Abstract
Background
Diabetes is a serious and quickly expanding global health problem. Cardiovascular disease is the leading cause of mortality in type 2 diabetes mellitus (T2DM) patients. Coronary slow flow (CSF) is characterised by delayed distal perfusion during coronary angiography with normal coronary arteries.
This study aimed to investigate the correlation between CSF and inflammatory markers regarding glycemic status in T2DM.
Methods
This cross-sectional study included 120 patients who were divided equally into 4 groups according to their glycemic control and presence or absence of coronary slow flow: Group I included patients with T2DM with good glycemic control without CSF; Group II included patients with T2DM with good glycemic control and CSF; Group III included patients with T2DM with poor glycemic control without CSF; and Group IV included patients with T2DM with poor glycemic control and CSF. The neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), C-reactive protein (CRP), platelets, hematocrit, and haemoglobin were also evaluated as risk factors for coronary slow flow.
Results
This study showed that body mass index (BMI), hematocrit level, NLR, and CRP demonstrated a moderate but significant correlation (r = 0.53) with CSF in poorly controlled T2DM. NLR cutoff > 2.1 could predict CSF in poorly controlled T2DM with a modest sensitivity and specificity. A 1.9 increase in HbA1c increases the likelihood of coronary slow flow. Dylipidemia increases the likelihood of coronary slow flow by 0.18 times. Other predictors for coronary slow flow include NLR, PLR, CRP, platelets, hematocrit, and hemoglobin. The effect of the predictors is still statistically significant after being adjusted for glycemic status, age, and sex (p < 0.001).
Conclusions
Poor glycemic control increases the incidence of CSF. This supports the hypothesis that CSF is related to endothelial dysfunction as poor glycemic control causes endothelial dysfunction due to inflammation.
Trial registration
ZU-IRB#9419–3-4–2022 Registered 3 April 2022, email. IRB_123@medicine.zu.edu.eg.
Similar content being viewed by others
Introduction
In 2019, the International Diabetes Federation (IDF) predicted that Egypt ranks ninth among the world’s countries, with around 8,850,400 cases and a frequency of 15.2% in adults. Egypt is expected to be the seventh-largest country in the world by 2045 [1].
Coronary heart disease (CHD), heart failure, arrhythmias, and sudden cardiac death are examples of macrovascular complications. Cerebrovascular disease and peripheral artery disease are both types of cardiovascular disease in T2DM. Complications contribute significantly to morbidity and death in both types of diabetes. Cardiovascular disease is the leading cause of mortality in T2DM patients [2, 3].
Glycemic control is evaluated by haemoglobin A1c (HbA1c), continuous glucose monitoring (CGM) with either time in range (TIR) and/or glucose management indicator (GMI), and blood glucose monitoring (BGM) [4].
One of the major causes of atherosclerosis is diabetes. Inflammation has been clearly established to have a significant role in the initiation, development, and progression of atherosclerosis. CSF was a marker of endothelial activation and inflammation. HbA1c is also a significant inflammatory marker [5].
Inflammation has a role in many cardiovascular diseases, and inflammatory pathways have been recognised in the setting of CSF. Other inflammatory indicators, such as red cell distribution width and serum uric acid levels, have also been linked to the presence of CSF. Inflammatory parameter abnormalities may be a sign of endothelial dysfunction, both of which lead to CSF [6].
Therefore, the current study aimed to investigate the correlation between CSF and inflammatory markers regarding glycemic status in T2DM.
Materials and methods
We enrolled 120 diabetic patients of type 2 with chronic coronary syndrome (CCS) at our Cardiology Department, Faculty of Medicine, Zagazig University, Egypt.
Inclusion criteria
All T2DM patients who were referred for coronary angiography and had coronary slow flow were included in the study. The presence of typical chest discomfort or positive or conflicting results from noninvasive screening measures for myocardial ischemia served as the justification for coronary angiography. If non-invasive assessment indicates high risk occurrences, coronary angiography is recommended. The CSF is basically defined as a delay in the progression of the contrast that is injected into the coronary arteries during coronary angiography [6].
Exclusion criteria
Patients with valvular heart disease, atrial fibrillation, cardiomyopathies, congenital heart disease and hematological disorders were excluded.
Study population
This study included all patients with T2DM on conventional glycemic control (CGC); Admission blood glucose, 180–200 mg/dl) by conventional therapy using insulin and Dipeptidyl-peptidase 4 (DPP4) inhibitors who referred for coronary angiography who also had CSF. The patients were divided into four groups based on their glycemic control and the presence or absence of CSF. Group I: patients with T2DM with good glycemic control without CSF (n = 30); Group II: patients with T2DM with good glycemic control and CSF (n = 30); Group III: patients with T2DM with poor glycemic control without CSF (n = 30); Group IV: patients with T2DM with poor glycemic control and CSF (n = 30). NLR was measured in each group to see how it related to glycemic control parameters and predicted the occurrence of CSF. Other predictors of the occurrence of CSF were also investigated.
Clinical assessment
Complete history taking
Age, gender, and CAD risk factors such as hypertension, diabetes, smoking, dyslipidemia, and a family history of premature coronary artery disease (CAD) are all considered.
According to the ESH/ESC Guidelines for the Management of Arterial Hypertension, hypertension is defined as blood pressure levels of 140 mmHg SBP and/or 90 mmHg DBP [7].
Diabetes mellitus was diagnosed on basis listed by American Diabetes Association (2010) as: Fasting blood sugar ≥ 126 mg/dl or 2 h postprandial blood sugar ≥ 200 mg/dl or HBA1C ≥ 6.5 or Symptoms of diabetes plus casual plasma glucose concentration ≥ 200 mg/dl. Casual is defined as any time of day without regard to time since last meal. The classic symptoms of diabetes include polyuria, polydipsia, and unexplained weight loss [8].
Smoking was defined as active smoking in the last 6 months [9].
Dyslipidemia was considered according to recommendations of Third Report of the National Cholesterol Education Program (NCEP), when any of the following was present: serum cholesterol ≥ 200 mg/dl, LDL ≥ 100 mg/dl, HDL < 40 mg/dl for high-risk patients [10].
Family history of premature CAD, defined by the presence of at least a first degree relative with a cardiovascular event or premature SCD at a young age (< 65 years for women and < 55 years for men) [11].
General and local examination
Blood pressure, BMI, and electrocardiogram (ECG) were measured to all patients. Body Mass Index (BMI), defined as the body weight divided by the square of the body height in meters, and is universally expressed in units of kg/m2, resulting from mass in kilograms and height in meters [12].
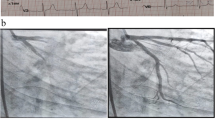
Invasive coronary angiography
The diagnostic criteria for CSF are based on the recommendations of Beltrame [13]. At coronary angiography, there was no coronary artery stenosis or stenosis 40%, and when the delay of distal angiographic contrast agent filling reaches a corrected TIMI frame count (cTFC) value greater than 27 frames (30 frames/s), at least one coronary artery is involved.
Transthoracic echocardiography (TTE)
All patients underwent TTE using the commercially available system (Vivid E9, General Electric, Horten, Norway, 2013) on admission for the coronary angiography procedure. Standard images were obtained using a 3.5–5 MHz transducer at a depth of 16 cm in the parasternal and apical views. The TTE study was performed according to the recommendations of the American Society of Echocardiography and European Association of Echocardiography, and measurements were indexed to body surface area when indicated. Assessment of resting regional wall motion abnormalities, wall motion score index (WMSI), ejection fraction and LV end-diastolic and end-systolic volumes were calculated using the biplane Simpson’s method and resting wall motion abnormalities (Fig. 1) [14].
Laboratory investigations
Blood samples of the patients were obtained in the morning between 8:00 a.m. and 10:00 a.m. after a fast of at least 8 h. The blood samples of all patients obtained for complete blood count (CBC), fasting plasma glucose, HbA1c, and hsCRP were studied. The NLR of the patients is calculated by dividing the absolute neutrophil number by the absolute lymphocyte number. The neutrophil-to-lymphocyte ratio (NLR), platelet-to-lymphocyte ratio (PLR), C-reactive protein (CRP), platelets, hematocrit, and haemoglobin were also evaluated as risk factors for coronary slow flow.
Statistical analysis
Version 26 of the Statistical Program for Social Science (SPSS) was used to analyse the data. Continuous data were represented as mean and SD, and categorical data were represented as event and percentage. One-way ANOVA, independent t-test, chi-square test, or exact Fisher test, and Pearson correlation were used. ROC curve analysis and the Kappa test were used to detect the ideal cut-off values of the predictors with the greatest sensitivity and specificity. When the probability of error is less than 5% (p < 0.05), the result is significant.
Results
This study revealed that there was no statistically significant difference between groups in terms of age, gender, or CAD family history.
This investigation revealed that there was no statistically significant difference in haemoglobin levels across groups.
Hematocrit, platelet lymphocyte ratio (PLR), and c-reactive protein (CRP) were significantly lower in patients without CSF (Group I, Group III) compared to those with CSF (Group II, Group IV) (p3, p5, p6 < 0.05) (Table 1).
CSF correlates positively with NLR in patients with inadequate glucose management (Table 2).
The current study looked at the relationship between coronary slow flow and NLR in relation to glycemic status. Coronary slow flow shows a moderately significant correlation with NLR (r = 0.548) (Table 3). When compared to non-hypertensive patients, the presence of hypertension increases the likelihood of coronary slow flow by 4.66 times. Smoking causes 3.5 times as many cases of coronary slow flow as nonsmokers. Dyslipidemia increases the likelihood of coronary slow flow by 0.18 times. Other predictors for coronary slow flow include NLR, PLR, CRP, platelets, hematocrit, and hemoglobin. The effect of the predictors was still statistically significant after being adjusted for glycemic status, age, and sex (p < 0.0001) (Table 3; Figs. 2, 3 and 4).
Discussion
Inflammation plays a role as an important pathogenic factor for various cardiovascular diseases, along with coronary heart disease. So, the neutrophil-to-lymphocyte ratio (NLR) has been reported to affect various inflammatory diseases, including some cardiovascular diseases. NLR is also an important factor in cardiovascular diseases in terms of morbidity and mortality [6].
In patients with T2DM and CSF, our study showed that NLR had a moderately significant correlation with glycemic control parameters. The study performed by Sefil et al. [15] reported results that were similar to those found in this study. Hussain et al. [16] reported similar results between NLR and glycemic regulation. They found a significant association between NLR and HbA1c among the groups divided into three according to their glycemic control status. In this study, NLR values after treatment were not investigated. Which explained by presence of DM can induce inflammation and release of inflammatory markers which induce endothelial dysfunction.
In a prospective study on a non-diabetic 38,074-strong cohort, an average of 6-year follow-up NLR was associated with the incidence and prevalence of T2DM. This finding suggests that the NLR is a predictor of diabetes development [17].
Our study found no significant relationship between NLR and glycemic control parameters in patients with T2DM who did not have CSF. This agreement with Mendes et al. [18] showed that hyperglycemic subjects had a NLR similar to that of normoglycemic subjects but had a lower PLR.
Our study showed that NLR was higher in patients with CSF than in patients without CSF, especially in patients with poor glycemic control; this agrees with Cetin et al. [19]; Oylumlu et al. [20]; and Challa et al. [21]. This may explain the role of inflammation in the pathogenesis of CSF.
Despite the studies mentioned above, the association between CSF and inflammation remains unclear due to the limited number of patients in these studies and conflicting data. In a study established by Altun et al. [22], they found no significant difference between patients with CSF and patients without CSF regarding NLR.
Our study showed that poor glycemic control increases the incidence of CSF. A one-degree increase in FBS increases the likelihood of CSF by 2.4. The increase in HbA1c increases the incidence of CSF by 1.9. This can ensure the hypothesis that coronary slow flow is caused by endothelial dysfunction, as chronic hyperglycemia is well known to accelerate the development of endothelial dysfunction and the pathological process of atherosclerosis, resulting in more diffuse coronary artery lesions and worse clinical outcomes [23].
Study limitations
The current study was restricted by its modest sample size (n = 120), as it was a single-center investigation. Patients with type 2 diabetes were the only ones included. All diabetic individuals should be included in future trials. Our research did not include those on chronic medication. It's possible that the long-term use of medicine contributes to the onset of coronary sluggish flow. Therefore, additional long-term studies are suggested to examine the connection between medications and CSF occurrence, preferably including the medication of patients.
Clinical implication
Patients are more likely to develop coronary sluggish flow if they have risk factors such as (hypertension, smoking, increased BMI, dyslipidemia, high platelet count, high hematocrit value, high NLR, high PLR, and high CRP level).
Conclusion
Poor glycemic control increases the incidence of CSF. This support the hypothesis that CSF is related to endothelial dysfunction as poor glycemic control cause endothelial dysfunction.
Other factors (hypertension, smoking, increased BMI, decreased dyslipidemia and high platelet count, hematocrit, PLR and CRP) significantly increase in patients with CSF and can be used as predictors of CSF.
Recommendations
Further large caliber, multicenter studies are needed to consolidate our findings. Further long-term studies which include patient medication are recommended to evaluate the relation between drugs and CSF occurrence. NLR may be useful as an easily measurable, non-invasive and cost-effective parameter for follow up of glycemic control in patients with CSF and also for prediction of CSF. Good glycemic control is mandatory as poor glycemic control leads to various cardiovascular events.
Availability of data and materials
Our data used to support the findings of this study are available from the corresponding author upon request.
Abbreviations
- BMI:
-
Body mass index
- CSF:
-
Coronary slow flow
- T2DM:
-
Type 2 diabetes mellitus
- CRP:
-
C-reactive protien
- NLR:
-
Neutrophil-to-lymphocyte ratio
- PLR:
-
Platelet-to-lymphocyte ratio
- WMSI:
-
Wall motion score index
- CHD:
-
Coronary heart disease
- IDF:
-
International Diabetes Federation
- HbA1c:
-
Hemoglobin A1c
- FBS:
-
Fasting blood sugar
- CGM:
-
Continuous glucose monitoring
- TIR:
-
Time in range
- GMI:
-
Glucose management indicator
- BGM:
-
Blood glucose monitoring
- CGC:
-
Conventional glycemic control
- DPP4:
-
Dipeptidyl-peptidase 4
- CAD:
-
Coronary artery disease
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- LDL:
-
Low density lipoprotin
- HDL:
-
High density lipoprotin
- SCD:
-
Sudden cardiac death
- ECG:
-
Electrocardiogram
- BMI:
-
Body mass index
- NCEP:
-
National cholesterol education program
- CBC:
-
Complete blood picture
References
Azzam MM, Ibrahim AA, El-Ghany A, Mohammed I. Factors affecting glycemic control among Egyptian people with diabetes attending primary health care facilities in Mansoura District. Egypt J Intern Med. 2021;33(1):1–10.
Viigimaa M, Sachinidis A, Toumpourleka M, Koutsampasopoulos K, Alliksoo S, Titma T. Macrovascular complications of type 2 diabetes mellitus. Curr Vasc Pharmacol. 2020;18(2):110–6.
Joseph JJ, Deedwania P, Acharya T, Aguilar D, Bhatt DL, Chyun DA. Comprehensive management of cardiovascular risk factors for adults with type 2 diabetes: a scientific statement From the American Heart Association. Circulation. 2022;145(9):e722–59.
Assessment G. Glycemic targets: standards of medical care in diabetes. Diabetes Care. 2021;44:S73–84.
Yilmaz H, Demir I, Uyar Z. Clinical and coronary angiographic characteristics of patients with coronary slow flow. Acta Cardiol. 2008;63(5):579–84.
Wang X, Nie SP. The coronary slow flow phenomenon: characteristics, mechanisms and implications. Cardiovasc Diagn Ther. 2011;1(1):37.
Williams B, Mancia G, Spiering W, AgabitiRosei E, Azizi M, Burnier M, Clement DL, Coca A, De Simone G, Dominiczak A, Kahan T. 2018 ESC/ESH Guidelines for the management of arterial hypertension: the Task Force for the management of arterial hypertension of the European Society of Cardiology (ESC) and the European Society of Hypertension (ESH). Eur Heart J. 2018;39(33):3021–104. https://doi.org/10.1093/eurheartj/ehy339.
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–9. https://doi.org/10.2337/dc10-S062.
Yang HP, Brinton LA, Platz EA, Lissowska J, Lacey JV Jr, Sherman ME, Garcia-Closas M. Active and passive cigarette smoking and the risk of endometrial cancer in Poland. Eur J Cancer. 2010;46(4):690–6.
Burke AC, Dron JS, Hegele RA, Huff MW. PCSK9: regulation and target for drug development for dyslipidemia. Annu Rev Pharmacol Toxicol. 2017;57:223-44.0.
Abdi-Ali A, Shaheen A, Southern D, Zhang M, Knudtson M, White J, Graham M, James MT, Wilton SB. Relation between family history of premature coronary artery disease and the risk of death in patients with coronary artery disease. Am J Cardiol. 2016;117(3):353–8.
Nuttall FQ. Body mass index: obesity, BMI, and health: a critical review. Nutr Today. 2015;50(3):117. https://doi.org/10.1097/NT.0000000000000092.
Beltrame JF. Defining the coronary slow flow phenomenon. Circ J. 2012;76(4):818–22.
Lang RM, Badano LP, Mor-Avi V, Afilalo J, Armstrong A, Ernande L, Voigt JU. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015;16(3):233–71.
Sefil F, Ulutas KT, Dokuyucu R, Sumbul AT, Yengil E, Yagiz AE, Gokce C. Investigation of neutrophil lymphocyte ratio and blood glucose regulation in patients with type 2 diabetes mellitus. J Int Med Res. 2014;42(2):581–8.
Hussain M, Babar MZM, Akhtar L, Hussain MS. Neutrophil lymphocyte ratio (NLR): a well assessment tool of glycemic control in type 2 diabetic patients. Pakistan J Med Sci. 2017;33(6):1366.
Guo X, Zhang S, Zhang Q, Liu L, Wu H, Du H, Niu K. Neutrophil: lymphocyte ratio is positively related to type 2 diabetes in a large-scale adult population: a Tianjin chronic low-grade systemic inflammation and health cohort study. Eur J Endocrinol. 2015;173(2):217–25.
Mendes BB, Oliveira ACR, Alcântara KCD. Comparison of the neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in normoglycemic and hyperglycemic subjects. Einstein (Sao Paulo). 2019;17:4403.
Çetin M, Kiziltunc E, Elalmış ÖU, Çetin ZG, Demirçelik MB, Çiçekçioğlu H, Ulusoy FV. Predictive value of neutrophil lymphocyte ratio and platelet lymphocyte ratio in patients with coronary slow flow. Acta Cardiol Sin. 2016;32(3):307.
Oylumlu M, Doğan A, Oylumlu M, Yıldız A, Yüksel M, Kayan F, Amasyalı B. Relationship between platelet-to-lymphocyte ratio and coronary slow flow. Anatol J Cardiol. 2015;15(5):391.
Reddy Challa KK, Jyotsna M. CRT-100.15 angiographic profile and laboratory predictors of coronary slow flow phenomenon in South Indian population. Cardiovasc Interv. 2022;15(4):S4–S4.
Altun I, Akin F, Kose N, Sahin C, Kirli I. Predictors of slow flow in angiographically normal coronary arteries. Int J Clin Exp Med. 2015;8(8):13762.
Xu J, Zou MH. Molecular insights and therapeutic targets for diabetic endothelial dysfunction. Circulation. 2009;120(13):1266–86.
Acknowledgements
Not applicable.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). The study was performed at our University Hospitals with no funding sources.
Author information
Authors and Affiliations
Contributions
M.E. wrote the manuscript and did statistical analysis. I.T. collected data and acquisition analysis and was the major contributor in writing the manuscript. G.M. did the statistical analysis, drafted and revised the article. S.Z. collected tables and figures and revised the article. I.S. interpreted the data and critical revision of article. All authors reviewed the manuscript. The author(s) read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The Zagazig University Institutional Review Board (ZU-IRB # 9419–3-4–2022) approved the study, confirming that all methods were carried out in accordance with The Code of Ethics of the World Medical Association (Declaration of Helsinki) for experiments involving humans and informed and written consent was taken from all participants in our research.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Elsanan, M.A.H.A., Tahoon, I.H.H.H., Mohamed, G.I. et al. Relationship between inflammatory markers and coronary slow flow in type 2 diabetic patients. BMC Cardiovasc Disord 23, 244 (2023). https://doi.org/10.1186/s12872-023-03275-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-023-03275-y