Abstract
Background
Clinical evidence demonstrating a longitudinal association between prescribed medications and sarcopenia onset is lacking. We investigated the association of polypharmacy (the use of five or more medications) and potentially inappropriate medications (PIMs) with sarcopenia risk in community-dwelling older adults.
Methods
In this longitudinal population-based cohort study, 2,044 older residents with no long-term care needs were randomly selected from a community in Kashiwa, Japan. Baseline data collection was conducted in 2012, with follow-ups in 2013, 2014, 2016, 2018, and 2021. Prescribed medications and PIMs (drugs listed in the Screening Tool for Older Person’s Appropriate Prescriptions for the Japanese or potentially muscle-wasting drugs) were identified through interviews. New-onset sarcopenia was identified according to the 2019 criteria of the Asian Working Group for Sarcopenia over a 9-year period and analyzed. We used Cox proportional hazards models to test the longitudinal association of prescribed medications with sarcopenia onset.
Results
Of the 1,549 participants without sarcopenia at baseline (mean age, 72.5 ± 5.5 years; 49.1% women; median and interquartile range, 6.0 [4.0–9.0] years), 230 experienced new-onset sarcopenia during the follow-up. After adjusting for confounders, polypharmacy combined with PIM use was strongly associated with new-onset sarcopenia (adjusted hazard ratio, 2.35; 95% confidence interval, 1.58–3.51; P < 0.001). No significant associations were observed for either PIM use or polypharmacy alone.
Conclusions
Polypharmacy combined with PIM use, but not polypharmacy alone, was associated with an increased risk of new-onset sarcopenia over the 9-year follow-up period among community-dwelling older adults. Limiting polypharmacy and imposing the prescription of appropriate medications may facilitate sarcopenia prevention.
Similar content being viewed by others
Background
Sarcopenia, a common and serious disorder that shortens healthy life expectancy in aging populations, such as those in Japan [1], involves the progressive loss of skeletal muscle with increased risks of adverse health outcomes, including frailty, functional disability, and mortality [1,2,3]. While the prevalence of sarcopenia varies depending on the assessment method and criteria, it is about a little more than 10% among Japanese community-dwelling older adults [4]. Sarcopenia was assigned an individual International Statistical Classification of Diseases and Related Health Problems code (M62.84) in 2016, with Japan publishing clinical practice guidelines in 2018. Considering the aging global population, sarcopenia is increasingly becoming a health care priority.
Adverse drug events have become increasingly common among older adults in outpatient settings, despite often being preventable [5]. Polypharmacy, the prescription of multiple medications, is a primary factor leading to adverse drug events and untoward drug interactions [6, 7]. The prevalence of polypharmacy among older adults is extremely wide-ranging, depending on age, current health status, health care setting, and geography [7]. Epidemiological data suggest that polypharmacy may affect more than one-third of older adults worldwide [8, 9]. Moreover, there is a relationship between polypharmacy and high sarcopenia prevalence, and together, they present a greater risk of frailty [10,11,12]. However, although polypharmacy constitutes a predictor of several adverse clinical outcomes among older adults, including mortality, a systematic review failed to demonstrate this association because key covariates were not considered [6]. Furthermore, as clinical evidence from longitudinal studies regarding the association between polypharmacy and muscle wasting is lacking, it remains unclear whether widely prescribed medications associated with muscle wasting affect sarcopenia development [13, 14]. Thus, data on the longitudinal contribution of the number of prescribed medications to sarcopenia development among those who do not require long-term care are insufficient.
Polypharmacy is considered a “necessary evil” because several clinical conditions necessitate the use of multiple drugs [15]. Thus, it is important to consider not only the number of medications but also the use of potentially inappropriate medications (PIMs) according to individual health conditions. The Japan Geriatrics Society published guidelines reflecting the current medical and medication situation in Japan, which were revised in 2015 as the “Screening Tool for Older Person’s Appropriate Prescriptions for the Japanese” (STOPP-J) [16]. Among Japanses older adults, the prevalnce of PIMs determined by STOPP-J was 41.9%, with higher frequencies among older adults, long-term care insurance users, and polypharmacy [17].Notably, some oral drugs such as statins, sulfonylureas (reiterated), and glinides may be associated with muscle wasting [13]. Moreover, age-associated physiological changes can alter drug disposition, and pathophysiological changes in older adults at risk of developing sarcopenia (e.g., body weight, body composition, protein synthesis) may lead to even greater heterogeneity in pharmacokinetics [18]. However, whether polypharmacy or PIM use is negatively associated with new-onset sarcopenia in community-dwelling older adults remains unclear.
Understanding whether the number of prescribed medications is related to sarcopenia development in community-dwelling older adults could facilitate longer and healthier living, even in consideration of the causal effects of PIM use. Thus, in this study, our aim was to evaluate whether polypharmacy, PIM use, or their combination is associated with a higher risk of sarcopenia over a 9-year follow up period in community-dwelling older adults not requiring long-term care.
Methods
Study setting and participants
We employed data from a longitudinal prospective cohort study conducted in Kashiwa, Japan, designed to identify important factors affecting healthy aging in community-dwelling older adults [19]. Urban and rural communities are intermingled in this area. In 2012, we randomly selected 12,000 adults aged 65 years and older with no long-term care needs from the registry of Kashiwa, Japan and sent invitations for participation in the study via mail. A total of 2,044 older adults (1013 men and 1031 women) agreed to participate. The participants reflected the age distribution in Kashiwa for each sex. Baseline data were collected between September and November 2012 at welfare and community centers. Exclusion criteria included (i) cognitive impairment (Mini–Mental State Examination [MMSE] score < 18), (ii) sarcopenia at baseline, (iii) an implanted pacemaker (prohibiting bioelectrical impedance analysis for sarcopenia diagnosis), (iv) missing any follow-up studies, and (v) missing data on sarcopenia or medications. Follow-ups in 2013, 2014, 2016, 2018, and 2021 were performed to examine the longitudinal association between prescribed medications and new-onset sarcopenia. The study followed the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines for cohort studies.
The ethics committee of the University of Tokyo Life Science Research Center approved the study protocol (#21–192). Written informed consent was obtained from all participants. This study was conducted in accordance with the tenets of the Declaration of Helsinki.
Prescribed medications and chronic diseases
Currently prescribed medication names and numbers were determined via face-to-face interviews conducted by trained nurses using a standardized questionnaire. Participants who used a prescription record note were requested to bring the note during assessment. In this study, we defined ≥ 5 drug prescriptions as polypharmacy. The number of prescribed medications were reassessed in all follow-up surveys. The number of prescribed medications was re-examined at all follow-up visits and excluded from polypharmacy when the number of prescribed medications major decreased; PIMs were defined as STOPP-J-listed drugs or potentially muscle-wasting drugs. The investigated medications were thus classified as “PIMs” or “not PIMs.”
STOPP-J drugs were classified into 19 categories and 28 subcategories; the categories consisted of antipsychotics, hypnotics, antidepressants, sulpiride, anti-Parkinson drugs, steroids, antithrombotic drugs (antiplatelet drugs and anticoagulants), digitalis, diuretics, β-blockers, α-blockers, first-generation H1 receptor antagonists, H2 receptor antagonists, antiemetics, laxatives, antidiabetic drugs, insulin, overactive bladder medications, and non-steroidal anti-inflammatory drugs (NSAIDs). As antipsychotics, selective serotonin reuptake inhibitor antidepressants, steroids, digitalis, β-blockers, and laxatives are considered PIMs in STOPP-J only in certain cases or in certain patient subsets (e.g., laxative use among patients with impaired renal function); they were excluded from this study [16]. Sodium–glucose cotransporter 2 (SGLT2) inhibitors were also excluded as they were not available in Japan at study initiation. We also evaluated the use of statins, sulfonylureas (reiterated), and glinides as drugs potentially associated with muscle wasting [13].
Data on current chronic diseases (hypertension, diabetes mellitus, dyslipidemia, osteoporosis, malignant neoplasm, stroke, chronic renal failure, and heart disease) were also obtained during the interviews, with comorbidity defined as the presence of two or more of these.
Sarcopenia
According to the Asian criteria and cut-off threshold (Asian Working Group of Sarcopenia 2019) [16], we diagnosed sarcopenia as low appendicular skeletal muscle mass with concomitant low muscle strength or physical function. Bioimpedance analyses were used to assess low appendicular skeletal muscle mass, defined as < 7.0 and < 5.7 kg/m2 for men and women, respectively, using the InBody 420 body composition analyzer (InBody Japan, Tokyo, Japan) [20]. Low muscle strength (< 28 and < 18 kg, respectively) was measured using a Smedley-type grip strength meter (Grip D dynamometer; Takei Scientific Instruments Co., Ltd., Niigata, Japan) [20]. Low physical function, defined as a normal walking speed of < 1.0 m/s, was determined by measuring the time required to travel 5 m between 11 m lanes [20]. Sarcopenia was remeasured in all follow-up surveys.
Covariates
Covariates included age, sex, body mass index (BMI), education level (college degree or less), living arrangement (alone vs. together), annual income, cognitive function determined using MMSE [21], depressive symptoms determined using the Geriatric Depression Scale-15 (GDS-15) [22], disability of instrumental activities daily living (IADL) [23], exercise habit (at least once weekly during leisure time) evaluated using the Global Physical Activity Questionnaire [24], daily food diversity, and current alcohol habits (responding “yes” to the question “Do you drink alcohol?”). We also collected data on biochemical parameters (i.e., serum albumin, total cholesterol, hemoglobin, C-reactive protein, platelet count, fasting blood glucose, and systolic/ diastolic blood pressure) via medical interviews and blood tests.
Statistical analysis
All statistical analyses were performed using IBM SPSS version 29.0 (IBM Japan, Tokyo, Japan). A two-sided P value of < 0.05 was considered to indicate statistically significant difference. Data are presented as the mean (± standard deviation) or median (interquartile range) for quantitative measures and as the number of subjects (percentage) for all qualitative measures.
Baseline differences in variables among those with/without new-onset sarcopenia were analyzed using the χ2 test or Fisher’s exact test for categorical variables, and unpaired t-test or Mann–Whitney U test for continuous variables. We assessed the baseline association between the number of prescribed medications and PIM use via multivariate logistic regression.
To explore the association between prescribed medications and sarcopenia onset, we assessed the longitudinal association between prescribed medications and sarcopenia onset using the Cox proportional hazards model. We calculated the hazard ratios (HRs) and 95% confidence interval (CI) using a bivariate model and a multivariable model, wherein the ratios were adjusted according to the variation in the following continuous variables: age (years), BMI (kg/m2), cognitive function (MMSE score), depressive symptoms (GDS-15 score), and daily food diversity score. Ratios were also adjusted baseline status for sex, education level (college degree or less), low annual income (either ≥ or < 1.4 million yen per household for men, and 1.2 million yen for women), living arrangement (alone vs. together), exercise habit (yes/no), current alcohol habit (yes/no), and individual chronic conditions (i.e., hypertension, diabetes mellitus, dyslipidemia, osteoporosis, malignant neoplasm, stroke, chronic renal failure, heart disease, and disability of IADL). Multiple imputation using fully conditional specification (chained equations) was applied to impute the missing values for covariates, and 10 datasets were created.
Results
Study participants
A total of 1,549 participants (mean age, 72.5 ± 5.5 years; 49.1% women) were eligible for participation in the present study. Of the 2,044 participants that completed the baseline assessment, 216 were excluded because they failed to meet the inclusion criteria (sarcopenia at baseline, n = 168; pacemaker or missing items; n = 48). Over the 9-year follow-up, 279 individuals were absent from all follow-ups. Over the 9-year follow-up (median year and interquartile range, 6.0 [4.0–9.0] years), 230 individuals (14.8%) experienced sarcopenia development, as determined using criteria from the Asian Working Group of Sarcopenia (AWGS) 2019 (Additional File 1).
Baseline characteristics and outcomes
Table 1 presents the baseline characteristics of the study participants classified according to new-onset sarcopenia experience. Those with higher age, physical weakness (lower handgrip strength and slower gait speed), psychological deterioration (lower cognitive function and depressive symptoms), and lower serum albumin and hemoglobin levels were more likely to exhibit sarcopenia onset; however, differences were minimal for gait speed, cognitive function, depressive symptoms, and blood test results (lower serum albumin, total cholesterol, and hemoglobin level). Regarding chronic diseases, those with hypertension, heart disease, malignant neoplasm, and comorbidity were more likely to develop sarcopenia. Living alone, low income, lack of exercise, drinking, dyslipidemia, and chronic renal failure tended to be associated with new-onset sarcopenia (P < 0.150). No significant differences were found in terms of sex.
Prescribed medications and potentially inappropriate medications
The median number of prescribed medications was 2.0 (interquartile range, 0–4; range, 0–17), whereas 428 (27.6%) individuals had no prescribed medications. The frequency of PIM use and the longitudinal association with sarcopenia onset is summarized in Additional File 2. According to the STOPP-J criteria, 436 (28.1%) individuals were prescribed PIMs, and 381 (24.6%) were prescribed potentially muscle-wasting drugs. Benzodiazepines and NSAIDs were the most commonly prescribed drugs matching the STOPP-J criteria; statins were the most commonly prescribed potentially muscle-wasting drugs. Only NSAIDs, muscarinic receptor antagonists, and statins were significantly associated with sarcopenia onset.
The association between the number of prescribed medications and use of PIMs, such as drugs listed in STOPP-J and potentially muscle-wasting drugs, at baseline are summarized in Additional File 3. Compared to the proportion of individuals with one prescription, the proportion of individuals prescribed PIMs increased significantly with an increase in the number of prescriptions, exceeding 50% for individuals with ≥ 4 prescriptions. The inclusion rate of potential muscle-weakening drugs was also significantly higher for individuals prescribed ≥ 5 drugs. Therefore, our definition of ≥ 5 drug prescriptions as polypharmacy, consistent with the definition of a previous study [25], representing 367 (23.7%) participants.
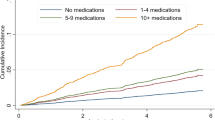
Prescribed medications and sarcopenia onset
Next, we examined whether polypharmacy, PIM use, and potential muscle-wasting drug use were individually associated with new-onset sarcopenia over the 9-year follow-up. The covariate-adjusted hazard ratios and 95% CIs of sarcopenia onset based on prescribed medications are presented in Table 2. After adjusting for covariates, older adults with polypharmacy tended to have an increased frequency of new-onset sarcopenia (25.6% vs. 11.5%), along with a large adjusted hazard ratio compared with those without polypharmacy. The use of STOPP-J-listed drugs and potentially muscle-wasting drugs tended to be associated with sarcopenia development.
Furthermore, we tested whether polypharmacy combined with the use of PIMs (drugs listed in STOPP-J or potential muscle-wasting drugs) was associated with sarcopenia development. Overall, 76.6% of older adults on polypharmacy also utilized PIMs, which was strongly correlated with new-onset sarcopenia. Neither polypharmacy nor PIM use alone was significantly associated with sarcopenia development.
Discussion
In this longitudinal cohort study, we examined the prescribed medications, chronic diseases, and physical and psychological status of individuals to identify whether polypharmacy is associated with an increased risk of sarcopenia development over a 9-year period among community-dwelling older adults with no long-term care needs. After adjusting for multifaceted confounders, polypharmacy combined with the use of STOPP-J-listed PIMs or potentially muscle-wasting drugs, but not polypharmacy alone, was significantly associated with an increased HR of sarcopenia onset.
To the best of our knowledge, our study provides the first evidence of the possibility of a longitudinal association between polypharmacy combined with PIMs and sarcopenia development among community-dwelling older adults. Similarly, a previous cross-sectional study reported that polypharmacy (≥ 5 medications) in older adults was associated with a 2.2-fold higher prevalence of sarcopenia based on low appendicular lean mass [10]. Our results are consistent with the findings from previous observational studies in other populations showing associations between polypharmacy and adverse geriatric outcomes, such as frailty, sarcopenia, and mortality [6, 10,11,12, 26].
Several possible explanations exist for the longitudinal association between polypharmacy and new-onset sarcopenia. First, older adults have an increased risk of adverse drug reactions (ADRs) because of age-related changes in pharmacokinetics, such as absorption, bioavailability, distribution, metabolism, and excretion [27]. Previous review informs the impact of chronological aging and various geriatric syndromes on drug disposition, and there is some evidence that changes in body weight and composition as well as protein synthesis affect drug distribution and metabolism [28]. Thus, poor pharmacokinetics may enhance the adverse outcomes of polypharmacy and long-term dosing.
Second, polypharmacy is strongly associated with PIM use [29], prescribing cascades [30], and low adherence [31]. A prescribing cascade occurs when nonspecific signs and symptoms of ADRs are misinterpreted as disease, and further medications are prescribed to treat the misinterpreted conditions. Unfortunately, because the symptoms caused by polypharmacy usually mimic those of aging, such as depressive symptoms [32], cognitive decline [33], and frailty [11, 12], the probability of prescribing cascades is higher among older adults exhibiting frailty. Thus, prescribing cascades can lead to the prescription of PIMs [30]. Our results also showed that individuals with polypharmacy were also prescribed PIMs or potentially muscle-wasting drugs, suggesting that polypharmacy may be linked to overmedication. Participants with new-onset sarcopenia were not only older at baseline but also exhibited lower physical and cognitive function, as well as more depressive symptoms. It is conceivable that psychological characteristics contributed to the lower adherence. These negative influences can explain why polypharmacy is associated with preventable and unplanned hospitalization [6, 34] and ADRs [5, 6, 35]. Our results showed that the risks of sarcopenia did not increase until ≥ 5 medications were used, supporting previous findings that older Japanese adults taking ≥ 6 medications were more likely to experience ADRs [36]. Therefore, in individuals with polypharmacy, the high risk of ADRs associated with age-related changes in pharmacokinetics, PIMs, and low adherence to prescribed medications could explain the increased risks of adverse outcomes.
Furthermore, we found that PIMs or potentially muscle-wasting drug use tended to be associated with increased sarcopenia risk. In addition to medication number and possible inter-drug interactions, the types of drugs used may directly or indirectly affect sarcopenia. For example, some drugs may negatively affect muscles, inducing eating disorders, or may lead to weight loss, which influences body composition [13, 14]. Potentially muscle-wasting drugs, such as statins, can cause muscle toxicity, whereas other PIMs (e.g., glucocorticoids, β blockers, and NSAIDs) may have detrimental metabolic effects. Statins may also induce serious adverse effects, including elevated liver enzymes and skeletal muscle abnormalities, ranging from benign myalgias to severe rhabdomyolysis [13, 14], potentially derived from mitochondrial dysfunction, alterations in apoptosis-related gene expression, protein degradation, and genetic predisposition. Such mechanisms are also involved in sarcopenia pathogenesis and may underlie the association between statins and sarcopenia. Furthermore, the use of PIMs such as benzodiazepine constitutes a risk factor for adverse health outcomes and may be contraindicated for long-term use [37,38,39]. Therefore, despite the benefits of appropriate medications for older individuals, the prescription of too many medications, including PIMs, may negatively influence geriatric endpoints such as sarcopenia. Consistently, after adjustment for potential confounders, including time-varying factors, we observed that polypharmacy with PIMs was significantly associated with sarcopenia development, thereby explaining the longitudinal association between polypharmacy combined with PIMs and increased sarcopenia risk over a 9-year period.
This study has some limitations. First, although we adjusted for several confounding factors, some biases may have remained owing to unobserved medical conditions or altered renal or liver function. Second, information on the duration of drug treatment or medication adherence was lacking. As such, the exact doses of the prescribed medications were unknown. Third, ADR occurrence, medication underuse, and medication duplication were not assessed. Fourth, the number of medications was evaluated at each follow-up and confirmed that the number of medications did not decrease dramatically, but PIMs could not be evaluated at each follow-up. Fifth, further prospective randomized control trials are necessary to evaluate the potential benefits of de-prescribing on sarcopenia risk. Notably, this study included a sample of community-dwelling older adults who participated through randomization, for whom health awareness is expected to be high, and the population representativeness is relatively high; consequently, the generalizability of the results is high. However, further research is required to determine whether similar results would be obtained in countries with different healthcare supply systems.
Conclusions
In this longitudinal study, we evaluated whether the number and type of prescribed medications are associated with increased sarcopenia risk among community-dwelling older adults. After adjustment for time-varying confounders, polypharmacy combined with PIM use was associated with an increased risk of sarcopenia onset over a 9-year follow-up period. Our results suggest that the appropriateness of multiple drug prescriptions should be thoroughly evaluated, particularly among individuals with polypharmacy. Efforts to structurally manage and advocate for appropriate drug prescribing, taking into account the characteristics of geriatric syndromes such as sarcopenia, may help prevent sarcopenia.
Data availability
The datasets generated and analyzed during the current study are not publicly available due them containing information that could compromise research participant privacy or consent but are available from the corresponding author on reasonable request.
Abbreviations
- ADRs:
-
adverse drug reactions
- AWGS:
-
Asian Working Group of Sarcopenia
- BMI:
-
body mass index
- HR:
-
hazard ratio
- OR:
-
odds ratio
- CI:
-
confidence interval
- GDS-15:
-
Geriatric Depression Scale-15
- MMSE:
-
Mini–Mental State Examination
- NSAID:
-
non-steroidal anti-inflammatory drug
- HR:
-
hazard ratio
- PIM:
-
potentially inappropriate medication
- SGLT2:
-
sodium–glucose cotransporter 2
- STOPP-J:
-
Screening Tool for Older Person’s Appropriate Prescriptions for the Japanese
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology.
References
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, et al. Sarcopenia in Asia: consensus report of the asian Working Group for Sarcopenia. J Am Med Dir Assoc. 2014;15:95–101. https://doi.org/10.1016/j.jamda.2013.11.025.
Kelley GA, Kelley KS. Is sarcopenia associated with an increased risk of all-cause mortality and functional disability? Exp Gerontol. 2017;96:100–3. https://doi.org/10.1016/j.exger.2017.06.008.
Hirani V, Blyth F, Naganathan V, Le Couteur DG, Seibel MJ, Waite LM, et al. Sarcopenia is associated with incident disability, institutionalization, and mortality in community-dwelling older men: the Concord Health and Ageing in Men Project. J Am Med Dir Assoc. 2015;16:607–13. https://doi.org/10.1016/j.jamda.2015.02.006.
Kitamura A, Seino S, Abe T, Nofuji Y, Yokoyama Y, Amano H, et al. Sarcopenia: prevalence, associated factors, and the risk of mortality and disability in japanese older adults. J Cachexia Sarcopenia Muscle. 2021 Feb;12(1):30–8. https://doi.org/10.1002/jcsm.12651.
Gurwitz JH, Field TS, Harrold LR, Rothschild J, Debellis K, Seger AC, et al. Incidence and preventability of adverse drug events among older persons in the ambulatory setting. JAMA. 2003;289:1107–16. https://doi.org/10.1001/jama.289.9.1107.
Fried TR, O’Leary J, Towle V, Goldstein MK, Trentalange M, Martin DK. Health outcomes associated with polypharmacy in community-dwelling older adults: a systematic review. J Am Geriatr Soc. 2014;62:2261–72. https://doi.org/10.1111/jgs.13153.
Akishita M, Arai H, Arai H, Inamatsu T, Kuzuya M, Suzuki Y, et al. Survey on geriatricians’ experiences of adverse drug reactions caused by potentially inappropriate medications: commission report of the Japan Geriatrics Society. Geriatr Gerontol Int. 2011;11:3–7. https://doi.org/10.1111/j.1447-0594.2010.00631.x.
Midão L, Giardini A, Menditto E, Kardas P, Costa E. Polypharmacy prevalence among older adults based on the survey of health, ageing and retirement in Europe. Arch Gerontol Geriatr 2018 Sep-Oct;78:213–20. doi: https://doi.org/10.1016/j.archger.2018.06.018.
Pazan F, Wehling M. Polypharmacy in older adults: a narrative review of definitions, epidemiology and consequences. Eur Geriatr Med. 2021 Jun;12(3):443–52. https://doi.org/10.1007/s41999-021-00479-3.
König M, Spira D, Demuth I, Steinhagen-Thiessen E, Norman K. Polypharmacy as a risk factor for clinically relevant sarcopenia: results from the Berlin Aging Study II. J Gerontol A Biol Sci Med Sci. 2017;73:117–22. https://doi.org/10.1093/gerona/glx074.
Veronese N, Stubbs B, Noale M, Solmi M, Pilotto A, Vaona A, et al. Polypharmacy is associated with higher frailty risk in older people: an 8-year longitudinal cohort study. J Am Med Dir Assoc. 2017;18:624–8. https://doi.org/10.1016/j.jamda.2017.02.009.
Saum KU, Schöttker B, Meid AD, Holleczek B, Haefeli WE, Hauer K, et al. Is polypharmacy associated with frailty in older people? Results from the Esther Cohort Study. J Am Geriatr Soc. 2017;65:e27–32. https://doi.org/10.1111/jgs.14718.
Campins L, Camps M, Riera A, Pleguezuelos E, Yebenes JC, Serra-Prat M. Oral drugs related with muscle wasting and sarcopenia. A review. Pharmacology. 2017;99:1–8. https://doi.org/10.1159/000448247.
Pana A, Sourtzi P, Kalokairinou A, Velonaki VS. Sarcopenia and polypharmacy among older adults: a scoping review of the literature. Arch Gerontol Geriatr. 2022;98:104520. https://doi.org/10.1016/j.archger.2021.104520.
Wise J. Polypharmacy: a necessary evil. BMJ. 2013;347:f7033. https://doi.org/10.1136/bmj.f7033.
Kojima T, Mizukami K, Tomita N, Arai H, Ohrui T, Eto M, et al. Screening tool for older persons’ appropriate prescriptions for japanese: report of the Japan Geriatrics Society Working Group on “Guidelines for medical treatment and its safety in the elderly. Geriatr Gerontol Int. 2016;16:983–1001. https://doi.org/10.1111/ggi.12890.
Kojima T, Hamaya H, Ishii S, Hattori Y, Akishita M. Association of disability level with polypharmacy and potentially inappropriate medication in community dwelling older people. Arch Gerontol Geriatr. 2023 Mar;106:104873. https://doi.org/10.1016/j.archger.2022.104873.
Maher D, Ailabouni N, Mangoni AA, Wiese MD, Reeve E. Alterations in drug disposition in older adults: a focus on geriatric syndromes. Expert Opin Drug Metab Toxicol. 2021;17:41–52. https://doi.org/10.1080/17425255.2021.1839413.
Tanaka T, Takahashi K, Hirano H, Kikutani T, Watanabe Y, Ohara Y, et al. Oral frailty as a risk factor for physical frailty and mortality in community-dwelling elderly. J Gerontol A Biol Sci Med Sci. 2018;73:1661–7. https://doi.org/10.1093/gerona/glx225.
Chen LK, Woo J, Assantachai P, Auyeung TW, Chou MY, Iijima K, et al. Asian Working Group for Sarcopenia: 2019 consensus update on sarcopenia diagnosis and treatment. J Am Med Dir Assoc. 2020;21:300–7. e2 e302.
Folstein MF, Folstein SE, McHugh PR. Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. https://doi.org/10.1016/0022-3956(75)90026-6.
Schreiner AS, Hayakawa H, Morimoto T, Kakuma T. Screening for late life depression: cut-off scores for the geriatric Depression Scale and the Cornell Scale for Depression in Dementia among japanese subjects. Int J Geriatr Psychiatry. 2003;18:498–505. https://doi.org/10.1002/gps.880.
Koyano W, Shibata H, Nakazato K, Haga H, Suyama Y. Measurement of competence: reliability and validity of the TMIG Index of competence. Arch Gerontol Geriatr. 1991;13(2):103–16. https://doi.org/10.1016/0167-4943(91)90053-s.
Cleland CL, Hunter RF, Kee F, Cupples ME, Sallis JF, Tully MA. Validity of the global physical activity questionnaire (GPAQ) in assessing levels and change in moderate-vigorous physical activity and sedentary behaviour. BMC Public Health. 2014;14:1255. https://doi.org/10.1186/1471-2458-14-1255.
Masnoon N, Shakib S, Kalisch-Ellett L, Caughey GE. What is polypharmacy? A systematic review of definitions. BMC Geriatr. 2017;17:230. https://doi.org/10.1186/s12877-017-0621-2.
Richardson K, Ananou A, Lafortune L, Brayne C, Matthews FE. Variation over time in the association between polypharmacy and mortality in the older population. Drugs Aging. 2011;28:547–60. https://doi.org/10.2165/11592000-000000000-00000.
Blackford MS. Drug therapy in older adults: effects of altered pharmacokinetics and pharmacodynamics (continuing education credit). Ohio Nurses Rev. 1995;70:13–7. quiz 19.
Maher D, Ailabouni N, Mangoni AA, Wiese MD, Reeve E. Alterations in drug disposition in older adults: a focus on geriatric syndromes. Expert Opin Drug Metab Toxicol 2021 Jan;17(1):41–52. doi: https://doi.org/10.1080/17425255.2021.1839413.
Guthrie B, McCowan C, Davey P, Simpson CR, Dreischulte T, Barnett K. High risk prescribing in primary care patients particularly vulnerable to adverse drug events: cross sectional population database analysis in scottish general practice. BMJ. 2011;342:d3514. https://doi.org/10.1136/bmj.d3514.
Rochon PA, Gurwitz JH. Optimising drug treatment for elderly people: the prescribing cascade. BMJ. 1997;315:1096–9. https://doi.org/10.1136/bmj.315.7115.1096.
Lyles A, Culver N, Ivester J, Potter T. Effects of health literacy and polypharmacy on medication adherence. Consult Pharm. 2013;28:793–9. https://doi.org/10.4140/TCP.n.2013.793.
Holvast F, van Hattem BA, Sinnige J, Schellevis F, Taxis K, Burger H, et al. Late-life depression and the association with multimorbidity and polypharmacy: a cross-sectional study. Fam Pract. 2017;34:539–45. https://doi.org/10.1093/fampra/cmx018.
Niikawa H, Okamura T, Ito K, Ura C, Miyamae F, Sakuma N, et al. Association between polypharmacy and cognitive impairment in an elderly japanese population residing in an urban community. Geriatr Gerontol Int. 2017;17:1286–93. https://doi.org/10.1111/ggi.12862.
Leendertse AJ, Egberts AC, Stoker LJ, van den Bemt PM, HARM Study Group. Frequency of and risk factors for preventable medication-related hospital admissions in the Netherlands. Arch Intern Med. 2008;168:1890–6. https://doi.org/10.1001/archinternmed.2008.3.
Bourgeois FT, Shannon MW, Valim C, Mandl KD. Adverse drug events in the outpatient setting: an 11-year national analysis. Pharmacoepidemiol Drug Saf. 2010;19:901–10. https://doi.org/10.1002/pds.1984.
Kojima T, Akishita M, Kameyama Y, Yamaguchi K, Yamamoto H, Eto M, et al. High risk of adverse drug reactions in elderly patients taking six or more drugs: analysis of inpatient database. Geriatr Gerontol Int. 2012;12:761–2. https://doi.org/10.1111/j.1447-0594.2012.00868.x.
American Geriatrics Society Beers Criteria Update Expert Panel. American Geriatrics Society 2015 updated beers criteria for potentially inappropriate medication use in older adults. J Am Geriatr Soc. 2015;63:2227–46. https://doi.org/10.1111/jgs.13702.
Glass J, Lanctôt KL, Herrmann N, Sproule BA, Busto UE. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ. 2005;331:1169. https://doi.org/10.1136/bmj.38623.768588.47.
O’Mahony D, O’Sullivan D, Byrne S, O’Connor MN, Ryan C, Gallagher P. STOPP/START criteria for potentially inappropriate prescribing in older people: version 2. Age Ageing. 2015;44:213–8. https://doi.org/10.1093/ageing/afu145.
Acknowledgements
The authors thank all staff members at the study locations and the study participants. We would like to thank Editage (http://www.editage.com) for English language editing and reviewing of this manuscript.
Funding
This work was supported by the Health and Labor Sciences Research Grant (grant number H24-Choju-Ippan-002) from the Ministry of Health, Labor, and Welfare of Japan. The financial sponsor had no role in the design, methods, subject recruitment, data collections, analysis, and preparation of the paper.
Author information
Authors and Affiliations
Contributions
Study concept and design: Tomoki Tanaka, Masahiro Akishita, and Katsuya IijimaAcquisition of subjects: Tomoki Tanaka, Masahiro Akishita, and Katsuya IijimaData analysis and interpretation: Tomoki Tanaka, Masahiro Akishita, Taro Kojima, Bo-Kyung Son, and Katsuya Iijima. Manuscript preparation: Tomoki Tanaka, Masahiro Akishita, Taro Kojima, Bo-Kyung Son, and Katsuya Iijima.All authors reviewed the manuscript. The corresponding author (Katsuya Iijima) attests that all listed authors meet the authorship criteria and that no others meeting the criteria have been omitted. All authors affirm that the manuscript is an honest, accurate, and transparent account of the study being reported; that no important aspects of the study have been omitted; and that any discrepancies from the study as originally planned have been explained.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethics committee of the University of Tokyo Life Science Research Center approved the study protocol (#21–192). Written informed consent was obtained from all participants. This study was conducted in accordance with the tenets of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tanaka, T., Akishita, M., Kojima, T. et al. Polypharmacy with potentially inappropriate medications as a risk factor of new onset sarcopenia among community-dwelling Japanese older adults: a 9-year Kashiwa cohort study. BMC Geriatr 23, 390 (2023). https://doi.org/10.1186/s12877-023-04012-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-023-04012-y