follows: (1) excluded 458 participants who have not completed the survey in the follow-up study during the period of August to September of 2020; (2) excluded 1495 participants who have enrolled in FDCS schemes; (3) excluded 933 participants and 47 participants who did not use 2-week medical services in 2019 and 2020 surveys respectively. Finally, a total of 310 participants were analyzed in the final study, with 191 participants in the treatment group and 119 participants in the control group. All respondents were fully informed with written informed consent for participation prior to the face-to-face interview. Ethical approval was granted by the Ethical Committee of Shandong University School of Public Health (No. 20,181,228). The Declaration of Helsinki was followed in all measurements.
Variables
We evaluated the FDCS policy effects by measuring the average levels of health-care facility if the participants used 2-week medical care. Each participant was asked “Did you see doctors in the past two weeks when you sick?” and “which health-care facility did you go to as first-contact?” The health-care facilities were divided into 5 categories and scored as “1 = village clinics, 2 = township hospitals, 3 = county hospitals, 4 = prefecture hospitals, 5 = provincial hospitals”. We calculated this attribute by taking average of the level of health-care facility of patient first-contact. The lower of the average score indicate more utilization of primary health-care resources.
The confounding variables we have adjusted were as follows: sex, age, household income, educational attainment, marital status, health behaviors variables including smoking status, alcohol drinking status, and health conditions. Moreover, the distance to the nearest medical service institution was also adjusted. This variable was categorized into two levels and scored as “0 = Less than 1KM, 1 = More than 1KM”.
Statistical analysis
Our methodological framework was a difference-in-differences design which compares the difference in average level of health care facilities for first contact of rural residents. A key challenge in evaluating the impact of the FDCS is that because this policy was implemented across the whole country, and all residents were subject to the policy. To select a plausible “treatment group” of residents, we treat the residents who were not contracted FDCS at the baseline but contracted FDCS in the second wave as the treatment group. And the residents who were not contracted FDCS both in the two waves as the control group (Fig. 1). It is assumed that before registered a family doctor, the residents in control group and treatment group were comparable in terms of health-care seeking behavior. Therefore, we can conclude the differences of healthcare seeking behavior were due to the implementation of FDCS. We made the following assumptions, contracted residents are more likely to go to see family doctors as their first-contact, and the health behaviors of contracted residents should be enhanced due to health care management provided by family doctors.
We calculated the causal effects of contracted family doctor services by applying the following difference-in-differences analysis equation:
Where \(\:{Y}_{ijk}\) is the average facility level of the first-contact, \(\:{Treat}_{i}\) denotes whether the interviewed participant has enrolled in family doctor contracted service plans, \(\:{Post}_{ij}\) indicate the survey round, the interaction term \(\:{Treat}_{i}\times\:{Post}_{ij}\) represents the difference in the health care facility levels of first-contact changes before and after contracted with family doctors, \(\:{X}_{ijk}\) indicates the confounding variables. We estimated \(\:{\beta\:}_{3}\) which indicates the difference of first-contact health-care facility levels.
To address selection bias and ensure the treatment group and control group were balanced, we calculated inverse probability weights (IPWs) and applied to each variable. As figure S1 shown, the standardized differences across all variables were less than 0.1, suggesting the control group and treatment group are balanced. Sensitivity analysis was performed by applying weighted variables to model estimation. The statistical analyses were undertaken in STATA v14.2.
Results
Description of the study population
As shown in Table 1, the majority of participants of both uncontracted and contracted group were female, with the average age over 68. The average household income in the control group was RMB 9411.21 which was higher than in the treatment group (RMB 7562.78). With respect to educational attainment, around 80% of the respondents were with low literacy level. The percentage of widowed or divorced residents was 25.21% in control group and was lower than in the treatment group (30.37%). In terms of living habits, 19.90% of the respondents in treatment group were current smokers, and the percentage of current smokers was higher than that of control group (12.61). The percentage of current acholic drinker was 14.29% in control group and was smaller than in treatment group (17.89%). Most of the respondents had chronic diseases, and the percentages were 83.19% and 82.72% in two groups. There was no significant difference between the two groups with respect to level of first-contact. The average level of first-contact in control group was 1.61 which was higher than the treatment group (1.41). The percentage of participants who choose village clinics as their first-contact health institution among treatment group is higher (80%) than among control group (68%). This may suggest that comparing with people who do not contract FDCS, residents who contracted FDCS were more prone to primary health facilities as their first contact.
Figure 2 presents visual trends in the average level of first-contact health facility among participants with contracted FDCS and not contracted FDCS, showing changes from not contract to contract FDCS. After controlling for age, sex, education, marital status, smoking status, alcohol drinking status, chronic conditions, and distance to the nearest health facility, we examined the effects of contracting family doctors on the mean facility level of first-contact. As shown in Fig. 2, participants who contracted FDCS (treatment group) experienced a significant decline in the mean level of first-contact health-care facilities, decreasing from 2.204 to 1.981. In contrast, participants who did not contract FDCS (control group), showed an increasing trend in the mean level of first-contact health-care facilities, rising from 2.128 to 2.445.
The impact of the FDCS policy on the healthcare facility levels of first-contact is provided in Table 2. The results showed that contracting FDCS is associated with approximately 0.54 extra lower mean level of first-contact health-care facilities (P = 0.03, 95% CI: -1.03 to 0.05). This finding suggests an approximately 24.5% reduction in the mean first-contact health-care facility level for participants compared with contracted FDCS than those who did not. Moreover, we observed that the distance to the nearest health facility associated with first-contact health institution levels. Particularly, participants with more than 1KM distance to the nearest health facility were associated with higher level of first-contact health facilities (β = 0.49, 95% CI: 0.09 to 0.88) than the reference group.
Discussion
In this study, we examined the impact of contracting a family doctor on healthcare seeking behavior of rural residents. The results indicated that implementation of FDCS have notably resulted in a reduction in the healthcare facility levels for first contact. In contrast to the pre-period and control group, there is a downward trend in the average level of health-care facility for first-contact, which indicates that participants who have contracted with family doctors are more likely to seek health care at primary facilities.
With respect to the gatekeeping effects of FDCS, our findings revealed the similar evidence with previous reports. In line with studies conducted in Hong Kong and Shanghai, urban residents contracted with a family doctor were more likely to utilize PHCs services as their first-contact, which suggested that family doctor-led primary care model was most effective in gate-keeping secondary care [28, 29]. As another cross-sectional study demonstrated, rural residents value accessibility most for seeking medication [30]. Therefore, rural residents with minor illness were prone to visit family doctors in village clinics since PHCs were more accessible, and they had close relationship with barefoot doctors. These might be the potential reasons to explain the significant downward trend in health care facility levels in rural areas.
Although the average level of first contact healthcare facility was significantly lower among treatment group, i.e., contracted family doctor group, than that of the control group, there were still instances of bypassing village clinics and going directly to higher-level institutions for the first contact. One possible explanation is that FDCS had only been implemented for three years and was still in the early stages. Contracted participants may not have been fully aware of the services as well as the benefit packages, which decrease the willingness to use FDCSs [31]. Therefore, the impact of FDCS on healthcare utilization might be underestimated. Another explanation might be the disparity in medical quality between village clinics and higher-level medical institutions in China [32, 33]. Due to a lack of trust in the competency of family doctors in village clinics, rural older adults might bypass their family doctors and seek care at higher-level medical institutions for high-quality services [34]. Previous studies also suggested that those rural patients with chronic diseases and high educational attainment are more likely to bypass primary care since they have higher medical demand and can afford high-quality medical services [35]. Therefore, Narrowing the gap in medical service levels between primary healthcare institutions and higher-level medical institutions, such as by equipping primary institutions with more well-trained healthcare personnel and improving the treatment environment, may be helpful [36].
Unfortunately, there was no strong evidence that hierarchical medical seeking order had been formalized with the enactment of FDCSs. Especially in the initial stage, there was no restriction on medical seeking behavior. The Chinese people enjoyed direct access to outpatient services provided by specialized doctors without referral from a family doctor. Similar findings have been demonstrated by other studies [37]. Furthermore, literatures demonstrated that health insurance as financial incentive to increase primary care utilization by cost sharing, and the use of capitation payment was also proven to significantly encourage family doctors to become health managers and gatekeepers [38]. However, these strategies have not been fully addressed and incorporated in FDCSs benefit packages which might limited health utilization and provision of services.
This study presents meaningful results in search of an optimal policy design to facilitate implementation of the family doctor contracted services policy. Several implications can be proposed. First, to enforce the gatekeeping role of family doctors, policies should be initiated to restrict first contact within the health system. Under this gatekeeping policy, patients need to be referred by a family doctor to seek specialist care rather than self-referred. Second, benefit packages should be tailored to meet the health need of rural residents- e.g. medical insurance incentives should be established to improve primary health utilization by increasing reimbursement subsidies and lowering their copayments. Finally, the government should strengthen primary healthcare system to enhance the quality of primary care. Comprehensive policies and incentives should be considered and adjusted to reconstruct health networks between primary and tertiary hospitals, so as to establish integrated and continued health care system.
This study had several limitations and should be taken into consideration in the future study. First, this study only captured the short-term effect of FDCS, as the policy had been fully implemented for only three years. Future study should investigate the long-term effect of FDCS. Second, since majority of the participants have enrolled in FDCS in the baseline study in 2019, they were excluded from final analysis. Moreover, we measured medical utilization using 2-week hospital visit, and because the prevalence rate was low within two weeks, this constraint led to a relatively small sample size.
Consequently, comprehensive indexes reflecting primary health care quality, including medication adherence, medical expenditure, and referrals should be added in the future analysis to evaluate impact of FDCS implementation on outpatient service utilization.
Conclusion
Hierarchical medical seeking order and primary healthcare should be promoted. This present study evaluated the impacts of FDCS implementation on healthcare utilization and health behaviors in rural China. The first assessment study suggested that the enrolment of FDCS led to significant downward trend of healthcare facility levels for first contact, but did not reduce the actual healthcare facility level. We suspected this mighty have been because the implementation of FDCS was at its first stage. Hence, restrictions on referral system should be introduced to encourage family doctors became gatekeepers on health management and health behavior, and a more comprehensive approach to enhance primary healthcare quality also need to be addressed.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author (Prof. Chengchao Zhou) on reasonable request.
References
Tao WJ, Zeng Z, Dang HX, Lu BQ, Chuong L, Yue DH et al. Towards universal health coverage: lessons from 10 years of healthcare reform in China. Bmj Glob Health. 2020;5(3). DOI: ARTN e00208610.1136/bmjgh-2019-002086. [PMID: WOS:000527713300012].
Liu X, Wang Z, Zhang H, Meng Q. Measuring and evaluating progress towards Universal Health Coverage in China. J Global Health. 2021;11:08005. https://doi.org/10.7189/jogh.11.08005. [PMID: 33981413].
Zhou Y, Li C, Wang M, Xu S, Wang L, Hu J, et al. Universal health coverage in China: a serial national cross-sectional study of surveys from 2003 to 2018. Lancet Public Health. 2022;7(12):e1051–63. https://doi.org/10.1016/S2468-2667(22)00251-1. [PMID: 36462516].
Schafer WLA, Boerma WGW, Schellevis FG, Groenewegen PP. GP practices as a one-stop shop: how do patients perceive the quality of care? A cross-sectional study in thirty-four countries. Health Serv Res. 2018;53(4):2047–63. https://doi.org/10.1111/1475-6773.12754. [PMID: WOS:000439548300004].
Li H, Liu K, Gu J, Zhang Y, Qiao Y, Sun X. The development and impact of primary health care in China from 1949 to 2015: a focused review. Int J Health Plann Manage. 2017;32(3):339–50. https://doi.org/10.1002/hpm.2435. [PMID: 28670754].
Bataineh H, Devlin RA, Barham V. Social capital and having a regular family doctor: evidence from longitudinal data. Soc Sci Med. 2019;220:421–9. https://doi.org/10.1016/j.socscimed.2018.12.003. [PMID: WOS:000456222400046].
Li X, Lu JP, Hu S, Cheng KK, De Maeseneer J, Meng QY, et al. The primary health-care system in China. Lancet. 2017;390(10112):2584–94. https://doi.org/10.1016/S0140-6736(17)33109-4. [PMID: WOS:000417493300027].
Xiao YX, Chen X, Li Q, Jia PF, Li LN, Chen ZF. Towards healthy China 2030: modeling health care accessibility with patient referral. Soc Sci Med. 2021;276:113834. DOI: ARTN 11383410.1016/j.socscimed.2021.113834. [PMID: WOS:000697111600012].
Rao S, Xue H, Teuwen DE, Shi H, Yi H. Measurements of quality of village-level care and patients’ healthcare-seeking behaviors in rural China. BMC Public Health. 2021;21(1):1873. https://doi.org/10.1186/s12889-021-11946-8. [PMID: 34657604].
Liu C, Qiu L, Wang H. Willingness rate of the first visit to primary healthcare services and the associated factors in China: a meta-analysis. Aust J Prim Health. 2022;28:459–68. https://doi.org/10.1071/PY21296. [PMID: 35858635].
The Central People’s Government of the People’s Republic of China. Opinions on developing community health care 2006 Available: http://www.gov.cn/zwgk/2006-02/23/content_208882.htm. Accessed: 8 December 2022.
National Health and Family Planning Commission. Guidline on promoting familiy doctor contract service 2016 Available: http://www.gov.cn/zhengce/zhengceku/2018-12/31/content_5435461.htm. Accessed: 23 November 2022.
National Health Commission of the People’s Republic of China. Opinions on implementation of family doctor contracted services policy 2019 Available: http://www.nhc.gov.cn/jws/s7881/201904/4cb8d9c938fd4ec08cba94bd92f64fcf.shtml. Accessed: 16 January 2023.
State Council of the People’s Republic of China. Guidance on regulating the implementation of family doctor contracted services 2018 Available: http://www.gov.cn/zhengce/zhengceku/2018-12/31/content_5435461.htm. Accessed: 16 December 2022.
National Health Commission of the People’s Republic of China. Opinions on promoting family doctor contracted services quality 2022 Available: http://www.nhc.gov.cn/jws/s7882/202203/060ecf9a84af443aa349d447c4dfdd31.shtml. Accessed: 12 November 2022.
Bischof T, Kaiser B. Who cares when you close down? The effects of primary care practice closures on patients. Health Econ. 2021;30(9):2004–25. https://doi.org/10.1002/hec.4287. [PMID: WOS:000655241300001].
Gyulai A, Nagy A, Pataki V, Tonte D, Adany R, Voko Z. General practitioners can increase participation in cervical cancer screening - a model program in Hungary. Bmc Family Practice. 2018;19. DOI: ARTN 6710.1186/s12875-018-0755-0. [PMID: WOS:000433242800001].
Tzartzas K, Oberhauser PN, Marion-Veyron R, Bourquin C, Senn N, Stiefel F. General practitioners referring patients to specialists in tertiary healthcare: a qualitative study. BMC Fam Pract. 2019;20(1):165. https://doi.org/10.1186/s12875-019-1053-1. [PMID: 31787078].
Wang C, Yan S, Jiang H, Nie Z, Miller M, He Y, et al. Residents’ willingness to maintain contracts with family doctors: a cross-sectional study in China. J Gen Intern Med. 2021;36(3):622–31. https://doi.org/10.1007/s11606-020-06306-y. [PMID: 33140279].
Dolton P, Pathania V. Can increased primary care access reduce demand for emergency care? Evidence from England’s 7-day GP opening. J Health Econ. 2016;49:193–208. https://doi.org/10.1016/j.jhealeco.2016.05.002. [PMID: WOS:000384869400015].
Ma YY, Nolan A, Smith JP. Free GP care and psychological health: quasi-experimental evidence from Ireland. J Health Econ. 2020;72:102351. DOI: ARTN 10235110.1016/j.jhealeco.2020.102351. [PMID: WOS:000552666400016].
Walsh B, Nolan A, Brick A, Keegan C. Did the expansion of free GP care impact demand for Emergency Department attendances? A difference-in-differences analysis. Soc Sci Med. 2019;222:101–11. https://doi.org/10.1016/j.socscimed.2018.12.029. [PMID: WOS:000459838900012].
Zheng QM, Shi L, Pang TT, Leung W. Utilization of community health care centers and family doctor contracts services among community residents: a community-based analysis in Shenzhen, China. Bmc Family Practice. 2021;22(1). DOI: ARTN 10010.1186/s12875-021-01444-6. [PMID: WOS:000653766200001].
Sun H, Lan K, Guo Y, Lin C, Zhang Y, Du Y. An empirical study on the impacts of family doctor contracting services on residents’medical treatment seeking behavior. Chin J Health Policy. 2020;13(3):44–8.
Zhou ZL, Zhao YX, Shen C, Lai S, Nawaz R, Gao JM. Evaluating the effect of hierarchical medical system on health seeking behavior: a difference-in-differences analysis in China. Soc Sci Med. 2021;268:113372. ARTN 113372.
1016/j. socscimed.2020.113372. [PMID: WOS:000604584500005].
Liao R, Liu YQ, Peng SZ, Feng XL. Factors affecting health care users’ first contact with primary health care facilities in north eastern China, 2008–2018. Bmj Glob Health. 2021;6(2). DOI: ARTN e00390710.1136/bmjgh-2020-003907. [PMID: WOS:000621258400003].
Dimick JB, Ryan AM. Methods for evaluating changes in Health Care Policy the difference-in-differences Approach. Jama-J Am Med Assoc. 2014;312(22):2401–2. https://doi.org/10.1001/jama.2014.16153. [PMID: WOS:000346345700015].
Fung CSC, Wong CKH, Fong DYT, Lee A, Lam CLK. Having a family doctor was associated with lower utilization of hospital-based health services. Bmc Health Serv Res. 2015;15. https://doi.org/10.1186/s12913-015-0705-7. [PMID: WOS:000348820500003].
Huang J, Liu Y, Zhang T, Wang L, Liu S, Liang H, Zhang Y, Chen G, Liu C. Can family doctor contracted services facilitate orderly visits in the referral system? A frontier policy study from Shanghai, China. Int J Health Plann Manag. 2022;37(1):403–16.
Hu X, Zhang H, Sun X, Gu Y, Zhen X, Gu S, et al. Older adults’ choices of first-contact care and related factors in Zhejiang and Qinghai Province, China. Geriatr Gerontol Int. 2019;19(9):938–44. https://doi.org/10.1111/ggi.13746. [PMID: 31342634].
Fu P, Wang Y, Liu S, Li J, Gao Q, Zhou C, et al. Analysing the preferences for family doctor contract services in rural China: a study using a discrete choice experiment. BMC Fam Pract. 2020;21(1):148. https://doi.org/10.1186/s12875-020-01223-9. [PMID: 32711467].
Li X, Krumholz HM, Yip W, Cheng KK, De Maeseneer J, Meng Q, et al. Quality of primary health care in China: challenges and recommendations. Lancet. 2020;395(10239):1802–12. https://doi.org/10.1016/s0140-6736(20)30122-7. [PMID: 32505251].
Wu Y, Ye R, Wang Q, Sun C, Meng S, Sylvia S, et al. Provider competence in hypertension management and challenges of the rural primary healthcare system in Sichuan province, China: a study based on standardized clinical vignettes. Bmc Health Serv Res. 2022;22(1):849. https://doi.org/10.1186/s12913-022-08179-9. [PMID: 35778732].
Shi J, Jin H, Shi L, Chen C, Ge X, Lu Y, et al. The quality of primary care in community health centers: comparison among urban, suburban and rural users in Shanghai, China. BMC Fam Pract. 2020;21(1):178. https://doi.org/10.1186/s12875-020-01250-6. [PMID: 32854623].
Li C, Chen Z, Khan MM. Bypassing primary care facilities: health-seeking behavior of middle age and older adults in China. Bmc Health Serv Res. 2021;21(1):895. https://doi.org/10.1186/s12913-021-06908-0. [PMID: 34461884].
Zhang A, Nikoloski Z, Albala SA, Yip W, Xu J, Mossialos E. Patient Choice of Health Care Providers in China: primary care facilities versus hospitals. Health Syst Reform. 2020;6(1):e1846844. https://doi.org/10.1080/23288604.2020.1846844. [PMID: 33314985].
Liu GG, Tang C, Liu Y, Bu T, Tang D. Will high-speed railway influence the healthcare seeking behaviour of patients? Quasi-experimental evidence from China. Health Policy Plan. 2021;36(10):1633–43. https://doi.org/10.1093/heapol/czab018. [PMID: 34058009].
Shen M, He W, Li L. Incentives to use primary care and their impact on healthcare utilization: evidence using a public health insurance dataset in China. Soc Sci Med. 2020;255:112981. https://doi.org/10.1016/j.socscimed.2020.112981. [PMID: 32315873].
Acknowledgements
We thank the officials of local health agencies and all participants and staff at the study sites for their cooperation.
Funding
This study was supported by the National Natural Science Foundation of China (72204147), and China Population Welfare Foundation (GJB-6-20211028-556). The funding bodies had no role in the design, data collection, analysis, interpretation of the data, and writing of this article.
Author information
Authors and Affiliations
Contributions
P.F., Y.W. and C.Z. conceived the idea and proofread the manuscript. P.F. and Y.W. coded and analysed the data, and P.F. prepared Figs. 1 and 2 and wrote the main manuscript. D.Z., J.Y., and C.Z. participated in the interpretation of the data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Ethical approval and consent to participate
All methods were carried out in accordance with relevant guidelines and regulations. This study protocol was approved by the Ethical Committee of Shandong University School of Public Health (No. 20,181,228). All respondents were fully informed with written informed consent for participation prior to the face-to-face interview.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Fu, P., Wang, Y., Zhao, D. et al. Does contracting family doctor promote primary healthcare utilization among older adults? - evidence from a difference-in-differences analysis. BMC Geriatr 24, 749 (2024). https://doi.org/10.1186/s12877-024-05336-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-05336-z