Abstract
Background
N-terminal pro B-type peptide (NT-proBNP) has been associated with risk of myocardial infarction (MI), but less is known about the relationship between NT-proBNP and very small non ST-elevation MI, also known as microsize MI. These events are now routinely detectable with modern troponin assays and are emerging as a large proportion of all MI. Here, we sought to compare the association of NT-proBNP with risk of incident typical MI and microsize MI in the REasons for Geographic and Racial Differences in Stroke (REGARDS) Study.
Methods
The REGARDS Study is a national cohort of 30,239 US community-dwelling black and white adults aged ≥ 45 years recruited from 2003 to 2007. Expert-adjudicated outcomes included incident typical MI (definite/probable MI with peak troponin ≥ 0.5 μg/L), incident microsize MI (definite/probable MI with peak troponin < 0.5 μg/L), and incident fatal CHD. Using a case-cohort design, we estimated the hazard ratio of the outcomes as a function of baseline NT-proBNP. Competing risk analyses tested whether the associations of NT-proBNP differed between the risk of incident microsize MI and incident typical MI as well as if the association of NT-proBNP differed between incident non-fatal microsize MI and incident non-fatal typical MI, while accounting for incident fatal coronary heart disease (CHD) as well as heart failure (HF).
Results
Over a median of 5 years of follow-up, there were 315 typical MI, 139 microsize MI, and 195 incident fatal CHD. NT-proBNP was independently and strongly associated with all CHD endpoints, with significantly greater risk observed for incident microsize MI, even after removing individuals with suspected HF prior to or coincident with their incident CHD event.
Conclusion
NT-proBNP is associated with all MIs, but is a more powerful risk factor for microsize than typical MI.
Similar content being viewed by others
Background
B-type natriuretic peptide (BNP) and its N-terminal fragment (NT-proBNP) are cardiac-derived secretory hormones with diuretic, vasodilatory, and natriuretic properties [1]. Although it is commonly used in assessing patients with heart failure (HF), NT-proBNP is independently associated with risk of coronary heart disease (CHD) as well as adverse outcomes among patients with ST-elevation myocardial infarction (STEMI). [2,3,4,5] Recently, the prognostic implications of NT-proBNP have been extended to patients with non–ST-elevation MI (NSTEMI) and those with stable CHD presenting with chest pain [6, 7].
While NT-proBNP is associated with MI in general, less is known about the relationship between NT-proBNP and the emerging disorder of very small NSTEMI, or microsize MI. Microsize MI has modest peak troponin elevations that in the past were considered to have uncertain clinical relevance [8]. Because of the wide implementation of sensitive troponin assays, microsize MIs are now increasingly recognized and have been shown to be associated with elevated long term CHD risk [8, 9]. A better understanding of the similarities and differences in risk factors between microsize and typical MIs is needed to guide risk stratification and optimize clinical management [10,11,12,13].
Prior to the widespread use of highly sensitive troponin assays, studies demonstrated an association of NT-proBNP with the incidence of typical MIs, but were limited in the ability to differentiate typical from microsize MIs. Therefore, we hypothesized that there would be an association between baseline levels of NT-proBNP and risk of incident microsize MIs. We conducted this study in the national Reasons for Geographic and Racial Differences in Stroke (REGARDS) cohort study.
Methods
REGARDS cohort study procedures
Details of the REGARDS study have been described previously [14]. Briefly, REGARDS is a prospective cohort study evaluating racial and geographic disparities in stroke and MI. 30,239 English-speaking, community dwelling U.S. adults ≥ 45 years of age were recruited between January 2003 and October 2007 by mail and telephone. Blacks and residents of the stroke belt were oversampled [14]. Participants completed a telephone interview ascertaining medical history followed by an in-home examination assessing blood pressure levels, height and weight, ECGs, anthropomorphic measures, and blood and urine samples along with a medication inventory. Blood and urine samples were processed at the REGARDS Central Laboratory at the University of Vermont. Phlebotomy was performed by trained personnel after a 10–12 h fast, using standardized procedures. Within 2 h of collection, samples were centrifuged and shipped on ice to the University of Vermont, where, upon arrival, samples were centrifuged at 30,000 × G and 4 °C, and either analyzed (general chemistries) or stored at − 80 °C [15, 16].
At six month intervals, participants are contacted by phone to ask about hospitalizations and general health status, with medical record retrieval for suspected coronary events. The study protocol was reviewed and approved by the University of Alabama at Birmingham Institutional review board and all participants provided written informed consent.
Primary outcome(s)
For CHD events, medical records were adjudicated by expert clinicians based on published guidelines [17, 18] considering clinical signs and symptoms consistent with ischemia; a rising and/or falling pattern of troponin over ≥ 6 h with a peak at least twice the upper limit of normal; and/or ECG or other imaging findings consistent with ischemia based on the Minnesota code [19]. Cases where the clinical presentation was equivocal or where the troponin rise was less than twice the upper limit of normal were adjudicated to be possible MIs and were not included as outcomes in this analysis. Cases with low-level troponin elevations without a rising and/or falling pattern over ≥ 6 h or with a non-ischemic cause of troponin elevation were not considered to be MIs. Elective and urgent coronary revascularization procedures were not included in the definition of MI and we classified MIs caused by an invasive procedure as procedure related. Only definite or probable MIs were considered as MIs. Definite MIs included cases with diagnostic enzymes or electrocardiogram and probable MIs included cases with elevated but not diagnostic (ie, equivocal) enzymes with a positive but not diagnostic electrocardiogram or, if enzymes were missing, a positive electrocardiogram in the presence of ischemic signs or symptoms.
As other REGARDS studies have done, 0.5 μg/L was used as the threshold of peak troponin to define microsize MI [20, 18]. This definition of microsize MI (peak troponin < 0.5 μg/L) has been previously used by Safford et al. (2013) and is based on clinical practice as well as an analyses of troponin assay 99th percentiles and 10% CV levels available on the International Federation of Clinical Chemists website [21]. All other adjudicated definite or probable MIs were considered to be typical MIs (peak troponin ≥ 0.5 μg/L) [20, 21].
Since death at the first presentation with CHD remains common, an additional endpoint included total incident fatal CHD (deaths caused by CHD including sudden deaths and death within 28 days of an adjudicated MI). Interviews with next of kin, the National Death Index, [14] death certificates, medical records, and autopsy reports were used to adjudicate cause of death.
NT-proBNP
Baseline NT-Pro BNP was measured using the Roche Elecsys analyzer (Roche Diagnostics Indianapolis, IN) which utilizes an electrochemiluminescence immunoassay (inter-assay coefficient of variation < 5%) [22].
Covariates
Demographic data included self-reported age, sex, race (black or white), education (less than high school and high school or higher), annual income (less than $20,000 and $20,000 and above). Region of residence was classified as being a resident of the stroke buckle (the coastal regions of North and South Carolina and Georgia), the stroke belt (the remainder of North and South Carolina and Georgia, plus Alabama, Mississippi, Louisiana, Arkansas, and Tennessee), or not a stroke belt resident (the remaining 40 contiguous United States). Clinical CHD risk factors included diabetes, defined as fasting blood glucose ≥126 mL/dL (or glucose > 200 mL/dL for those failing to fast) or oral hypoglycemic or insulin use; systolic blood pressures based on the average of 2 standardized blood pressure measurements (continuous variables in mm Hg); body mass index (BMI) based on measured height and weight; cigarette smoking (current smoking versus never or former smokers); albumin-to-creatinine ratio (ACR), which was log transformed for the analysis; high sensitivity c-reactive protein (hsCRP), which was also log transformed; and high-density lipoprotein (HDL) and total cholesterol. Estimated glomerular filtration rate (eGFR) was calculated using the Chronic Kidney Disease (CKD) Epidemiology Collaboration formula, [23] with CKD defined as eGFR as < 60 ml/min/1.73 [2]. Medication use included aspirin (yes or no), statins (yes or no), and antihypertensive medications (yes or no).
Case-cohort design
The case-cohort study design minimizes the cost of expensive biomarker assays without compromising the power advantage of large cohort studies [24, 25]. Here, the study was comprised of all incident acute CHD cases through 12/31/2010 and a stratified random sample of participants free of CHD at baseline and not on dialysis (the sub-cohort). The sub-cohort random sample was selected as previously described using stratified random sampling in 20 age (45–54, 55–64, 65–74, 75–84, ≥ 85 years), race (black and white), and sex strata [26].
Statistical analysis
Participant characteristics were compared across tertiles of NT-proBNP within the cohort random sample using appropriate sampling weights. Analysis of variance and Χ2 tests were used to evaluate significant differences.
Using Cox regression for case-cohort studies, [25] with Barlow and Prentice sampling weights, [27] we performed competing risk analyses as described by Lunn and McNeil [28] incorporating the sub-cohort sampling weights to test whether the association between NT-proBNP and the risk of incident microsize MI differed from 1) that of typical MI and 2) while also accounting for incident fatal CHD death. Hazard ratios (HR) and 95% confidence intervals (CI) were calculated for the outcomes defined above as a function of NT-proBNP in crude models and models adjusted for demographics (age, race, sex, income, education, geographic region of residence), Framingham risk factors (smoking, systolic blood pressure, diabetes, HDL, total cholesterol), and additional CVD risk factors (BMI, hsCRP, ACR, eGFR, medications). NT-proBNP was analyzed in tertiles with the lowest tertile serving as the reference group. In the analysis accounting for incident fatal CHD death, MI events followed by death within 28 days were classified as CHD death, effectively comparing the association between NT-proBNP and three separate outcomes: nonfatal typical MI, nonfatal microsize MI, and fatal CHD.
Because elevated BNP may be associated with HF, we repeated all analyses excluding individuals with NT-proBNP levels above the age-specific normal range (> 125 pg/mL if < 75 years old and > 450 pg/mL if ≥75 years old), with an adjudicated HF hospitalization prior to their MI event or CHD death, or who had HF during the incident MI hospitalization.
In all analyses, a 2-tailed P value < 0.05 was considered statistically significant. Additionally, 10% of individuals had at least one missing value for covariates, thus final analyses were conducted with multiple imputation using chained equations [29]. Covariates with the largest amount of missing values were ACR (4%) and hsCRP (2%). Analyses were conducted using SAS software version 9.4 (SAS Institute, Cary, NC) and Stata 14 (Stata Corp, College Station, TX).
Results
Baseline characteristics of the study participants
Of the 30,239 REGARDS participants, we excluded 569 who were missing follow up, leaving 29,670 from which 1104 were drawn for the random sub-cohort. Of these, 50 were excluded for missing NT-proBNP, 23 for laboratory inconsistencies, 182 for a history of CHD at baseline, and 2 on dialysis. A final analytic sub-cohort of 847 was used for this analysis (Additional file 1: Fig. S1). Over a median of 5.0 (IQR: 3.5, 6.3) years of follow-up time, there were 454 incident MI cases, of which 315 were typical MIs and 139 were microsize MIs. The median time to event for microsize MI was 2.7 (IQR: 1.3, 5.5) and the median time to event for typical MI was 2.2 (1.1, 3.7). There were also 195 incident fatal CHD cases. Twenty-one of the participants who experienced incident MI or fatal CHD were in the randomly selected sub-cohort.
Baseline characteristics of sub-cohort random sample participants by tertile of NT-proBNP are shown in Table 1. Higher NT-proBNP was characterized by female sex, white race, older age, lower educational attainment, lower annual income, higher risk factor levels, and a greater burden of medical illness.
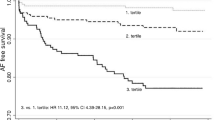
Associations of NT-proBNP with microsize and typical MIs
The cause-specific hazard ratios (CHR) for microsize and typical MIs by tertile of NT-proBNP are shown in Table 2. A significant difference in the association between NT-proBNP and the risk of microsize versus typical MI was seen in unadjusted and adjusted models (p for equality = 0.03). In the unadjusted model, participants in the highest tertile of baseline NT-proBNP compared to the lowest had higher risk of incident microsize MI (CHR 7.06, CI: 3.96–12.57) compared to incident typical MI (CHR 2.86, CI: 2.01–4.05). These results were similar with full adjustment (NT-proBNP and microsize MI adjusted CHR [aCHR] 6.83 (CI: 3.52–13.25) and typical MI aCHR 2.63 (CI: 1.63–4.33) with a p for equality of 0.03 (Table 2).
In the sensitivity analysis of the competing risk between microsize and typical MI among participants without possible HF, a total of 71 participants with microsize MIs and 133 participants with typical MIs were excluded. A significant difference in the risk of incident microsize versus typical MI by NT-proBNP tertiles persisted (p for equality = 0.05), with the association between NT-proBNP and microsize MI remaining larger across unadjusted and adjusted models, albeit of borderline statistical significance (p for equality = 0.06) (Table 3).
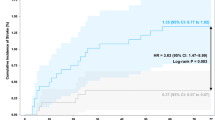
When accounting for acute fatal CHD as a competing risk, a significant difference in the association between NT-proBNP and risk of incident non-fatal microsize MI versus non-fatal typical MI was detected in unadjusted (p for equality < 0.01) and adjusted models (p for equality = 0.03) (Additional file 1: Table S1). In the unadjusted analysis, participants in the highest tertile of baseline NT-proBNP compared to the lowest tertile had higher risk of incident non-fatal microsize MI (CHR 6.69, CI: 3.69–12.12) than typical MI (CHR 2.57, CI: 1.80–3.67) and incident fatal CHD (CHR 5.15, CI: 3.31–8.01). These results were similar with full adjustment (NT-proBNP and incident non-fatal microsize MI aCHR 6.07, CI: 3.12–11.77; typical MI aCHR 2.25, CI: 1.41–3.60; and incident fatal CHD (aCHR 4.76, CI: 2.79–8.10).
In the sensitivity analysis accounting for fatal CHD among those without possible HF, there were substantially fewer events (Additional file 1: Table S2). Similar to the main results, the unadjusted HR for non-fatal microsize MI (HR 4.69 (95% CI 2.06–10.70) was higher than for typical MI (HR 2.20 [95% CI 1.35–3.59]), but this difference was not statistically significant. These patterns were maintained after full adjustment, and were also not statistically significant.
Discussion
In this prospective study of black and white US adults, similar to past studies, NT-proBNP was strongly associated with MI, but we observed an even stronger association between NT-proBNP and microsize MI than typical MI. The greater association between NT-proBNP and risk of microsize MI compared with typical MI persisted across multivariable models, in analyses excluding patients with potential HF, and analyses incorporating incident fatal CHD. To our knowledge, this is the first examination of the relationship of NT-proBNP with microsize MI, an entity only recently recognized as a large component of MIs in the modern era.
Increasingly sensitive troponin assays now routinely detect very small, or microsize, MIs, [30,31,32,33] which comprised 31.3% of non-fatal MI events in REGARDS and have been found to be associated with long-term CHD risk, apart from typical MIs [8]. Yet, due to variation across US laboratories, these very small events may often be missed or misclassified [21]. Work by Mills et al. (2011) suggests that misclassification may have serious clinical consequences: among patients presenting with suspected acute coronary syndrome (ACS), lowering the diagnostic threshold for MI from the previous generation troponin assay cutoff (0.20 ng/mL) to 0.05 ng/mL was associated with increased detection of MIs by 29%, increased evidence-based treatment in the group with peak troponin 0.05–0.20 ng/mL, and 50% reduction in death or recurrent MI among those with these small events [12]. The percent rise in events in the Mills study (29%) is remarkably similar to the proportion of microsize MIs in the REGARDS study (31%). These two studies, and others, [34, 35] demonstrate that failing to recognize and potentially treat microsize MI events could have profound implications for patient morbidity and mortality.
To date, the clinical characteristics of individuals who present with microsize MIs are not well described. We found that baseline levels of NT-proBNP were more strongly associated with risk of incident microsize MIs compared to typical MIs, which suggests that microsize MIs and typical MIs may differ with respect to their risk factor profiles and possibly their underlying pathophysiology. It is well known that myocardial stretch stimulates the release of NT-proBNP; NT-proBNP levels are also closely associated with vascular remodeling, inflammation, and hypertrophy in the cardiovascular system [33, 36]. Local hypoxemia and ischemia, independent of changes in left ventricular function, have been shown to induce NT-proBNP synthesis [37,38,39] and following tissue injury, inflammatory cytokines [40, 41] and cardiac myocytes induce BNP secretion as fibrosis [41] and vascular remodeling occurs [42]. Given the extent to which we found NT-proBNP to be associated with microsize MIs, it is plausible that these small events occur in the context of microvascular derangements of circulating factors in a way that differs from the medium vessel atherosclerotic plaque rupture that characterizes typical MIs. Recent studies further support this hypothesis by demonstrating that NT-proBNP levels are associated with small vessel disease [43, 44]. Mutlu et al. (2016) reported that in participants without cardiovascular disease, higher levels of NT-proBNP were associated with microvascular damage in the retina and retinal arterioles [45]. Additionally, Bower et al. (2015) found that higher levels of NT-proBNP were associated with incident hypertension, [46] a process that involves arteriolar narrowing, increased cardiac output, hypoxemia at the level of myocytes, and ultimately release of NT-proBNP. Finally, in a prospective study, Cushman et al. (2016), found that higher NT-pro-BNP levels were associated with incident cognitive impairment, independent of CVD and Alzheimer’s disease risk factors [16]. Together, these studies suggest that high levels of NT-proBNP may occur alongside, or in response to, systemic microvascular dysfunction in addition to, or apart from, its known association with large vessel disease.
Our findings also have important implications for the utility of NT-proBNP as a biomarker of CHD. A recent individual-participant-data meta-analysis found that among those without known baseline CVD, NT-proBNP concentration predicted first-onset HF and improved the prediction of CHD and stroke. [47] Additionally, the Dallas Heart Study demonstrated an independent association between coronary atherosclerosis burden and circulating levels of NT-proBNP [48] in a large, low-risk population without symptomatic HF or ischemia. NT-proBNP levels are independently predictive of atherosclerotic events [49, 50]; Goyal et al. (2014) found that BNP levels are related to the severity of coronary atherosclerosis such that patients with multi-vessel disease had higher BNP levels than those with one or two vessel involvement. Notably, this finding was independent of a diagnosis of unstable angina or NSTEMI. Collectively, these findings, in addition to our finding that NT-proBNP was strongly associated with both non-fatal microsize MI and fatal CHD, suggest that NT-proBNP might be used for risk stratification. However, it is important to note that major clinical trials in CHD have focused almost exclusively on typical MIs. As such, additional work is needed to identify the optimal clinical management strategies for patients surviving a microsize MI event.
Strengths and limitations
This study’s strengths include the large, geographically and racially diverse cohort in which participants were followed prospectively. Baseline data were collected in standardized fashion and prospective data included CHD endpoints adjudicated by expert clinicians. This study is unique in that we were able to study microsize MI events, which have not been specifically reported in other cohort studies and may be difficult to capture in claims data. Finally, competing risk analyses permitted examination of the association between NT-proBNP and incident microsize MIs versus typical MIs while accounting for acute fatal CHD.
Some limitations should be considered when interpreting these findings. Only a single baseline measure of NT-proBNP was available, with varying elapsed time between baseline and the events of interest. Only black and white adults were included, potentially limiting generalizability to other races or ethnicities. We were unable to measure left ventricular ejection fraction (LVEF) among cases or controls in this study; since ischemic and dilated cardiomyopathies are often associated with elevated troponin and NT-proBNP levels, future studies on the association between NT-proBNP and microsize MIs ought to include this as a covariate in multivariable models. Our sensitivity analysis excluding those with possible HF to some extent overcomes this limitation. Finally, several variables were self-reported with known vulnerability to bias.
Conclusion
This is the first study to examine the association of NT-proBNP with risk of microsize MI. Although baseline NT-proBNP levels were associated with microsize MIs, typical MIs, and fatal CHD, the association between NT-proBNP and risk of incident microsize MI was markedly higher than typical MI. This association persisted with adjustment for demographic and clinical covariates, excluding participants with possible HF, and accounting for fatal CHD. These results highlight the utility of NT-proBNP as a marker of CHD events, particularly the entity of microsize MIs. Our findings are concordant with past studies that suggest that these very small events represent a large proportion of MI events, but our findings build on these observations to suggest that they may differ from typical MIs, particularly with respect to risk factors and pathophysiology. Further study is needed to understand the relative contribution of traditional and non-traditional risk factors to the incidence of microsize MIs compared to typical MIs, as well as to understand differences in outcomes. If there are sufficient differences, it is possible that separate risk stratification tools may be needed, and NT-proBNP may be a candidate for inclusion in such tools. Our findings underscore that a better understanding is needed of this very large proportion of MIs in the modern era.
References
Levin E, Gardner DG, Samson WK. Natriuretic peptides. N Engl J Med. 1998;339(5):321–8.
de Lemos JA, Morrow DA, Bentley JH, et al. The prognostic value of B-type natriuretic peptide in patients with acute coronary syndromes. N Engl J Med. 2001;345(14):1014–21.
Bibbins-Domingo K, Gupta R, Na B, Wu AH, Schiller NB, Whooley MA. N-terminal fragment of the prohormone brain-type natriuretic peptide (NT-proBNP), cardiovascular events, and mortality in patients with stable coronary heart disease. JAMA. 2007;297(2):169–76.
Kragelund C, Gronning B, Kober L, Hildebrandt P, Steffensen R. N-terminal pro-B-type natriuretic peptide and long-term mortality in stable coronary heart disease. N Engl J Med. 2005;352(7):666–75.
Di Angelantonio E, Chowdhury R, Sarwar N, et al. B-type natriuretic peptides and cardiovascular risk: systematic review and meta-analysis of 40 prospective studies. Circulation. 2009;120(22):2177–87.
Heeschen C, Hamm CW, Mitrovic V, Lantelme NH, White HD. N-terminal pro-B-type natriuretic peptide levels for dynamic risk stratification of patients with acute coronary syndromes. Circulation. 2004;110(20):3206–12.
Jernberg T, Stridsberg M, Venge P, Lindahl B. N-terminal pro brain natriuretic peptide on admission for early risk stratification of patients with chest pain and no ST-segment elevation. J Am Coll Cardiol. 2002;40(3):437–45.
Safford MM, Brown TM, Muntner PM, et al. Association of race and sex with risk of incident acute coronary heart disease events. JAMA. 2012;308(17):1768–74.
Bhatt H, Safford M, Glasser S. Coronary heart disease risk factors and outcomes in the twenty-first century: findings from the REasons for geographic and racial differences in stroke (REGARDS) study. Curr Hypertens Rep. 2015;17(29):1–20.
Mills NLLK, McAllister DA, et al. Implications of lowering threshold of plasma troponin concentration in diagnosis of myocardial infarction: cohort study. The BMJ. 2012;344:e1533. The BMJ. 2012;e1533:344.
Morrow DA. Evidence-based decision limits for cardiac troponin: low-level elevation and prognosis. Am Heart J. Vol 148. United States2004:739–742.
Mills NL, Churchhouse AM, Lee KK, et al. Implementation of a sensitive troponin I assay and risk of recurrent myocardial infarction and death in patients with suspected acute coronary syndrome. JAMA. 2011;305(12):1210–6.
Morrow DA, Cannon CP, Rifai N, et al. Ability of minor elevations of troponins I and T to predict benefit from an early invasive strategy in patients with unstable angina and non-ST elevation myocardial infarction: results from a randomized trial. JAMA. 2001;286(19):2405–12.
Howard VJ, Cushman M, Pulley L, et al. The reasons for geographic and racial differences in stroke study: objectives and design. Neuroepidemiology. 2005;25(3):135–43.
Cushman M, McClure LA, Howard VJ, Jenny NS, Lakoski SG, Howard G. Implications of increased C-reactive protein for cardiovascular risk stratification in black and white men and women in the US. Clin Chem. 2009;55(9):1627–36.
Cushman M, Callas PW, McClure LA, et al. N-terminal pro-B-type natriuretic peptide and risk of future cognitive impairment in the REGARDS cohort. Journal of Alzheimer's disease : JAD. 2016;
Zhang ZM, Prineas RJ, Eaton CB. Evaluation and comparison of the Minnesota Code and Novacode for electrocardiographic Q-ST wave abnormalities for the independent prediction of incident coronary heart disease and total mortality (from the Women's Health Initiative). The American journal of cardiology. 2010;106(1):18–25.e12.
Luepker RV, Apple FS, Christenson RH, et al. Case definitions for acute coronary heart disease in epidemiology and clinical research studies: a statement from the AHA Council on epidemiology and prevention; AHA statistics committee; world heart federation council on epidemiology and prevention; the European Society of Cardiology Working Group on epidemiology and prevention; Centers for Disease Control and Prevention; and the National Heart, Lung, and Blood Institute. Circulation. 2003;108(20):2543–9.
Prineas RCR, Blackburn H. The Minnesota code manual of electrocardiographic findings: standards and procedures for measurement and classification. Boston, MA: Wright-OSG; 1982.
Tate J BJ, Bunk D, et al. Analytical characteristics of commercial and research cardiac troponin I and T assays declared by the manufacturer. 2012; http://www.ifcc.org/media/102202/IFCC_Troponin_Table_vDec_2010_FINAL_ug_L_28Jan11.pdf. Accessed September 24, 2017.
Safford MM, Parmar G, Barasch CS, et al. Hospital laboratory reporting may be a barrier to detection of ‘microsize’ myocardial infarction in the US: an observational study. BMC Health Serv Res Vol 132013:162.
Galasko GI, Lahiri A, Barnes SC, Collinson P, Senior R. What is the normal range for N-terminal pro-brain natriuretic peptide? How well does this normal range screen for cardiovascular disease? Eur Heart J. 2005;26(21):2269–76.
Levey AS, Stevens LA, Schmid CH, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12.
Prentice RL, Pyke R. Logistic disease incidence models and case-control studies. Biometrika. 1979;66(3):403–11.
Onland-Moret NC, van der AD, van der Schouw YT, et al. Analysis of case-cohort data: a comparison of different methods. J Clin Epidemiol. 2007;60(4):350–5.
Cushman M, Judd SE, Howard VJ, et al. N-terminal pro-B-type natriuretic peptide and stroke risk: the reasons for geographic and racial differences in stroke cohort. Stroke. 2014;45(6):1646–50.
Barlow WE, Ichikawa L, Rosner D, Izumi S. Analysis of case-cohort designs. J Clin Epidemiol. 1999;52(12):1165–72.
Lunn M, McNeil D. Applying cox regression to competing risks. Biometrics. 1995;51(2):524–32.
Rubin DBSN. Multiple imputation in health-care databases: an overview and some applications. Stat Med. 1991;10:585–98.
Thygesen K, Alpert JS, White HD, et al. Universal definition of myocardial infarction. Circulation. 2007;116(22):2634–53.
Thygesen K, Alpert JS, Jaffe AS, et al. Third universal definition of myocardial infarction. Eur Heart J. 2012;33(20):2551–67.
Mueller C. Biomarkers and acute coronary syndromes: an update. Eur Heart J. 2014;35(9):552–6.
Konstam MA. Natriuretic peptides and cardiovascular events: more than a stretch. Jama. Vol 297. United States2007:212–214.
Mills NL, Lee KK, McAllister DA, et al. Implications of lowering threshold of plasma troponin concentration in diagnosis of myocardial infarction: cohort study. BMJ (Clinical research ed). 2012;344:e1533.
Bonaca M, Scirica B, Sabatine M, et al. Prospective evaluation of the prognostic implications of improved assay performance with a sensitive assay for cardiac troponin I. J Am Coll Cardiol. 2010;55(19):2118–24.
Pastormerlo LE, Maffei S, Della Latta D, Chubuchny V, Susini C, Berti S, Clerico A, Prontera C, Passino C, Januzzi JL, Emdin M. N-terminal prob-type natriuretic peptide is a marker of vascular remodelling and subclinical atherosclerosis in asymptomatic hypertensives. Eur J Prev Cardiol. 2016;23(4):366–76.
Hopkins WE, Chen Z, Fukagawa NK, Hall C, Knot HJ, LeWinter MM. Increased atrial and brain natriuretic peptides in adults with cyanotic congenital heart disease: enhanced understanding of the relationship between hypoxia and natriuretic peptide secretion. Circulation. 2004;109(23):2872–7.
Tateishi JMM, Ohyanagi M, Iwasaki T. Transient increase in plasma brain (B-type) natriuretic peptide after percutaneous transluminal coronary angioplasty. Clin Cardiol. 2000;23:776–80.
Goetze JPGA, Moller CH, Steinbruchel DA, Rehfeld JF, Nielsen LB. Acute myocardial hypoxia increases BNP gene expression. FASEB J. 2004;18:1928–30.
Min NLP, Khaper N, Liu P. Inflammatory cytokines and Postmyocardial Infarcation remodeling. Circ Res. 2004;94:1543–53.
Tsuruda T, Boerrigter G, Huntley BK, et al. Brain natriuretic peptide is produced in cardiac fibroblasts and induces matrix metalloproteinases. Circ Res. 2002;91(12):1127–34.
Pauriah MKF, Lim TK, et al. B-type natriuretic peptide is an independent predictor of endothelial function in man. Clin Sci. 2012;123:307–12.
Luchner A, Hengstenberg C, Lowel H, Riegger GA, Schunkert H, Holmer S. Effect of compensated renal dysfunction on approved heart failure markers: direct comparison of brain natriuretic peptide (BNP) and N-terminal pro-BNP. Hypertension (Dallas, Tex. : 1979). 2005;46(1):118–23.
Dadu RT, Fornage M, Virani SS, et al. Cardiovascular biomarkers and subclinical brain disease in the atherosclerosis risk in communities study. Stroke. 2013;44(7):1803–8.
Mutlu U, Ikram MA, Hofman A, de Jong PT, Klaver CC, Ikram MK. N-terminal pro-B-type natriuretic peptide is related to retinal microvascular damage: the Rotterdam study. Arterioscler Thromb Vasc Biol. 2016;36(8):1698–702.
Bower JK, Lazo M, Matsushita K, et al. N-terminal pro-brain natriuretic peptide (NT-proBNP) and risk of hypertension in the atherosclerosis risk in communities (ARIC) study. Am J Hypertens. 2015;28(10):1262–6.
Natriuretic Peptides Studies C, Willeit P, Kaptoge S, et al. Natriuretic peptides and integrated risk assessment for cardiovascular disease: an individual-participant-data meta-analysis. The lancet. Diabetes & endocrinology. 2016;4(10):840–9.
Abdullah SM, Khera A, Das SR, et al. Relation of coronary atherosclerosis determined by electron beam computed tomography and plasma levels of n-terminal pro-brain natriuretic peptide in a multiethnic population-based sample (the Dallas heart study). Am J Cardiol. 2005;96(9):1284–9.
Gan L, Feng C, Liu C, Tian S, Song X, Yang L. Association between serum N-terminal pro-B-type natriuretic peptide levels and characteristics of coronary atherosclerotic plaque detected by coronary computed tomography angiography. Experimental and therapeutic medicine. 2016;12(2):667–75.
Ndrepepa G, Braun S, Mehilli J, et al. Plasma levels of N-terminal pro-brain natriuretic peptide in patients with coronary artery disease and relation to clinical presentation, angiographic severity, and left ventricular ejection fraction. Am J Cardiol. 2005;95(5):553–7.
Acknowledgements
The authors thank the other investigators, the staff, and the participants of the REGARDS study for their valuable contributions. A full list of participating REGARDS investigators and institutions can be found at http://www.regardsstudy.org.
Funding
This research project is supported by a cooperative agreement U01 NS041588 from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Department of Health and Human Service. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Neurological Disorders and Stroke or the National Institutes of Health. Representatives of the funding agency have been involved in the review of the manuscript but not directly involved in the collection, management, analysis or interpretation of the data. Dr. Sterling is supported by grant number T32HS000066 from the Agency for Healthcare Research and Quality. The content is solely the responsibility of the authors and does not necessarily represent the official views of the Agency for Healthcare Research and Quality.
Availability of data and materials
The data analyzed during the current study belong to REGARDS and further inquiry can be made at http://www.regardsstudy.org
Author information
Authors and Affiliations
Contributions
Study concept and design by MRS, RDW, MMS, EBL, SPG, TMB, JSR, MC Data analysis by JB and YK, with additional statistical expertise provided by EBL, JSR and GH Laboratory data and samples of NT-proBNP provided by laboratory of MC The drafting of the manuscript by MRS and MMS All authors read and approved the final manuscript and provided critical revisions.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was reviewed and approved by the University of Alabama at Birmingham Institutional Review Board and all participants provided written informed consent.
Competing interests
Dr. Durant receives support from Amgen related to the treatment of heart failure. He also receives research grant funding from Amarin related to primary and secondary prevention of myocardial infarction. Dr. Levitan receives research grants from Amgen related to treatment of heart failure and other cardiovascular disease (significant) and does consulting for Amgen and Novartis related to treatment of heart failure (modest). Dr. Brown receives Amgen support for research related to heart failure. Dr. Safford receives salary support for investigator-initiated research from Amgen, Inc. All other authors have no conflicts or competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional file
Additional file 1:
Figure S1. Selection of the Sub-Cohort in the Reasons for Geographic and Racial Differences in Stroke (REGARDS), Table S1. Cause- Specific Hazard Ratios for Nonfatal Microsize MI, Nonfatal Typical MI, and Fatal CHD according to Baseline Brain Natriuretic Peptide (NT-proBNP) Tertiles, Table S2. Cause- Specific Hazard Ratios for Nonfatal Microsize MI, Nonfatal Typical MI, and Fatal CHD according to Baseline Brain Natriuretic Peptide (NT-proBNP) Tertiles, Excluding Individuals with Possible Heart Failure (HF). (DOCX 98 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Sterling, M.R., Durant, R.W., Bryan, J. et al. N-terminal pro-B-type natriuretic peptide and microsize myocardial infarction risk in the reasons for geographic and racial differences in stroke study. BMC Cardiovasc Disord 18, 66 (2018). https://doi.org/10.1186/s12872-018-0806-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12872-018-0806-4