Abstract
Background
Previous studies have proven the positive relationship between healthy lifestyles and cognitive function in older adults. However, the specific impacts and mechanisms require further investigation. Therefore, this study aimed to investigate whether healthy lifestyles and cognitive function were associated with Chinese older adults and whether depressive symptoms mediated their association.
Methods
8272 valid samples were included using the latest data from the Chinese Longitudinal Healthy Longevity Survey (CLHLS). Pearson’s test was applied to investigate the relationship between the key variables. Regression models were employed to examine the mediating effects of healthy lifestyles, using Sobel’s test and the bootstrap method to confirm path effects.
Results
There was a significant correlation between healthy lifestyles, depressive symptoms, and cognitive function (p < 0.01). Healthy lifestyles directly impact cognitive function (β = 0.162, p < 0.01). Healthy lifestyles had a significant effect on depressive symptoms (β=-0.301, p < 0.01), while depressive symptoms have a significant impact on cognitive function (β=-0.108, p < 0.01). Depressive symptoms partially mediated the effect of healthy lifestyles on cognitive function (β = 0.032, p < 0.01). The Sobel and bootstrap tests confirmed the robustness of the regression analysis results.
Conclusion
Depressive symptoms mediate the relationship between healthy lifestyles and cognitive function. Our findings suggest that prevention strategies for cognitive impairment in older adults should focus on healthy lifestyles and mental health.
Similar content being viewed by others
Introduction
Population aging poses a significant challenge to public health worldwide. China, in particular, is currently undergoing a rapid and profound aging process [1]. According to China’s population census data, the total number of individuals aged 60 and older in China has reached 264 million, accounting for about 18.7% of the total population. Concurrently, cognitive decline associated with aging has emerged as a growing public health concern [2]. Some studies have shown that there are nearly 15 million dementia patients in China, approximately 25% of the worldwide total, and this number is constantly increasing [3]. Impaired cognitive function was associated with a range of adverse health outcomes, including mild cognitive impairment, Alzheimer’s disease, depressive symptoms, and physical impairment [4]. Furthermore, the decline in cognitive function carries serious social and economic burdens [5]. It is estimated that cognitive impairment results in a greater disease burden compared to cancer and cardiovascular disease, equating to approximately $19,144.36 per patient [6]. Therefore, addressing age-related cognitive decline has become a priority for public health [7].
The World Health Organization (WHO) has defined healthy lifestyles as taking actions that individuals can take within their capacity to promote physical, mental, and social health [8]. According to WHO recommendations, smoking, alcohol consumption, diet, and physical activity are identified as the four primary lifestyle behaviors influencing health outcomes [9]. Increasing evidence suggests that healthy lifestyles are important protective and easily modifiable factors for cognitive function [10]. Therefore, numerous researchers have explored the relationship between healthy lifestyles and cognitive function in different populations. For instance, a systematic review has demonstrated that individuals who abstain from smoking exhibit superior performance in daily activities and specific cognitive tasks compared to smokers [11]. Research has established that long-term excessive alcohol consumption may impair an individual’s executive function, memory, and metacognitive abilities [12]. Findings from a study conducted in China have revealed that adopting healthier lifestyles, which encompass abstaining from smoking and alcohol, engaging in moderate exercise, and maintaining a healthy diet and weight, is associated with enhanced cognitive function after accounting for genetic factors [13]. Similarly, a longitudinal study involving Korean elderly individuals found that maintaining an overall healthy lifestyle, measured by a composite healthy lifestyle score derived from factors such as smoking, alcohol consumption, weight, and exercise, was effective in preventing or mitigating cognitive decline [14]. Therefore, healthy lifestyles are an essential factor in preventing and mitigating cognitive impairment in older adults.
Depressive symptoms are a common mental disorder with significant impacts on an individual’s health and daily life [15]. Previous studies have shown that positive, healthy lifestyles are associated with a reduced risk of depressive symptoms [16, 17]. For example, a cross-sectional study found that higher smoking frequency and volume were associated with an increased risk of depressive symptoms in older adults [18]. A multinational study encompassing more than 50 countries identified a connection between alcohol consumption and episodes of depressive symptoms, though these associations exhibited heterogeneity across different nations [19]. Physical exercise could produce antidepressant effects through multiple biological and psychosocial pathways. Downstream cellular processes stimulated by neurotrophins during physical activity could result in structural changes in the brain, such as improved vascular circulation, which in turn improves areas associated with depressive symptoms, such as the hippocampus [20]. Physical activity probably increases personal social interactions and social support [21], contributing to a reduced risk of depressive symptoms [22]. Furthermore, several studies have emphasized the importance of dietary patterns and dietary diversity for the health of older adults, including mobility, physical health, and depressive symptoms [23, 24]. Therefore, positive and healthy lifestyles play a pivotal role in ameliorating depressive symptoms.
The relationship between depressive symptoms and cognitive function has been extensively studied in recent years [25]. Cognitive impairment is a central feature of depressive symptoms and is mainly characterized by a significant trend of decline in executive functioning, memory, and attention in depressed patients [26]. Cognitive function naturally diminishes in older adults, influenced by various factors, including structural changes in the brain (such as fewer neurons and changes in synaptic connectivity), cerebrovascular disease, medication side effects, reduced physical activity, and psychological and social stress [27]. Notably, depressive symptoms further exacerbate the adverse impact of these contributing factors [28]. Furthermore, some studies have proposed that depressive symptoms might serve as early indicators or precursors of cognitive decline, potentially contributing to subsequent cognitive deterioration in older adults [29]. For instance, a longitudinal study has established an association between depressive symptoms and diminished cognitive function in older adults [30]. Individuals experiencing depressive symptoms often suffer from low self-esteem, decreased motivation, and disruptions in sleep patterns, all of which can impose a cognitive burden [31]. Moreover, poorer sleep quality may impede the brain’s ability to efficiently remove protein waste, potentially leading to cognitive decline [32]. Therefore, depressive symptoms are an important predictor of cognitive function in older adults.
An integrated healthy lifestyle considers the interactions and interconnectedness between different lifestyles among various aspects of healthy living rather than concentrating solely on a single facet of a healthy lifestyle [33]. Therefore, it is important to analyze the potential effects of integrating healthy lifestyles on the cognitive performance of older adults [34]. Moreover, most of the existing evidence comes from studies conducted in developed countries, making it challenging to generalize the findings to other populations due to variations in genetic factors, economic disparities, and sociocultural distinctions [35]. Given that China is the world’s largest developing country and has the largest elderly population, it is imperative to conduct extensive investigations into the healthy lifestyles and cognition of Chinese older adults [36]. Several scholars have investigated the relationship between healthy lifestyles and cognitive function in older adults [37, 38]. However, few have investigated the mediating role of depressive symptoms between healthy lifestyles and cognitive function among older adults in the Chinese context. Therefore, this study aimed to investigate the relationship between healthy lifestyles, depressive symptoms, and cognitive functioning in older adults. Based on the theories and literature above, we proposed the following hypotheses:
H1: Cognitive function is influenced by healthy lifestyles.
H2: Depressive symptoms are influenced by healthy lifestyles.
H3: Cognitive function is influenced by depressive symptoms.
Methods
Study population and data source
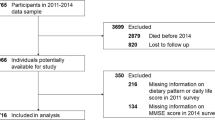
The data for this study were derived from the 2018 wave of the Chinese Longitudinal Healthy Longevity Survey (CLHLS). The CLHLS is a nationally representative comprehensive survey of the elderly in China, covering the domains of physical and mental health, cognitive function, social participation, health behaviors, socioeconomic status, family structure, intergenerational relationships, and caregiving needs. The CLHLS was initiated in 1998 and carried out every two to three years by Peking University’s Center for Healthy Aging and Family Studies and the China National Research Center on Aging. To ensure good scientific and national representativeness, CLHLS employed a multi-stage disproportionate and targeted random sampling method covering 23 provinces, municipalities, and autonomous regions in China. We excluded samples with ages less than 60 and missing variables. A total of 8272 observations were finally included in the final analysis. The absence of relevant important variables is shown in Fig. 1.
Every participant provided written informed consent. CLHLS was approved by the Research Ethics Boards of Peking University and Duke University (IRB00001052-13074) and conducted in accordance with approved guidelines. This study utilized publicly available and de-identified data from CLHLS 2018, thus exempting it from the need for additional ethical approval.
Measures
Referring to previous studies [39], a healthy lifestyle was measured by smoking, drinking, exercise status, and nutritional intake. Smoking, drinking, and not exercising were scored as zero points. Otherwise, they were scored as one point. Nutritional intake was assessed using the Dietary Diversity Score (DDS), which considered consumption of fruits, vegetables, meat, eggs, fish, beans, nuts, milk, and tea. The DDS scale has acceptable reliability (Cronbach’s alpha = 0.631) and validity (KMO = 0.747, p < 0.001). Individuals who responded “often or almost every day” were scored as one, while those who reported “occasionally” or “rarely or never” were scored as zero. The DDS was calculated by summing the scores of all the items, resulting in a range from 0 to 9, where higher scores signified greater dietary diversity. A score of 1 was assigned for a favorable DDS (7–9 DDS); otherwise, a score of 0 was recorded [40]. Consequently, we summed scores for smoking, drinking, physical activity, and DDS to calculate the Healthy Lifestyle Score. The Healthy Lifestyle Score ranged from 0 to 4, with higher scores indicating healthier lifestyles.
Depressive symptoms were measured using the Center for Epidemiologic Studies Depression Scale (CESD-10) [41]. The CESD-10 exhibited good reliability and validity, which was validated and applied to Chinese older adults. In this study, the reliability (Cronbach’s alpha = 0.735) and validity (KMO = 0.839, p < 0.001) of the CES-D10 scale were good. During the process of the CES-D10 investigation, participants were requested to assess their personal status in the past week. Each question had four options: 0 = never, 1 = seldom or sometimes, 2 = sometimes, and 3 = always. The CESD-10 score was derived by summing the responses to the 10 items, ranging from 0 to 30. Higher CESD-10 scores were associated with more severe depressive symptoms [42].
Cognitive function in the CLHLS study was evaluated using the Chinese version of the Mini-Mental State Examination (MMSE), which has been validated for validity and reliability [43]. The MMSE questionnaire comprised 24 items that evaluated orientation, one-minute food counting, attention, calculation, drawing, recall, and language skills. Food counting in one minute was scored from 0 to 7 points, with 1 point assigned for each correctly counted food item, up to a maximum of 7 points. Other questions were assigned a value of 1 for a correct answer and 0 for an incorrect answer. MMSE scores ranged from 0 to 30, with higher scores denoting higher cognitive function. Participants with MMSE scores ≥ 24 and < 24 are respectively defined as having “normal cognitive function” and “cognitive impairment [44]. In this study, the MMSE scale had good reliability (Cronbach’s alpha = 0.705) and validity (KMO = 0.818, p < 0.001) [45].
Considering the effect of potential confounders, several covariates were included in this study, including age, gender, ethnicity, household registration, marriage status, years of education, socioeconomic status, living arrangements, and self-rated health. Gender, ethnicity, hukou, marital status, and living arrangements were dichotomous variables. Living arrangements are categorized as living alone and living with household member(s). Residence with household member(s) was set to 1, otherwise it was 0. Socioeconomic status and self-assessed health were scored using a five-point Likert scale, with responses ranging from 1 (very poor) to 5 (very good). Years of education were assessed based on the question, “How many years of schooling have you had?”
Statistical analysis
We conducted all statistical analyses using STATA version 17.0. Firstly, this study performed a statistical description of sociodemographic characteristics and key variables. Categorical variables were described by frequencies (percentages) and continuous variables by means (standard deviation, SD). Differences in characteristics between subgroups of different cognitive functions were compared using t-tests or chi-square tests [46]. Secondly, Pearson’s correlation analysis was employed to measure bivariate correlations between healthy lifestyles, depressive symptoms, and cognitive function. Next, Judd and Kenny’s recommendations and Baron and Kenny’s causal step approach were employed to investigate the relationship between healthy lifestyles, depression, and cognitive function in older adults [47]. Therefore, the three regression processes would estimate the following effects: (1) the effect of healthy lifestyles on cognitive function; (2) the effect of healthy lifestyles on depressive symptoms; (3) the effect of depressive symptoms on cognitive function when healthy lifestyles were controlled; and (4) the effect of healthy lifestyles on cognitive function when depressive symptoms were controlled. Covariates were included in all regression analyses to improve the accuracy of model estimation. Subsequently, we used the Sobel test to rigorously examine whether the indirect effect was significantly non-zero. The indirect effect was considered significant if the Z-value obtained from the Sobel test exceeded 1.96. To determine effect sizes and obtain 95% confidence intervals, we assessed direct, indirect, and total effects using the bootstrap method with 5000 iterations [47]. A significant effect was shown when the 95% confidence interval did not include zero. All statistical tests were two-sided, and p < 0.05 was considered statistically significant.
Results
Table 1 presents the descriptive statistics of the participants. A total of 8272 participants were recruited in the study, with an average age of 81.73 years, comprising 3954 males and 4318 females. The majority of participants were Han Chinese (94.79%), divorced, widowed, or unmarried (51.06%), registered rural households (67.70%), and lived with others (83.64%). Participants whose socio-economic status was very poor, poor, fair, good, and very good accounted for 0.85%, 11.74%, 38.32%, 35.88%, and 3.02%, respectively. The percentages of participants who rated their health as very poor, poor, fair, good, and very good were 1.05%, 8.09%, 69.73%, 18.11%, and 13.21%, respectively. The means for education, healthy lifestyles, depressive symptoms, and cognitive function were 4.07 years, 2.28 points, 7.15 points, and 26.79 points, respectively. There were significant differences between cognitive impairment and normal cognitive functioning in terms of age, gender, ethnic, marriage, years of education, household registration, self-rated health, socioeconomic status, healthy lifestyles, depressive symptoms, and cognitive functioning.
As shown in Table 2, the results of Pearson’s correlation analysis suggested that there were mutually significant correlations between healthy lifestyles, depressive symptoms, and cognitive function (p < 0.01). Specifically, healthy lifestyles were negatively associated with depressive symptoms (r=-0.102, p < 0.01) and positively associated with cognitive function (r = 0.084, p < 0.01). Depressive symptoms were negatively correlated with cognitive function (r=-0.202, p < 0.01).
Regression analysis was utilized to explore the mediating role of depressive symptoms on the relationship between healthy lifestyles and cognitive function. We calculate the variance inflation factor (VIF) of the covariates of the three equations separately, and the corresponding variance inflation factors (VIF) of all the variables are < 2, indicating that there is not excessive multicollinearity problem [48, 49]. Table 3; Fig. 2 demonstrate the results of the mediation analysis of depressive symptoms between healthy lifestyles and cognitive function after controlling for covariates. In the total effects regression, healthy lifestyles were a significant predictor of cognitive function (β = 0.194, p < 0.01). This relationship remained significant when depressive symptoms was considered (β = 0.162, p < 0.01). Moreover, healthy lifestyles showed a significant effect on depressive symptoms (β=-0.301, p < 0.01), whereas depressive symptoms exerted a significant effect on cognitive function (β=-0.136, p < 0.01).
The Sobel and bootstrap tests were conducted to check for indirect, direct, and total effects [50]. As shown in Table 4, Sobel’s test indicates that the indirect effect (Z = 5.098, p < 0.001), direct effect (Z = 3.322, p < 0.001), and total effect (Z = 3.971, p < 0.001) were significant. It suggested that healthy lifestyles affect depressive symptoms, which in turn affects cognitive function. The bootstrap method indicated that the direct effect of healthy lifestyles on cognitive function was 0.162 (95% CI: 0.082, 0.241), while the total effect was 0.194 (95% CI: 0.113, 0.272). The indirect effect of healthy lifestyles on cognitive function mediated by depressive symptoms was 0.032 (95% CI: 0.020, 0.045). All paths were significant, indicating the robustness of the mediation model results [51].
Discussion
Using data from the 2018 Chinese Longitudinal Healthy Longevity Survey (CLHLS), the study found significant associations between healthy lifestyles and depressive symptoms and cognitive function among Chinese older adults. Depressive symptoms partially mediated the relationship between healthy lifestyles and cognitive functioning. The Sobel and Bootstrap methods supported the results of the underlying analyses, indicating the robustness of the results.
The present study found that healthy lifestyles have a positive predictive effect on cognitive function in the Chinese elderly population, which supports hypothesis 1. Several potential mechanisms underpin this relationship. For instance, smoking can elevate oxidative stress levels, affecting the cognitive degenerative process and increasing the risk of developing age-related cognitive impairment [52]. Excessive alcohol consumption may result in alcohol-related brain damage, including alcohol-related memory deficits and executive dysfunction [53]. Additionally, there exists a favorable correlation between physical exercise and cognitive improvement [54]. Physical activity boosts the levels of brain-derived neurotrophic factors, which play a pivotal role in enhancing cognitive performance [55]. Different types of food provide various nutrients, such as vitamins, minerals, and antioxidants, closely linked to brain health and cognitive function [56]. Simultaneously, the physiological functions related to nutrient intake, such as chewing, salivation, and absorption, tend to diminish with age [57]. Therefore, older adults are more susceptible to poor dietary habits, potentially leading to cognitive impairment [58]. Furthermore, this study provides evidence regarding the collective impact of multiple healthy lifestyle factors on cognition, comprehensively evaluating them through assessments of smoking, alcohol consumption, exercise status, and nutrient intake [59]. Regular physical activity increases blood flow to the brain and promotes the release of nerve growth factors, which contribute to neuronal growth and survival [60]. Positive social interactions reduce stress, loneliness and depression and provide cognitive stimulation to keep the brain active [61]. Good quality sleep helps the brain clear metabolic waste such as beta-amyloid, and the accumulation of these waste products is associated with the development of cognitive disorders such as Alzheimer’s disease [62].
Healthy lifestyles are associated with a reduced risk of depressive symptoms in older adults, confirming Hypothesis 2. The connection between healthy lifestyles and depressive symptoms can be elucidated through various biological and social mechanisms. Smoking, for instance, induces a short-term pharmacological effect that stimulates the brain and alleviates stress and anxiety [63]. However, it’s important to note that smoking can be addictive and potentially render individuals more sensitive, vulnerable, and anxious. On the other hand, excessive alcohol consumption has the potential to lead to alcohol dependence, as it can alter neurotransmitter production and brain function, heightening feelings of anxiety [64]. In contrast, physical activity plays an effective role in stimulating regional cerebral blood flow and promoting the body’s dopamine production, thereby maintaining a positive mood [65]. Additionally, the consumption of a diverse and healthy diet is closely associated with better nutritional status, which, in turn, can contribute to the reduction of depressive symptoms [66]. Moreover, the social context significantly influences the connection between lifestyles and depressive symptoms. Social support, for example, has the potential to promote a healthy lifestyle by alleviating stress and providing essential emotional support, effectively reducing an individual’s risk of depressive symptoms [67]. Conversely, high-intensity social stress, such as work-related pressure and family conflicts, can lead to unhealthy lifestyles, including irregular sleep patterns, disrupted dietary habits, and a lack of physical exercise, consequently increasing the risk of depressive symptoms [68].
Depressive symptoms are associated with cognitive impairment, supporting Hypothesis 3. Indeed, depressive symptoms are associated with abnormal neurotransmitter secretion and altered neuronal activity. Depressed individuals typically exhibit reduced levels of neurotransmitters like serotonin and norepinephrine in their brains, along with elevated levels of excitatory neurotransmitters like glutamate [69]. These abnormal neurotransmitter levels can lead to unstable neuronal activity, subsequently impacting cognitive function [70]. Depressive symptoms are often accompanied by a deterioration in social functioning, leading to damage to social networks and support systems, which may result in a dearth of emotional support and social isolation [71]. Research indicates that decreased social functioning and weakened social networks are associated with cognitive impairment [72]. Moreover, individuals with depressive symptoms often experience cognitive impairments, including poor concentration and memory lapses [73]. Specifically, they often experience fatigue, helplessness, and disorientation, and these emotional states could impact their ability to concentrate and remember information. Furthermore, depressive symptoms are associated with lower self-evaluation and self-esteem, potentially influencing the performance of cognitive function [74]. Therefore, the mechanisms by which depressive symptoms affect cognitive functioning are multifaceted, including biological, sociological, and psychological mechanisms.
The results of the Sobel and Bootstrap analyses suggest that depressive symptoms partially mediate the relationship between healthy lifestyles and cognitive function. Specifically, the direct effect of healthy lifestyles on cognitive function was 0.162, the total effect was 0.194, and the indirect effect mediated by depressive symptoms was 0.032. These findings suggest that healthy lifestyles have the potential to deter the onset of depressive symptoms, thereby reducing the risk of cognitive decline in the elderly population [75]. Therefore, it is imperative to prioritize the well-being of older adults by focusing on their healthy lifestyles and mental health [76]. To enhance cognitive function in this demographic, we recommend the promotion of healthy lifestyles and the cultivation of positive psychological states. This can be accomplished through the reinforcement of physical exercise, the advocacy of a well-rounded and nutritious diet, and the provision of professional mental health support and counseling services [77]. Implementing these measures can prevent cognitive impairment and improve the quality of life of older adults, thus contributing to the alleviation of the significant challenges presented by population aging [78].
The interpretation of the results of this study should be considered in the context of several limitations. Firstly, this study is a cross-sectional design, which cannot establish precise causal relationships between variables. Future studies could employ longitudinal randomized controlled trials to verify causal relationships between variables. Secondly, the data on healthy lifestyles and depression were assessed through self-report questionnaires, which may introduce reporting biases. Subsequently, although this study controlled for several covariates, potential confounding factors may still exist and influence our conclusions. Finally, we excluded samples containing missing values, which could introduce potential estimation bias. Once again, the limitation about the sample being restricted to those who were able to answer the questionnaire is significant, and this constraint may introduce selection bias.
Conclusion
This study investigated the relationship between healthy lifestyles, depressive symptoms, and cognitive function in Chinese older adults. Our findings showed significant correlations between healthy lifestyles and depressive symptoms and cognitive function in Chinese older adults. Depressive symptoms were found to mediate the relationship between healthy lifestyles and cognitive function. Our study suggests that relevant governments and staff should consider the mechanism of action of promoting healthy lifestyles and mental health diversion when developing strategies to improve cognitive functioning in older adults. Initiatives such as lifestyle programs, psychological support and counseling services, regular check-ups, and healthcare interventions specifically targeting older adults can effectively prevent or delay cognitive decline, thus achieving the goal of healthy aging.
Data availability
The data for this study was the Chinese Longitudinal Healthy Longevity Survey (CLHLS) by the Center for Healthy Aging and Development, Peking University. https://doi.org/10.18170/DVN/WBO7LK.
References
Zhang XD, Han HY. Spatiotemporal dynamic characteristics and causes of China’s population aging from 2000 to 2020. Sustainability. 2023;15(9):7212. https://doi.org/10.3390/su15097212.
Lassi M, Fabbiani C, Mazzeo S, Burali R, Vergani AA, Giacomucci G, et al. Degradation of EEG microstates patterns in subjective cognitive decline and mild cognitive impairment: early biomarkers along the Alzheimer’s disease continuum? NeuroImage-Clin. 2023;38:15. https://doi.org/10.1016/j.nicl.2023.103407.
Ren R, Qi J, Lin S, Liu X, Yin P, Wang Z, et al. The China Alzheimer Report 2022. Gen Psychiatr. 2022;35(1):e100751. https://doi.org/10.1136/gpsych-2022-100751.
Denver P, McClean PL. Distinguishing normal brain aging from the development of Alzheimer’s disease: inflammation, insulin signaling and cognition. Neural Regen Res. 2018;13(10):1719–30. https://doi.org/10.4103/1673-5374.238608.
Wang J, Xiao LD, He GP, De Bellis A. Family caregiver challenges in dementia care in a country with undeveloped dementia services. J Adv Nurs. 2014;70(6):1369–80. https://doi.org/10.1111/jan.12299.
Jia J, Wei C, Chen S, Li F, Tang Y, Qin W, et al. The cost of Alzheimer’s disease in China and re-estimation of costs worldwide. Alzheimers Dement. 2018;14(4):483–91. https://doi.org/10.1016/j.jalz.2017.12.006.
Beard JR, Officer A, de Carvalho IA, Sadana R, Pot AM, Michel JP, et al. The world report on ageing and health: a policy framework for healthy ageing. Lancet. 2016;387(10033):2145–54. https://doi.org/10.1016/S0140-6736(15)00516-4.
Glymour MM, Avendano M. Can self-reported strokes be used to study stroke incidence and risk factors? Evidence from the health and retirement study. Stroke. 2009;40(3):873–9. https://doi.org/10.1161/STROKEAHA.108.529479.
Hua Y, Wang B, Wallen GR, Shao P, Ni C, Hua Q. Health-promoting lifestyles and depression in urban elderly Chinese. PLoS ONE. 2015;10(3):e0117998. https://doi.org/10.1371/journal.pone.0117998.
Wang Z, Pang Y, Liu J, Wang J, Xie Z, Huang T. Association of healthy lifestyle with cognitive function among Chinese older adults. Eur J Clin Nutr. 2021;75(2):325–34. https://doi.org/10.1038/s41430-020-00785-2.
Wang YY, Wang S, Zheng W, Zhong BL, Ng CH, Ungvari GS, et al. Cognitive functions in smoking and non-smoking patients with schizophrenia: a systematic review and meta-analysis of comparative studies. Psychiatry Res. 2019;272:155–63. https://doi.org/10.1016/j.psychres.2018.12.064.
Le Berre AP, Fama R, Sullivan EV. Executive functions, memory, and social cognitive deficits and recovery in chronic alcoholism: a critical review to inform future research. Alcohol Clin Exp Res. 2017;41(8):1432–43. https://doi.org/10.1111/acer.13431.
Jin X, He W, Zhang Y, Gong E, Niu Z, Ji J, et al. Association of APOE ε4 genotype and lifestyle with cognitive function among Chinese adults aged 80 years and older: a cross-sectional study. PLoS Med. 2021;18(6):e1003597. https://doi.org/10.1371/journal.pmed.1003597.
Lee HJ, Jang J, Choi DW, Chae W, Park EC, Jang SI. Association between change in lifestyle and cognitive functions among elderly koreans: findings from the Korean longitudinal study of aging (2006–2016). BMC Geriatr. 2020;20(1):317. https://doi.org/10.1186/s12877-020-01693-7.
Petersen RC, Smith GE, Waring SC, Ivnik RJ, Tangalos EG, Kokmen E. Mild cognitive impairment: clinical characterization and outcome. Arch Neurol. 1999;56(3):303–8. https://doi.org/10.1001/archneur.56.3.303.
Cao Z, Yang H, Ye Y, Zhang Y, Li S, Zhao H, et al. Polygenic risk score, healthy lifestyles, and risk of incident depression. Transl Psychiatry. 2021;11(1):189. https://doi.org/10.1038/s41398-021-01306-w.
Mazurek Melnyk B, Hoying J, Tan A. Effects of the MINDSTRONG© CBT-based program on depression, anxiety and healthy lifestyle behaviors in graduate health sciences students. J Am Coll Health. 2022;70(4):1001–9. https://doi.org/10.1080/07448481.2020.1782922.
Wu Z, Yue Q, Zhao Z, Wen J, Tang L, Zhong Z, et al. A cross-sectional study of smoking and depression among US adults: NHANES (2005–2018). Front Public Health. 2023;11:1081706. https://doi.org/10.3389/fpubh.2023.1081706.
Keyes KM, Allel K, Staudinger UM, Ornstein KA, Calvo E. Alcohol consumption predicts incidence of depressive episodes across 10 years among older adults in 19 countries. Int Rev Neurobiol. 2019;148:1–38. https://doi.org/10.1016/bs.irn.2019.09.001.
Cicek G, Atan T, Kamuk YU, Imamoglu O, Yamaner F, Aslan V. Effects of exercise on levels of depression. Anthropol. 2015;20(3):670–4. https://doi.org/10.1080/09720073.2015.11891772.
Cao J, Wang K, Shi YH, Pan YQ, Lyu M, Ji Y. The associations between social support change and physical activity trajectory from late adolescence to young adulthood. BMC Public Health. 2023;23(1):11. https://doi.org/10.1186/s12889-023-16422-z.
Zhou Y, Guo KL. Physical activity and depression: a chain mediation model. Soc Behav Pers. 2023;51(10):9. https://doi.org/10.2224/sbp.12646.
Hsiao FY, Peng LN, Lee WJ, Chen LK. Higher dietary diversity and better healthy aging: a 4-year study of community-dwelling middle-aged and older adults from the Taiwan Longitudinal Study of Aging. Exp Gerontol. 2022;168:111929. https://doi.org/10.1016/j.exger.2022.111929.
Poorrezaeian M, Siassi F, Milajerdi A, Qorbani M, Karimi J, Sohrabi-Kabi R, et al. Depression is related to dietary diversity score in women: a cross-sectional study from a developing country. Ann Gen Psychiatry. 2017;16:39. https://doi.org/10.1186/s12991-017-0162-2.
Rapp MA, Schnaider-Beeri M, Wysocki M, Guerrero-Berroa E, Grossman HT, Heinz A, et al. Cognitive decline in patients with dementia as a function of depression. Am J Geriatr Psychiatry. 2011;19(4):357–63. https://doi.org/10.1097/JGP.0b013e3181e898d0.
Rock PL, Roiser JP, Riedel WJ, Blackwell AD. Cognitive impairment in depression: a systematic review and meta-analysis. Psychol Med. 2014;44(10):2029–40. https://doi.org/10.1017/S0033291713002535.
Hopkins EG, Leman PJ, Cervin M, Numbers K, Brodaty H, Kochan NA, et al. Network of mental activities, cognitive function and depression in older men and women. J Psychiatr Res. 2023;162:113–22. https://doi.org/10.1016/j.jpsychires.2023.05.030.
Lin TH, Chang SF, Liao MT, Chen YH, Tsai HC. The relationships between physical function, nutrition, cognitive function, depression, and sleep quality for facility-dwelling older adults with dynapenia. BMC Geriatr. 2023;23(1):15. https://doi.org/10.1186/s12877-023-03847-9.
Perrino T, Mason CA, Brown SC, Spokane A, Szapocznik J. Longitudinal relationships between cognitive functioning and depressive symptoms among hispanic older adults. J Gerontol B Psychol Sci Soc Sci. 2008;63(5):309–17. https://doi.org/10.1093/geronb/63.5.P309.
Wei J, Ying M, Xie L, Chandrasekar EK, Lu H, Wang T, et al. Late-life depression and cognitive function among older adults in the U.S.: the national health and nutrition examination survey, 2011–2014. J Psychiatr Res. 2019;111:30–5. https://doi.org/10.1016/j.jpsychires.2019.01.012.
Zheng XW, Jiang ML, Ren X, Han LY. Combined influence of depressive symptoms and systemic inflammation on cardiovascular diseases in China. J Psychosomat Res. 2023;174:111480. https://doi.org/10.1016/j.jpsychores.2023.111480.
Liang W, Miao J, Wang Y, Sun W, Pan C, Chen M, et al. Longitudinal relationships between depressive symptoms and cognitive function after stroke: a cross-lagged panel design. J Psychosom Res. 2023;174:111486. https://doi.org/10.1016/j.jpsychores.2023.111486.
Lee Y, Kim J, Back JH. The influence of multiple lifestyle behaviors on cognitive function in older persons living in the community. Prev Med. 2009;48(1):86–90. https://doi.org/10.1016/j.ypmed.2008.10.021.
Dannefer D. Cumulative advantage/disadvantage and the life course: cross-fertilizing age and social science theory. J Gerontol B Psychol Sci Soc Sci. 2003;58(6):S327–37. https://doi.org/10.1093/geronb/58.6.S327.
Jin S, Li C, Cao X, Chen C, Ye Z, Liu Z. Association of lifestyle with mortality and the mediating role of aging among older adults in China. Arch Gerontol Geriatr. 2022;98:104559. https://doi.org/10.1016/j.archger.2021.104559.
Liu H, Wang Z, Zou L, Gu S, Zhang M, Hukportie DN, et al. Favourable lifestyle protects cognitive function in older adults with high genetic risk of obesity: a prospective cohort study. Front Mol Neurosci. 2022;15:808209. https://doi.org/10.3389/fnmol.2022.808209.
Zhang HC, Chen YY, Ni RY, Cao YW, Fang WB, Hu W, et al. Traffic-related air pollution, adherence to healthy lifestyles, and risk of cognitive impairment: a nationwide population-based study. Ecotox Environ Safe. 2023;262:115349. https://doi.org/10.1016/j.ecoenv.2023.115349.
Halloway S, Wagner M, Tangney C, Lange-Maia BS, Bennett DA, Arvanitakis Z, et al. Profiles of lifestyle health behaviors and cognitive decline in older adults. Alzheimers Dement. 2023;20(1):472–82. https://doi.org/10.1002/alz.13459.
Wang J, Chen C, Zhou J, Ye L, Li Y, Xu L, et al. Healthy lifestyle in late-life, longevity genes, and life expectancy among older adults: a 20-year, population-based, prospective cohort study. Lancet Healthy Longev. 2023;4(10):e535–43. https://doi.org/10.1016/S2666-7568(23)00140-X.
Cheng T, Zhang B, Luo L, Guo J. The influence of healthy lifestyle behaviors on cognitive function among older Chinese adults across age and gender: evidence from panel data. Arch Gerontol Geriatr. 2023;112:105040. https://doi.org/10.1016/j.archger.2023.105040.
Qiu WD, Cai AP, Li LW, Feng YQ. Association of depression trajectories and subsequent hypertension and cardiovascular disease: findings from the CHARLS cohort. J Hypertens. 2024;42(3):432–40. https://doi.org/10.1097/HJH.0000000000003609.
Pakhomova TE, Tam C, Wang L, Salters K, Moore DM, Barath J, et al. Depressive symptoms, the impact on art continuation, and factors associated with symptom improvement among a cohort of people living with HIV in British Columbia, Canada. AIDS Behav. 2024;28(1):43–58. https://doi.org/10.1007/s10461-023-04156-3.
Roca F, Lepiller L, Keroulle C, Lesage D, Rougette K, Chassagne P. Effect of a multimodal training on the ability of medical students to administer the MMSE: a comparative study. BMC Med Educ. 2024;24(1):9. https://doi.org/10.1186/s12909-024-05044-7.
Jun MH, Ku B, Kim K, Lee KH, Kim JU. A screening method for mild cognitive impairment in elderly individuals combining bioimpedance and MMSE. Front Aging Neurosci. 2024;16:15. https://doi.org/10.3389/fnagi.2024.1307204.
Yen C-F, Hwang A-W, Liou T-H, Chiu T-Y, Hsu H-Y, Chi W-C, et al. Validity and reliability of the functioning disability evaluation scale-adult version based on the WHODAS 2.0–36 items. J Formos Med Assoc. 2014;113(11):839–49. https://doi.org/10.1016/j.jfma.2014.08.008.
Yang Q, Jia J. Association of intergenerational relationships with cognitive impairment among Chinese adults 80 years of age or older: prospective cohort study. BMC Geriatr. 2022;22(1):838. https://doi.org/10.1186/s12877-022-03529-y.
Wang G, Zhou Y, Duan J, Kan Q, Cheng Z, Tang S. Effects of adverse childhood health experiences on cognitive function in Chinese middle-aged and older adults: mediating role of depression. BMC Public Health. 2023;23(1):1293. https://doi.org/10.1186/s12889-023-16169-7.
Wei K, Liu Y, Yang J, et al. Living arrangement modifies the associations of loneliness with adverse health outcomes in older adults: evidence from the CLHLS. BMC Geriatr. 2022;22:59. https://doi.org/10.1186/s12877-021-02742-5.
Zhang J, Xu G, Xu L. Number of teeth and denture use are associated with frailty among Chinese older adults: a cohort study based on the CLHLS from 2008 to 2018. J Nutr Health Aging. 2023;27(11):972–9. https://doi.org/10.1007/s12603-023-2014-x.
Sobel ME. Asymptotic confidence intervals for indirect effects in structural equation models. Sociol Methodol. 1982;13:290–312. https://doi.org/10.2307/270723.
Cristi-Montero C, Courel-Ibáñez J, Ortega FB, Castro-Piñero J, Santaliestra-Pasias A, Polito A, et al. Mediation role of cardiorespiratory fitness on the association between fatness and cardiometabolic risk in European adolescents: the HELENA study. J Sport Health Sci. 2021;10(3):360–7. https://doi.org/10.1016/j.jshs.2019.08.003.
Ge S, Tang X, Wei Z, Dune L, Liu T, Li J, et al. Smoking and cognitive function among middle-aged adults in China: findings from the China health and retirement longitudinal study baseline survey. J Addictions Nurs. 2020;31(3):E5–12. https://doi.org/10.1097/JAN.0000000000000352.
Han L, Jia J. Long-term effects of alcohol consumption on cognitive function in seniors:a cohort study in China. BMC Geriatr. 2021;21(1):699. https://doi.org/10.1186/s12877-021-02606-y.
Sáez de Asteasu ML, Martínez-Velilla N, Zambom-Ferraresi F, Casas-Herrero Á, Izquierdo M. Role of physical exercise on cognitive function in healthy older adults: a systematic review of randomized clinical trials. Ageing Res Rev. 2017;37:117–34. https://doi.org/10.1016/j.arr.2017.05.007.
Kim B, Kang S. Regular leisure-time physical activity is effective in boosting neurotrophic factors and alleviating menopause symptoms. Int J Environ Res Public Health. 2020;17(22):8624. https://doi.org/10.3390/ijerph17228624.
Beydoun MA, Gamaldo AA, Beydoun HA, Tanaka T, Tucker KL, Talegawkar SA, et al. Caffeine and alcohol intakes and overall nutrient adequacy are associated with longitudinal cognitive performance among U.S. adults. J Nutr. 2014;144(6):890–901. https://doi.org/10.3945/jn.113.189027.
Phillips RM. Nutrition and depression in the community-based oldest-old. Home Healthc Now. 2012;30(8):462–71. https://doi.org/10.1097/NHH.0b013e31826517ad.
Andriollo-Sanchez M, Hininger-Favier I, Meunier N, Venneria E, O’Connor JM, Maiani G, et al. Age-related oxidative stress and antioxidant parameters in middle-aged and older European subjects: the ZENITH study. Eur J Clin Nutr. 2005;59(2):S58–62. https://doi.org/10.1038/sj.ejcn.1602300.
Goodwin RD, Prescott M, Tamburrino M, Calabrese JR, Liberzon I, Galea S. Smoking is a predictor of depression onset among national guard soldiers. Psychiatry Res. 2013;206(2):321–3. https://doi.org/10.1016/j.psychres.2012.11.025.
Aggio D, Smith L, Fisher A, Hamer M. Context-specific associations of physical activity and sedentary behavior with cognition in children. Am J Epidemiol. 2016;183(12):1075–82. https://doi.org/10.1093/aje/kww031.
Liu CL, Jeong H, Cui HN, Dewaele JM, Okamoto K, Suzuki Y, et al. Effects of social interactions on the neural representation of emotional words in late bilinguals. Lang Cogn Neurosci. 2024;17. https://doi.org/10.1080/23273798.2024.2307630.
Koutsonida M, Psyhogiou M, Aretouli E, Tsilidis KK. Sleep quality and cognitive abilities in the Greek cohort of epirus health study. Nat Sci Sleep. 2024;16:33–42. https://doi.org/10.2147/NSS.S436519.
Linli ZQ, Feng JF, Zhao W, Guo SX. Associations between smoking and accelerated brain ageing. Prog Neuro-Psychopharmacol Biol Psychiatry. 2022;113:110471. https://doi.org/10.1016/j.pnpbp.2021.110471.
Kolla BP, Winham SJ, Ho AMC, Mansukhani MP, Loukianova LL, Pazdernik V, et al. The interaction between brain-derived neurotrophic factor levels and alcohol consumption, sleep disturbance and sex-hormones in alcohol use disorders. Alcohol Alcohol. 2023;58(2):209–15. https://doi.org/10.1093/alcalc/agad001.
Boolani A, Sur S, Yang D, Avolio A, Goodwin A, Mondal S, et al. Six minutes of physical activity improves mood in older adults: a pilot study. J Geriatr Phys Ther. 2021;44(1):18–24. https://doi.org/10.1519/JPT.0000000000000233.
Yun H, Kim DW, Lee EJ, Jung J, Yoo S. Analysis of the effects of nutrient intake and dietary habits on depression in Korean adults. Nutrients. 2021;13(4):1360. https://doi.org/10.3390/nu13041360.
Liu L, Gou Z, Zuo J. Social support mediates loneliness and depression in elderly people. J Health Psychol. 2016;21(5):750–8. https://doi.org/10.1177/1359105314536941.
Chaouloff F. Social stress models in depression research: what do they tell us? Cell Tissue Res. 2013;354(1):179–90. https://doi.org/10.1007/s00441-013-1606-x.
Laxton AW, Neimat JS, Davis KD, Womelsdorf T, Hutchison WD, Dostrovsky JO, et al. Neuronal coding of implicit emotion categories in the subcallosal cortex in patients with depression. Biol Psychiatry. 2013;74(10):714–9. https://doi.org/10.1016/j.biopsych.2013.03.029.
Chen J, Chen X, Mao R, Fu Y, Chen Q, Zhang C, et al. Hypertension, sleep quality, depression, and cognitive function in elderly: a cross-sectional study. Front Aging Neurosci. 2023;15:1051298. https://doi.org/10.3389/fnagi.2023.1051298.
Li C, Jiang S, Zhang X. Intergenerational relationship, family social support, and depression among Chinese elderly: a structural equation modeling analysis. J Affect Disord. 2019;248:73–80. https://doi.org/10.1016/j.jad.2019.01.032.
Kelly ME, Duff H, Kelly S, McHugh Power JE, Brennan S, Lawlor BA, et al. The impact of social activities, social networks, social support and social relationships on the cognitive functioning of healthy older adults: a systematic review. Syst Rev. 2017;6(1):259. https://doi.org/10.1186/s13643-017-0632-2.
Van der Linde RM, Brayne C, Dening T. Depression and other behavioral and psychological symptoms of dementia - separate research worlds in need of a common understanding. Int Psychogeriatr. 2014;26(2):177–83. https://doi.org/10.1017/S1041610213001592.
Rapp MA, Schnaider-Beeri M, Grossman HT, Sano M, Perl DP, Purohit DP, et al. Increased hippocampal plaques and tangles in patients with Alzheimer disease with a lifetime history of major depression. Arch Gen Psychiatry. 2006;63(2):161–7. https://doi.org/10.1001/archpsyc.63.2.161.
Ding ZH, Leung PY, Lee TL, Chan AS. Effectiveness of lifestyle medicine on cognitive functions in mild cognitive impairments and dementia: a systematic review on randomized controlled trials. Ageing Res Rev. 2023;86:101886. https://doi.org/10.1016/j.arr.2023.101886.
Zhou W, Chen D, Hong Z, Fan H, Liu S, Zhang L. The relationship between health-promoting lifestyles and depression in the elderly: roles of aging perceptions and social support. Qual Life Res. 2021;30(3):721–8. https://doi.org/10.1007/s11136-020-02674-4.
Helgadóttir B, Hallgren M, Ekblom Ö, Forsell Y. Training fast or slow? Exercise for depression: a randomized controlled trial. Prev Med. 2016;91:123–31. https://doi.org/10.1016/j.ypmed.2016.08.011.
Rahe C, Baune BT, Unrath M, Arolt V, Wellmann J, Wersching H, et al. Associations between depression subtypes, depression severity and diet quality: cross-sectional findings from the bidirect study. BMC Psychiatry. 2015;15:38. https://doi.org/10.1186/s12888-015-0426-9.
Acknowledgements
We are very grateful for the funding support, as well as the editors and reviewers who worked hard to get the article published. Finally, we are very grateful to Hang Zhao for his support and help.
Funding
This work was supported by the National Social Science Foundation [grant numbers 20CFX017]; the Humanities and Social Sciences Foundation of the Ministry of Education [grant numbers 21YJC820050]; Sichuan Medical and Health Rule of Law Research Center-Chinese Society of Health Law Joint Project [grant numbers YF23-Y07].
Author information
Authors and Affiliations
Contributions
GX participated in writing, data analysis and revision; JZ and XZ conceived the idea for the writing; CM provided the methodology; WH and YG participated in the statistical analysis; YC cleaned the data; YM reviewed and revised the manuscript. All authors have read and agreed to the published version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was conducted in accordance with the Declaration of Helsinki, and approved by the Research Ethics Boards of Peking University and Duke University (IRB00001052-13074).
Informed consent
Obtained from all the elderly involved in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Xian, G., Chai, Y., Gong, Y. et al. The relationship between healthy lifestyles and cognitive function in Chinese older adults: the mediating effect of depressive symptoms. BMC Geriatr 24, 299 (2024). https://doi.org/10.1186/s12877-024-04922-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-024-04922-5