Abstract
Background
Phosphate disturbances are relatively common in hospitalized patients, especially in critically ill patients. The abnormal phosphate levels may indicate an abnormal body condition. However, little is known about the association between elevated serum phosphate and outcome in critically ill elderly patients. Therefore, the purpose of the present study was to investigate the association between early elevated phosphate and mortality in critically ill elderly patients.
Methods
The present study was a retrospective cohort study based on the medical information mart for intensive care IV (MIMIC-IV) database. Patients with age ≥60 years old were enrolled in the present study. The primary outcome in the present study was ICU mortality. Univariate and multivariate Cox proportional hazard regression analyses were used to evaluate the association between early elevated phosphate and ICU mortality in critically ill elderly patients.
Results
Twenty-four thousand two hundred eighty-nine patients were involved in this analysis and 2,417 patients died in ICU. The median age of involved patients was 78.4 (67.5, 82.9) years old. The median level of serum phosphate in the survivor group was 3.6 (3.0, 4.3) mg/dL, and the median level of serum phosphate in the non-survivor group was 4.4 (3.4, 5.8) mg/dL. The level of serum phosphate in the non-survivor group was significantly higher than the survivor group (4.4 vs. 3.6, P<0.001). The multivariate Cox proportional hazard regression demonstrated that elevated phosphate was an independent risk factor for ICU mortality, after adjustment for other covariates (HR=1.056, 95%CI: 1.028-1.085, P<0.001).
Conclusions
In critically ill elderly patients, early elevated phosphate was significantly associated with increased ICU mortality.
Similar content being viewed by others
Background
Critically ill elderly patients are important components in critically ill patients in the intensive care unit (ICU). As an aging population, the number of critically ill elderly patients admitting to ICU is quickly increasing. The proportion of critically ill elderly patients was up to 20–30 percent of all admissions [1,2,3]. Why do we pay more attention to elderly patients? Because patients with old age tend to develop chronic illness and functional impairment, or generate poor outcomes [4,5,6]. Therefore, elderly patients, especially elderly critically patients require more concentration by physicians and careful treatments.
The development of electrolyte disorders is common in critically ill patients, such as hyponatremia, hypernatremia, hypomagnesemia, hyperkalemia, and the like [7]. These electrolyte disorders usually were reported to be associated with increased poor outcomes in critically ill patients, or be useful biomarkers for outcomes prediction [8,9,10]. Serum phosphate disturbances also belong to electrolyte disorders and develop frequently in hospitalized patients. Serum phosphate level elevates due to excretion by the kidney diminishes, especially in patients with kidney function injury [11,12,13]. Because critically ill patients develop organ failure including kidney injury frequently, serum phosphate disturbances are common in critically ill patients [14,15,16]. Thongprayoon and her (his) colleagues reported that admission hyperphosphatemia increased the risk of acute kidney injury in hospitalized patients [17]. George and her (his) colleagues found that hyperphosphatemia was also associated with an increased risk for mortality in severe burns [18]. Thus, Serum phosphate disturbances including hyperphosphatemia were a potential risk factor for poor outcomes in hospitalized patients.
Even though some related studies about serum phosphate were conducted and investigated that abnormal serum phosphate level was an independent risk factor for the development of poor outcomes in hospitalized patients, the relationship between serum phosphate on ICU admission and the mortality in critically ill elderly patients has not been explored and validated based on the big data. Therefore, the present study was designed and conducted based on the medical information mart for intensive care IV (MIMIC-IV) database to investigate the association between early serum phosphate on ICU admission and ICU mortality in critically ill patients.
Material and methods
Database source
Medical information mart for intensive care IV (MIMIC-IV, version 1.0) database is a single-center and big database containing real hospital stays for patients admitted to a tertiary academic medical center from 2008 to 2019 in Boston, MA, USA [19]. The MIMIC-IV database contains three modules including MIMIC-IV-Core, MIMIC-IV-Hosp, and MIMIC-IV-ICU. Patient demographics, clinical measurements, laboratory tests, treatments, pharmacotherapy, medical data, survival data, and more were included in the MIMIC-IV database. The researchers completing and passing the required training course could acquire access to this database. The consent for original data acquisition was obtained and the institutional review boards of the Massachusetts Institute of Technology and Beth Israel Deaconess Medical Center approved the establishment of the database. Therefore, patient informed consent and ethics approval were exempted for the present study. Data collected and presented in the present study were extracted by the author Yang and Cheng who completed and passed the required training course.
Study population and data collection
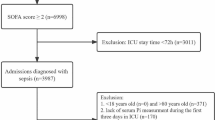
The present retrospective cohort study was conducted based on the MIMIC-IV database. Patients were included in the present study if they were older than 60 years old and with available serum phosphate measurement records upon ICU admission within 24 hours. Patients were excluded if their length of ICU stay was less than 24 hours.
Patient medical data was extracted using PostgreSQL tools (version 13.0). The data including patient demographics and characteristics, signs and symptoms, laboratory findings, and treatment were collected when ICU admission within 24 hours. Of them, the maximum values of serum phosphate during the first 24 hours after ICU admission were included in the analysis. Patient outcomes were followed up in each ICU stay. The primary outcome in the present study was ICU mortality after 24 hours on ICU admission and the secondary outcomes were the length of ICU stay.
Statistical analysis
Baseline characteristics and other clinical variables were compared between the survivors group and non-survivors group. Continuous variables were presented as mean ± standard deviation (SD) or median and interquartile range (IQR) according to their different distributions. A two-sample independent t-test was used for normal distribution or Mann–Whitney U test was used for non-normal distribution to compare differences between two groups. Categorical variables were presented as numbers and percentages, and compared by Chi-square test or Fisher’s exact probability test as appropriate. Univariate and multivariate COX proportional hazard regression analyses (variables presenting P<0.05 were included in multivariate regression analysis) were used to identify the association between early serum phosphate level and ICU mortality in critically ill elderly patients. The Lowess smoothing was also used to explore the curve relationship between serum phosphate level and ICU mortality. The receiver operator characteristic curve (ROC) and area under the curve (AUC) were used to evaluate the performance of early serum phosphate for prediction and calculate the cutoff value. The adjusted model using restricted cubic spline with 4 knots was conducted to flexibly represent the association between the hazard ratio and early serum phosphate as a continuous variable, using a reference level of the cutoff value of phosphate. The correlation between serum phosphate level and sequential organ failure assessment (SOFA) score was investigated using Spearman correlation analysis. P<0.05 was considered statistically significant in comparing differences between two groups, Cox proportional hazard regression models, and correlation analysis. All statistical analyses were performed by SPSS (version 22.0), STATA (version 16.0), and R software (version 4.0.4).
Results
A total of 47,382 critically patients received an assessment. There were 24,289 critically ill elderly patients included in the present study and 2,147 patients died in ICU (Fig. 1). The median age of all patients was 74.8 years old and the non-survivors group was significantly older than the survivors group (76.7 vs. 74.5, P<0.001). The median SOFA score in the non-survivors group was significantly higher than the survivors group (11.0 vs. 5.0, P<0.001). As well as the SOFA score, the Charlson score indicating patient comorbidities was also higher in the non-survivors group (7.0 vs. 6.0, P<0.001). Other comparisons of demographics and clinical characteristics between the non-survivors group and survivors were also compared in Table 1.
Table 2 demonstrated the results of univariate and multivariate Cox proportional hazard regression analyses. Early elevated serum phosphate was independently associated with increased ICU mortality in critically ill elderly patients (HR=1.056, 95%CI: 1.028-1.085, P<0.001) after adjustment other covariates and this result confirmed our hypothesis. Figure 2 using the Lowess smoothing also explored the curve relationship between early serum phosphate and ICU mortality. An elevated curve relationship between early serum phosphate and ICU mortality in critically ill elderly patients was found.
We further conducted ROC and AUC to evaluate the predictive performance of early serum phosphate and calculate the cutoff value. Figure 3 demonstrated the results of ROC and AUC (AUC=0.67) and the cutoff value of serum phosphate was 4.3mg/dL. According to the cutoff value calculated, the survival rates between the high-phosphate group (≥4.3 mg/dL) and the low-phosphate group (<4.3 mg/dL) were compared using the log-rank test. Figure 4 demonstrated that survival probability in the low-phosphate group was significantly higher than the high-phosphate group (P<0.001). The restricted cubic spline model was also used to investigate the potential non-linear association between early different serum phosphate levels and risk of ICU mortality better. There was an elevated curve observed in restricted cubic spline for the association between early serum phosphate and risk of ICU mortality (Fig. 5). Figure 6 showed that phosphate levels of non-survivors in each day within the first 7 days were significantly higher than survivors. Admission serum phosphate was positively correlated with the SOFA score (Fig. 7), but the correlation was very poor.
Association between early serum phosphate as a continuous variable and risk of ICU mortality of critically ill elderly patients. The analysis used a restricted cubic spline model with adjustment for age, SOFA score, Charlson index, respiratory rate, heart rate, mean arterial pressure, SpO2, WBC count, hemoglobin, urea, anion gap, AKI, and dialysis treatment. The reference (hazard ratio = 1, horizontal dotted line) was a serum phosphate of 4.3 mg/dL (vertical dotted line)
Discussion
The ICU mortality in critically ill elderly patients in the present study was 9.95% and this mortality was similar to other investigations reported [20, 21]. Because serum phosphate changes in hospitalized patients were common, we designed and conducted this retrospective cohort study to explore the association between early serum phosphate level and ICU mortality in critically ill elderly patients based on the large-sample database. The present study demonstrated that early elevated serum phosphate was associated with an increased risk of death in critically ill elderly patients. The result of Lowess smoothing further showed that ICU mortality increased along with serum phosphate elevating. The AUC of early serum phosphate predicting mortality was 0.67, and indicated that serum phosphate was not a good predictor in elderly critically patients and might combine with other predicters to obtain a good predictive performance. The restricted cubic spline model adjusted for related covariates was further conducted to better investigate the potential non-linear association between early different serum phosphate levels and risk of ICU mortality.
Phosphate balance is maintained due to body intake and output, and it is necessary for cell metabolism and cell function [22]. Phosphate intake is along the gastrointestinal tract through two different routes: the passive paracellular route and the active transcellular route [13]. When the body lacks phosphate, enteral absorption is very efficient to enable the body to maintain an optimal phosphate level. However, body balance could be disturbed due to different disease statuses. Electrolyte and mineral homeostasis disorders commonly occur in hospitalized patients. These electrolyte disorders including serum phosphate disturbances occurred more frequently in critically ill patients due to organ dysfunction [23, 24].
Haider and her (his) colleagues conducted a cross-sectional study, and found that hyperphosphatemia was usual in patients in the emergency room and associated with patient mortality [25]. Two studies conducted by Miller and HarbiIn reported that hyperphosphatemia was also associated with increased mortality in patients with mechanical ventilation or sepsis [24, 26]. In the present study, early serum phosphate in the non-survivors group was significantly higher than survivors and was independently associated with ICU mortality in critically ill elderly patients. These results indicated that early phosphate disturbance was also common in critically ill patients with elderly age and was a risk factor for poor outcomes. Therefore, physicians should pay more attention to changes of early serum phosphate in critically ill elderly patients.
The multivariate analysis also showed that the SOFA score (HR=1.122, 95%CI: 1.110-1.134) and Charlson comorbidity index (HR=1.054, 95%CI: 1.037-1.072) had a more powerful or similar association with ICU mortality, compared with serum phosphate (HR=1.056, 95%CI: 1.028-1.085). These results could be normal and accepted. The SOFA score is a sequential organ failure assessment score to describe organ dysfunction/failure including the respiratory system, cardiovascular system, coagulation system, liver, renal, and CNS [27]. It is a composite index that can reflect patient one or more organ failure and the SOFA score was more comprehensive than other indicators. Thus, the multivariate analysis in the present study showed SOFA score had a more powerful association with ICU mortality. Same as the SOFA score, the Charlson comorbidity index is also a composite index to measure comorbid disease status or casemix in health care databases [28]. In addition, the patients enrolled in the present study were elderly critically ill patients and elderly patients were usually with more comorbid diseases. Therefore, the Charlson comorbidity index might also have a more powerful or similar association with poor outcomes.
Because the present study conducted was based on a MIMIC-IV database with a large sample, we could adjust for more covariates and get more information. More than that, data in the MIMIC-IV database was collected from 2008 to 2019 and was relatively new. Thus, the result of this study was also much more credible. However, the present study also existed some limitations. Firstly, the present study could not demonstrate a causal relationship due to the design of a retrospective cohort study. Secondly, we only recorded the serum phosphate in the first day of admission and did not collect the phosphate levels at other time points. Thus, we did not have adequate evidence to conclude the possible association between the temporal change of phosphate level and patient poor outcomes. Further prospective large-sample investigations are required to solve these limitations.
Conclusions
In critically ill elderly patients, early elevated serum phosphate was independently associated with increased ICU mortality. Therefore, when patients are on ICU admission and under treatment, clinicians should pay more attention to the change of serum phosphate in critically ill elderly patients.
Availability of data and materials
The datasets used for the analysis in the current study are available from the corresponding author on reasonable request.
Abbreviations
- MIMIC-IV:
-
the medical information mart for intensive care IV
- ICU:
-
intensive care unit
- SD:
-
standard deviation
- IQR:
-
median and interquartile range
- ROC:
-
receiver operator characteristic curve
- AUC:
-
area under the curve
- SOFA:
-
sequential organ failure assessment
References
Le Borgne P, Maestraggi Q, Couraud S, Lefebvre F, Herbrecht J-E, Boivin A, et al. Critically ill elderly patients (≥ 90 years): Clinical characteristics, outcome and financial implications. PloS one. 2018;13(6):e0198360.
Vallet H, Moïsi L, Thomas C, Guidet B, Boumendil A. Acute critically ill elderly patients: What about long term caregiver burden? J Crit Care. 2019;54:180–4.
Docherty AB, Anderson NH, Walsh TS, Lone NI. Equity of Access to Critical Care Among Elderly Patients in Scotland: A National Cohort Study. Crit Care Med. 2016;44(1):3–13.
Unsar S, Sut N. Depression and health status in elderly hospitalized patients with chronic illness. Arch Gerontol Geriatr. 2010;50(1):6–10.
Song X, Macknight C, Latta R, Mitnitski AB, Rockwood K. Frailty and survival of rural and urban seniors: results from the Canadian Study of Health and Aging. Aging Clin Exp Res. 2007;19(2):145–53.
Seckinger J, Dschietzig W, Leimenstoll G, Rob PM, Kuhlmann MK, Pommer W, et al. Morbidity, mortality and quality of life in the ageing haemodialysis population: results from the ELDERLY study. Clin Kidney J. 2016;9(6):839–48.
Manning AM. Electrolyte disorders. Vet Clin North Am Small Anim Pract. 2001;31(6):1289–321.
Umbrello M, Mantovani ES, Formenti P, Casiraghi C, Ottolina D, Taverna M, et al. Tolvaptan for hyponatremia with preserved sodium pool in critically ill patients. Annals Intensive Care. 2016;6(1).
Deheinzelin D, Negri EM, Tucci MR, Salem MZ, Cruz VMD, Oliveira RM, et al. Hypomagnesemia in critically ill cancer patients: a prospective study of predictive factors. Brazilian J Med Biol Res. 2000;33(12):1443–8.
Chen M, Sun R, Hu B. The influence of serum magnesium level on the prognosis of critically ill patients. Zhonghua Wei Zhong Bing Ji Jiu yi Xue. 2015;27(3):213–7.
Bhan I. Phosphate management in chronic kidney disease. Curr Opin Nephrol Hypertens. 2014;23(2):174–9.
Vervloet MG, van Ballegooijen AJ. Prevention and treatment of hyperphosphatemia in chronic kidney disease. Kidney Int. 2018;93(5):1060–72.
Vervloet MG, Sezer S, Massy ZA, Johansson L, Cozzolino M, Fouque D. The role of phosphate in kidney disease. Nat Rev Nephrol. 2017;13(1):27–38.
Reintam Blaser A, Gunst J, Ichai C, Casaer MP, Benstoem C, Besch G, et al. Hypophosphatemia in critically ill adults and children - A systematic review. Clin Nutr. 2021;40(4):1744–54.
Hendrix RJ, Hastings MC, Samarin M, Hudson JQ. Predictors of Hypophosphatemia and Outcomes during Continuous Renal Replacement Therapy. Blood Purif. 2020;49(6):700–7.
El Shazly AN, Soliman DR, Assar EH, Behiry EG, Gad Ahmed IAEN. Phosphate disturbance in critically ill children: Incidence, associated risk factors and clinical outcomes. Annals Med Surg. 2017;21:118–23.
Thongprayoon C, Cheungpasitporn W, Mao MA, Sakhuja A, Erickson SB. Admission hyperphosphatemia increases the risk of acute kidney injury in hospitalized patients. J Nephrol. 2018;31(2):241–7.
Kuo G, Lee C-C, Yang S-Y, Hsiao Y-C, Chuang S-S, Chang S-W, et al. Hyperphosphatemia is associated with high mortality in severe burns. PloS One. 2018;13(1):e0190978.
Johnson A, Bulgarelli L, Pollard T, Horng S, Celi LA, Mark R. MIMIC-IV (version 1.0). PhysioNet. 2021. https://doi.org/10.13026/s6n6-xd98.
Duprey MS, Van Den Boogaard M, Van Der Hoeven JG, Pickkers P, Briesacher BA, Saczynski JS, et al. Association between incident delirium and 28- and 90-day mortality in critically ill adults: a secondary analysis. Critical Care. 2020;24(1).
Ferrer M, Torres A. Epidemiology of ICU-acquired pneumonia. Current Opinion Crit Care. 2018;24(5):325–31.
Berndt T, Kumar R. Novel Mechanisms in the Regulation of Phosphorus Homeostasis. Physiology. 2009;24(1):17–25.
de Menezes FS, Leite HP, Fernandez J, Benzecry SG, de Carvalho WB. Hypophosphatemia in children hospitalized within an intensive care unit. J Intensive Care Med. 2006;21(4):235–9.
Miller CJ, Doepker BA, Springer AN, Exline MC, Phillips G, Murphy CV. Impact of Serum Phosphate in Mechanically Ventilated Patients With Severe Sepsis and Septic Shock. J Intensive Care Med. 2020;35(5):485–93.
Haider DG, Lindner G, Wolzt M, Ahmad SS, Sauter T, Leichtle AB, et al. Hyperphosphatemia Is an Independent Risk Factor for Mortality in Critically Ill Patients: Results from a Cross-Sectional Study. PloS One. 2015;10(8):e0133426.
Al Harbi SA, Al-Dorzi HM, Al Meshari AM, Tamim H, Abdukahil SAI, Sadat M, et al. Association between phosphate disturbances and mortality among critically ill patients with sepsis or septic shock. BMC. Pharmacol Toxicol. 2021;22(1).
Vincent JL, Moreno R, Takala J, Willatts S, De Mendonca A, Bruining H, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22(7):707–10.
Sundararajan V, Henderson T, Perry C, Muggivan A, Quan H, Ghali WA. New ICD-10 version of the Charlson comorbidity index predicted in-hospital mortality. J Clin Epidemiol. 2004;57(12):1288–94.
Acknowledgements
The present study data was based on the MIMIC-IV database. We would like to thank all staff and patients involved in the construction of the MIMIC-IV database.
Funding
This work was supported by the Project of Establishment of Early Warning and First-aid Screening System for Critically ill Patients in Hospitals Based on Artificial Intelligence (2020YFS0093) and the 1.3.5 project for disciplines of excellence, West China Hospital, Sichuan University (ZYJC18006).
Author information
Authors and Affiliations
Contributions
Jie Yang: study design, data extraction, data analyses, and manuscript writing. Yisong Cheng, data extraction and data analyses. Ruoran Wang: data extraction. Bo Wang: manuscript revising.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
MIMIC-IV database used in the present study was approved by the Institutional Review Boards (IRB) of the Massachusetts Institute of Technology, and consent was obtained for the original data collection. Therefore, the need for informed consent were waived for this manuscript.
Consent for publication
Not applicable.
Competing interests
All authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yang, J., Cheng, Y., Wang, R. et al. Association between early elevated phosphate and mortality among critically ill elderly patients: a retrospective cohort study. BMC Geriatr 22, 208 (2022). https://doi.org/10.1186/s12877-022-02920-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12877-022-02920-z