Abstract
Background
Vitamin D is an essential micronutrient for the overall health and well-being of individuals. For strong musculoskeletal and neurological development of human body, vitamin D levels during childhood and adolescence have key importance. This is the first national-level study that analyzes the deficiency and concentration of serum 25-Hydroxyvitamin D [25(OH)D)] among Indian children and adolescents with respect to various demographic and socioeconomic characteristics.
Methods
Data of Comprehensive National Nutrition Survey (CNNS, 2016–18) was utilized for the present study. Vitamin D levels were assessed based on serum 25-hydroxyvitamin D concentration. Prevalence of vitamin D deficiency has been shown for the three age groups: 0–4 years (n = 12,764), 5–9 years (n = 13,482), 10–19 years (n = 13,065). Vitamin D deficiency was defined as: serum 25(OH)D < 12 ng/mL; and insufficiency as: 12 ng/ml ≤ 25(OH) < 20 ng/ml. 25(OH) D level higher than 20 ng/mL was accepted as adequate. Random slope multilevel logistic regression models were employed to assess the demographic and socioeconomic correlates of vitamin D deficiency.
Results
Mean serum 25(OH)D concentration level was found to be 19.51 ± 8.76, 17.73 ± 7.91, and 17.07 ± 8.16 ng/ml in age group 0–4 years, 5–9 years and 10–19 years respectively. 49.12% of the children aged 0–4 years were having insufficient level of vitamin D. Prevalence of vitamin D deficiency was comparatively higher among female adolescents (76.16%), adolescents living in rural region (67.48), Sikh individuals (0–4 years: 76.28%; 5–9 years: 90.26%; 10–19 years: 89.56%), and adolescents coming from rich households. North-Indian individuals were having substantially higher odds of vitamin D deficiency in all the three age groups.
Conclusion
The present study demonstrated that the prevalence of vitamin D deficiency is considerably high among children and adolescents of India. The study highlights high-risk group which require prompt policy interventions.
Similar content being viewed by others
Introduction
Vitamin D deficiency is a serious public health problem prevalent worldwide among individuals of all geographic regions, age groups, ethnicities, and races [1]. Earlier, vitamin D was only considered to be important for the prevention of rickets in children, but the recent biomedical and epidemiological research show that vitamin D is essential for the overall health and well-being of individuals. Research shows that insufficient levels of vitamin D are associated with elevated risk of developing numerous skeletal and non-skeletal diseases like colon cancer [2], prostate cancer [3, 4], various other types of cancer [5,6,7,8,9], type-1 diabetes mellitus [10, 11], multiple sclerosis [12], rheumatoid arthritis [13], depression [14], schizophrenia [15], cardiovascular diseases [16], Obesity [17], infectious diseases [18], and various other diseases. Due to diverse and multidimensional impacts on overall health of individuals, vitamin D levels keep an important place in policy formation of a nation or organization.
Vitamin D is a fat-soluble vitamin that promotes mineral homeostasis and absorption of calcium, phosphorous, magnesium, iron, and zinc in the intestine [1]. It plays a pivotal role in maintaining adequate serum calcium and phosphate concentrations which ultimately helps in maintaining normal bone mineralization [19, 20]. Apart from this, it has also been found to be associated with regulation of insulin and glucose secretion [21, 22], and regulation of cardiac and renal functions. Increasing cellular immunity by stimulating production of anti-microbial peptide (cathelicidin) [23], reduction of inflammation, and modulation of cell growth [24] are also influenced by vitamin D.
High prevalence of vitamin D deficiency is being reported all around the world. According to cut off level of 25(OH)D < 20 ng/ml, 24% of the US, 37% of the Canada and 40% of the European population have low levels of vitamin D [25], however, the prevalence varies by age, gender, race, ethnicity, and socioeconomic status. Numerous small scale studies have reported a high prevalence of vitamin D deficiency in Indian subpopulations [26]. In spite of abundant sunshine and being from a tropical region, vitamin D deficiency is significantly high in India. The estimated prevalence of vitamin D deficiency in various population groups across India varies from 34 to 94% [27]; however, we did not found any large scale study which has provided nationally representative estimates of vitamin D deficiency.
Major skeletal and neurological development of the human body takes place during childhood and adolescence. For vigorous physical and mental development, vitamin D levels during childhood and adolescence have key importance. High prevalence of vitamin D deficiency has been reported among adolescents and children worldwide [28,29,30]. A few small scale studies on vitamin D deficiency among children and adolescents have been conducted in India, but none of them was nationally representative [19, 31]. Hence the present study makes an effort to comprehensively analyze the deficiency and levels of vitamin D among Indian children and adolescents with respect to various demographic and socioeconomic characteristics using nationally representative data. The study will also explore the demographic and socioeconomic correlates of vitamin D deficiency among adolescents using robust statistical analyses.
Methodology
Data
The present study utilizes the data of the Comprehensive National Nutrition Survey (CNNS, 2016–18). CNNS provides robust data on nutritional status, anthropometric indicators, food intake, and micronutrient levels of children and adolescents aged 0 to 19 years. The survey was the largest micronutrient survey globally. The CNNS was conducted under the stewardship of Ministry of Health and Family Welfare (MohFW), Government of India; technical support was provided by UNICEF, over field coordination training, and data analysis was conducted by Population Council. The survey adopted a multi-stage sampling design to collect data from 30 states of India. The data collection was done for three target groups: preschoolers (0–4 years), school-age children (5–9 years), and adolescents (10–19 years). The total planned national-level sample size was 122,100 children and adolescents from 2035 primary sampling units. For each of the three age groups, the planned sample size was 40,700 individuals for household survey and anthropometric measurements; and for biological samples, the sample size was 20,350 individuals from each group. The overall response rate for individual interviews was 95%; on the other hand, the response rates for biological sample collection were comparatively low: 63–64% in the three age groups. Detailed description of household selection, questionnaire, data collection, instruments used, and data handling can be accessed from the CNNS (2016–18) report [32].
Blood collection and serum 25(OH)D estimation
Parents and subjects were instructed regarding overnight fasting (8–10 h) 1 day before the sample collection. The venous blood samples were collected by trained phlebotomists. The status of fasting (yes/no) was also asked before the blood sample collection. The blood samples were transported to the nearest collection center in cold bags. There, the serum was separated and divided into aliquots within 6 h of sample collection. The aliquots were then stored at − 20 °C until the analysis. The 25(OH)D concentration was measured with an antibody competitive immunoassay using the chemiluminescence (Siemens Centaur) method. The biochemical analysis was performed by SRL labs. With standard internal and external quality assurance procedures, extensive quality control measures were taken during the data collection [32].
Sample size
Although the planned sample size was 20,350 individuals from each age group, but due to missing values, non-response, insufficient quality, and invalid observations, the final sample size of the study was reduced. For the 0–4 age group, the sample size was 12,764, for 5–9 age group 13,482, and for 10–19 age group, the sample size was 13,065. For the national representation of the estimates, sampling weights were utilized, which were provided in the CNNS dataset.
Outcome variable
Serum 25-hydroxyvitamin D [25(OH)D] is considered as the most reliable indicator of vitamin D levels in the human body [1]. The serum 25(OH)D concentration level reflects not only cutaneous synthesis of vitamin D but also dietary absorption of vitamin D. In the present study, therefore, 25(OH)D concentration level was taken as the principal outcome variable. There are two established cut-offs of 25(OH)D concentration for indication of vitamin D deficiency: < 12 ng/ml defined by National Academy of Medicine, USA and < 20 ng/ml defined by Endocrine Society, USA. However, most of the researchers follow criteria suggested by ‘Munns et al.’ [33]. According to their criteria, vitamin D deficiency is defined as serum 25(OH)D level of < 12 ng/mL and insufficiency as 25(OH) D level between 12 and 20 ng/mL. 25(OH) D level higher than 20 ng/mL was accepted as adequate. We have also used the criteria suggested by ‘Munns et al.’ to define vitamin D deficiency and insufficiency in this study [33]. For regression analysis a new binary variable was defined as 1 = “deficient” (< 12 ng/ml) and 0 = “Not deficient” (≥ 12 ng/ml).
Predictor variables
All the available demographic and socio-economic variables were included in the regression analysis as predictor variables. The variables are as follows: Age of the individual (in months), Gender (Male, Female), Place of residence (Urban, Rural), Wealth Index (Poorest, Poor, Middle, Rich, Richest), Religion (Hindu, Muslim, Christian, Sikh, Other), Caste (Scheduled Caste(SC), Scheduled Tribe (ST), Other Backward Class (OBC), and Others), Mothers Education Level (no education, < 5 years completed, 5–8 years completed, 9–11 years completed, ≥ 12 years completed), Region (North, Central, East, West, South, North-East). The results were controlled for BMI, cholesterol and seasonal variation. The results of the controlled variables are presented in supplementary file. (Note: The wealth index was calculated on the basis of possession of common household items and facilities as described in National Family Health Survey - 4 [34].)
Statistical analyses
The association between vitamin D deficiency and demographic & socioeconomic variables was assessed using two-level random slope logistic regression models. As the data was hierarchical in nature and observations were clustered within PSUs, there were high chances that the observations were correlated within PSUs. So a simple logistic regression might suffer from intra-cluster correlation and provide less reliable estimates. This issue can be solved using a multilevel model that will not only control for intra-cluster correlation but also community variables like development level, political profile, climatic conditions, etc. PSUs were set as level-2 in the multilevel logistic regression model. Variance inflation factors were calculated to detect any kind of multi-collinearity in the model. No evidence of multi-collinearity was found in the analysis. All the statistical analyses were performed on STATA 16 [35].
Results
Table 1 is showing the age group wise prevalence of vitamin D deficiency, insufficiency and mean serum 25(OH)D. The prevalence of vitamin deficiency was 14, 19 and 24% in the age groups 0–4, 5–9 and 10–19 respectfully. 68% of the adolescents were having insufficient levels of vitamin D. Mean serum 25(OH)D level was highest in 0–4 years age group and lowest in 10–19 years age group.
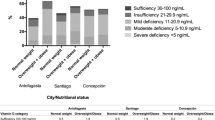
Table 2 illustrates average concentration levels of serum 25(OH)D by background characteristics among Indian children and adolescents. In all the three age groups, the 25(OH)D levels were higher for males than females. The levels of 25(OH)D were lower among urban individuals compared to rural individuals. The 25(OH)D levels were substantially low among Sikh individuals in all the three age groups. Children and adolescents of the northern region of the country were having significantly low levels of 25(OH)D; on the other hand, individuals of the southern region were having comparatively high levels of 25(OH)D.
Figure 1 is showing the choropleth maps of vitamin D deficiency in India according to cut-off level of serum 25(OH)D < 12 ng/mL. From the graphs, it can be clearly visualized that the prevalence of vitamin D deficiency is comparatively low in southern and north-eastern regions of the country and very high in northern and western regions of the country.
The prevalence of vitamin D deficiency with respect to demographic and socioeconomic characteristics is presented in Table 3. In the age group 0–4 and 5–9, there was not much difference in the prevalence of deficiency between males and females, however, in 10–19 years age group the prevalence was very high among female adolescents compared to male adolescents. Vitamin D deficiency was more prevalent among children and adolescents of rich households compared to adolescents of poor households. The prevalence was substantially high among Sikh children; 89.59% of the Sikh children of age group 10–19 years were having insufficient levels of vitamin D.
The results of multilevel logistic regressions are presented in Table 4. Compared to males, females were having 1.54 (OR: 1.54; 95% CI: 1.39–1.71) and 3.8 (OR: 3.8; 95% CI: 3.42–4.22) times higher odds of being vitamin deficient in 5–9 and 10–19 years age group respectively. Results show that in the three age groups the odds of being vitamin D deficient are significantly higher among urban individuals compared to rural individuals. Wealth Index did not found to be strongly associated with vitamin D deficiency among children of 0–4 age group, however, in 5–9 and 10–19 years, age group the individuals of the richest households were having 56% (OR: 1.56; 95% CI: 1.14–2.14) and 65% (OR: 1.65; 95% CI: 1.25–2.18) higher odds of being vitamin D deficient respectively compared to individuals of the poorest households. Children of Sikh family were at high risk of vitamin D deficiency, the odds of having vitamin D deficiency were 2.1 (OR: 2.1; 95% CI: 1.39–3.19) times higher among 10–19 year old adolescents of Sikh family compared to adolescents of Hindu family. Children and adolescents of ST households were having significantly lower odds of being vitamin D deficient compared to other caste groups. Geographical region of the country was strongly associated with vitamin D deficiency among children and adolescents. As the mean 25(OH)D levels were highest in southern region so we took south region of the country as the base category. The risk of vitamin D deficiency was highest in northern region, a 5–9 year old individual living in northern region of the country was 10.4 (OR: 10.44; 95% CI: 7.76–14.05) times more likely to be vitamin D deficient compared to a 5–9 year old individual living in southern region. In 4–9 and 5–9 year age group, age (in months) of the child was positively associated with odds of vitamin D deficiency, in both the age groups with 1 month increase in age was associated with 1% (OR: 1.01; 95% CI: 1.005–1.015) increase in odds of vitamin D deficiency; however, in 10–19 years age group the association was other way round i.e. with 1 month increase in age there was decrement of 1% (OR: 0.997; 95% CI: 0.9954–0.9983) in odds of being vitamin D deficient. The intra-class correlation was statistically significant in all the three regression models.
Discussion
In the present study, we have tried to assess the serum 25(OH)D profile and vitamin D deficiency of Indian children and adolescents. Up to the best of our knowledge, this is the first national-level study of vitamin D deficiency among children and adolescents in India to date. The study finds a significantly high prevalence of vitamin D deficiency in all the three age groups; however, the prevalence was highly variable between the demographic and socioeconomic categories.
Ultraviolet B (UVB) (290-320 nm) radiation from sunlight plays the most crucial role in the production of vitamin D3(cholecalciferol) in the human body. Cutaneous exposure of UVB is channelized through numerous Individual factors such as skin pigmentation (melanin concentration in the skin), clothing behavior, use of sunscreen creams, sun avoidant lifestyle, etc. In the present study also, variation in serum 25(OH)D concentration level might be explained by extent of sunlight exposure among individuals of various demographic and socioeconomic categories. Like some European and middle-eastern countries, there is no policy of vitamin D fortification of food products in India; hence sunlight exposure and skin synthesis is the main source of vitamin D production in the body among the Indians. The present study shows that the prevalence of vitamin D deficiency was higher in rural areas compared to urban areas; this can be simply explained by the fact that people living in rural areas are more exposed to sunlight compared to people living in urban areas. Most of the people in rural areas do agricultural work and their children also help them in the field, exposing them to sunlight for a significant amount of time; on the other hand, people in urban areas generally try to keep their children away from sunlight. Similarly, we also found that serum 25(OH)D concentration levels are considerably high among poor people compared to rich people; again the main factor is lifestyle: generally, rich people in India have sun avoidant lifestyle, on the other hand, poor people’s lifestyle makes them exposed to sunlight which ultimately leads to higher concentrations of serum 25(OH)D. similar kinds of results were found in a study conducted on healthy school girls of Delhi [31].
Among adolescents, serum 25(OH)D concentration was substantially higher among males compared to females. Generally, males are more involved in outdoor activities than females in India, which might be one of the reasons of elevated serum 25(OH)D concentration among males. Apart from that, use of sunscreen products and sun avoidant behavior is more common among females than males [36]. Similar results are found in numerous previous studies [36,37,38]. However, in some other studies, the results were other way round, i.e. serum 25(OH)D levels were higher among females compared to males [39, 40].
We also observed that vitamin D deficiency was alarmingly high among Sikh children and adolescents. From the literature, we did not find any convincing explanation of low vitamin D levels among Sikh individuals. Further research on causes and correlates of low serum 25(OH)D levels among Sikh individuals is required.
Results of the present study reveal that the concentration of serum 25(OH)D was higher among individuals of the southern region of the country and substantially low among individuals of the northern region of the country, even when urbanization is higher in southern India compared to northern India. There can be numerous reasons for this, but the most convincing reason we found was ‘Ultraviolet Index’ (UV Index); UV index tells us the expected amount of UV radiation that will reach the earth’s surface at the time when the sun is highest in the sky. The amount of UV radiation reaching the surface is affected by elevation of the sun in the sky, the amount of ozone in the stratosphere, and the amount of cloud cover. The UV index ranges from 0 to 13: higher the UV index higher the amount of UV radiation reaching the surface. The UV index in northern region of India ranges from 3 to 7, on the other hand, UV index in southern region of the country varies from 6 to 13 [41] i.e. the amount of UV radiation exposure is much higher in southern India compared to northern India. This might be one of the major reasons of higher vitamin D levels among southern India Individuals. Another point is that northern India comprises of states like Himachal Pradesh and Jammu Kashmir which have hilly landscapes and cold weather i.e. people wear full clothes to keep them warm resulting in less exposure to sunlight.
Though exposure to sunlight is indeed very important for the production of vitamin D in the body but exposure to UV radiation has some serious side effects also. It is a well-established fact that chronic exposure to Ultraviolet-B (UV-B) radiation can increase the risk of nonmelanoma skin cancer (NMSC) in humans [42]. UV-B radiation of 290 to 320 wavelength present in the solar spectrum can cause erythema, burns, damage in DNA, and skin cancer [42]. That is why direct exposure of sunlight to skin is not recommended by doctors and scientists, especially during peak hours (mid-day); however, early morning and late evening sunlight is considered safe, healthy, and beneficial [43, 44].
From the literature, there are a few recommendations to deal with vitamin D deficiency among children and adolescents in India:
-
Fortification of food products with vitamin D: Fortification is a well-known strategy to deal with deficiency of any micronutrient in the population [45]. The government can introduce protocols for mandatory or voluntary fortification of selected food products. Fortification of food staple by government mandate is the most effective method of increasing dietary intake of a particular micronutrient in the population [45]. Currently, there is mandatory vitamin D fortification programs for specific food products are running in Canada and United States [46].
-
Vitamin D supplementation: Vitamin D supplementation to the target groups in the form of tablets, capsules, drops can be a potential way to elevate vitamin D levels among the high-risk groups. Supplementation of 400 IU/day to breast-feeding infants is extensively recommended and practiced in numerous first world countries like Canada and United States [24, 33]. However, the WHO does not recommend routine supplementation of vitamin D to children.
-
Health education regarding sunlight: Government can promote awareness regarding the benefits of sunlight through mass media like radio, television and social media. Previously Indian government has run various health awareness programs pertaining to polio, HIV, tuberculosis, etc. Similarly, a well-structured program focusing on key points like the best time for sunlight exposure, detrimental effects of vitamin D deficiency, and the importance of vitamin D in the body can help in increasing awareness in the population.
-
A well-structured school level program focusing on outdoor physical activities for a specific period of time during school hours can be instrumental in dealing with vitamin D deficiency among children and adolescents.
Limitations
The unavailability of data on important aspects related to vitamin D was one of the major limitations of the study. One of the most important factors that affect vitamin D levels in the body is the amount of time spent in sunlight, and CNNS does not provide information on this, that is why we could not control for it in regression analysis, which puts the results on risk of omitted variable bias.
Conclusion
The present study portrays the national level profile of serum 25(OH)D among children and adolescents of India. In conclusion, it can be said that there is significant level of vitamin D deficiency among children and adolescents in India, and certain demographic and socioeconomic groups are at a very high risk of complications related to vitamin D deficiencies. Exposure to sunlight has a very important role in channelizing vitamin D levels among Indian children and adolescents. We believe that the results of the present study have important policy implications.
Availability of data and materials
The dataset utilized in the present study can be accessed from Population Council (India) on reasonable request basis.
Abbreviations
- CNNS:
-
Comprehensive National Nutrition Survey
- 25(OH)D:
-
25-Hydroxyvitamin-D
- UV-B:
-
Ultra Violet – B
- IU/day:
-
International Unit per day
- BMI:
-
Body Mass Index
- ng/ml:
-
Nanograms per milliliter
- nmol/liter:
-
Nanomoles per liter
- SC:
-
Scheduled Caste
- ST:
-
Scheduled Tribe
- OBC:
-
Other Backward Category
References
Holick MF, Vitamin D. Deficiency. N Engl J Med. 2007;357(3):266–81. https://doi.org/10.1056/NEJMra070553.
Garland CF, Garland FC, Shaw EK, Comstock GW, Helsing KJ, Gorham ED. Serum 25-Hydroxyvitamin D and colon cancer: eight-year prospective study. Lancet. 1989;334(8673):1176–8. https://doi.org/10.1016/S0140-6736(89)91789-3.
Jemal A, Ward E, Wu X, Martin HJ, McLaughlin CC, Thun MJ. Geographic patterns of prostate cancer mortality and variations in access to medical care in the United States. Cancer Epidemiol Biomark Prev. 2005;14(3):590–5. https://doi.org/10.1158/1055-9965.EPI-04-0522.
Ahonen MH, Tenkanen L, Teppo L, Hakama M, Tuohimaa P. Prostate cancer risk and prediagnostic serum 25-hydroxyvitamin D levels (Finland). Cancer Causes Control. 2000;11(9):847–52. https://doi.org/10.1023/A:1008923802001.
Grant WB. An estimate of premature cancer mortality in the U.S. due to inadequate doses of solar ultraviolet-B radiation. Cancer. 2002;94(6):1867–75. https://doi.org/10.1002/cncr.10427.
Grant WB, Garland CF. The Association of Solar Ultraviolet B (UVB) with Reducing Risk of Cancer: Multifactorial Ecologic Analysis of Geographic Variation in Age-adjusted Cancer Mortality Rates. Anticancer Res. 2006;26(4A).
Garland CF, Garland FC, Gorham ED, Lipkin M, Newmark H, Mohr SB, et al. The role of vitamin D in cancer prevention. Am J Public Health. 2006;96(2):252–61. https://doi.org/10.2105/AJPH.2004.045260.
Garland C, Barrett-Connor E, Rossof AH, Shekelle RB, Criqui MH, Paul O. Dietary vitamin D and calcium and risk of colorectal cancer: a 19-year prospective study in men. Lancet. 1985;325(8424):307–9. https://doi.org/10.1016/S0140-6736(85)91082-7.
Lappe JM, Travers-Gustafson D, Davies KM, Recker RR, Heaney RP. Vitamin D and calcium supplementation reduces cancer risk: results of a randomized trial. Am J Clin Nutr. 2007;85(6):1586–91. https://doi.org/10.1093/ajcn/85.6.1586.
Zipitis CS, Akobeng AK. Vitamin D supplementation in early childhood and risk of type 1 diabetes: a systematic review and meta-analysis. Arch Dis Child. 2008;93(6):512–7. https://doi.org/10.1136/adc.2007.128579.
Hyppönen E, Läärä E, Reunanen A, Järvelin MR, Virtanen SM. Intake of vitamin D and risk of type 1 diabetes: a birth-cohort study. Lancet. 2001;358(9292):1500–3. https://doi.org/10.1016/S0140-6736(01)06580-1.
Munger KL, Zhang SM, O’Reilly E, et al. Vitamin D intake and incidence of multiple sclerosis. Neurology. 2004;62(1):60–5. https://doi.org/10.1212/01.WNL.0000101723.79681.38.
Merlino LA, Curtis J, Mikuls TR, Cerhan JR, Criswell LA, Saag KG. Vitamin D intake is inversely associated with rheumatoid arthritis: results from the Iowa Women’s health study. Arthritis Rheum. 2004;50(1):72–7. https://doi.org/10.1002/art.11434.
Gloth FM, Alam W, Hollis B. Vitamin D vs broad spectrum phototherapy in the treatment of seasonal affective disorder. J Nutr Health Aging. 1999;3(1):5–7 https://jhu.pure.elsevier.com/en/publications/vitamin-d-vs-broad-spectrum-phototherapy-in-the-treatment-of-seas-3. Accessed February 2, 2021.
McGrath J, Selten JP, Chant D. Long-term trends in sunshine duration and its association with schizophrenia birth rates and age at first registration - data from Australia and the Netherlands. Schizophr Res. 2002;54(3):199–212. https://doi.org/10.1016/S0920-9964(01)00259-6.
Wallis DE, Penckofer S, Sizemore GW. The sunshine deficit and cardiovascular disease. Circulation. 2008;118(14):1476–85. https://doi.org/10.1161/CIRCULATIONAHA.107.713339.
Wortsman J, Matsuoka LY, Chen TC, Lu Z, Holick MF. Decreased bioavailability of vitamin D in obesity. Am J Clin Nutr. 2000;72(3):690–3. https://doi.org/10.1093/ajcn/72.3.690.
Bouillon R, Bischoff-Ferrari H, Willett W. Vitamin D and health: perspectives from mice and man. J Bone Miner Res. 2008;23(7):974–9. https://doi.org/10.1359/jbmr.080420.
Marwaha RK, Tandon N, Reddy DRH, et al. Vitamin D and bone mineral density status of healthy schoolchildren in northern India. Am J Clin Nutr. 2005;82(2):477–82. https://doi.org/10.1093/ajcn.82.2.477.
DeLuca HF. The transformation of a vitamin into a hormone: the vitamin D story. Harvey Lect. 1979;75:333–79 https://pubmed.ncbi.nlm.nih.gov/400608/. Accessed February 2, 2021.
Garbossa SG, Folli F. Vitamin D, sub-inflammation and insulin resistance. A window on a potential role for the interaction between bone and glucose metabolism. Rev Endocr Metab Disord. 2017;18(2):243–58. https://doi.org/10.1007/s11154-017-9423-2.
Maestro B, Campión J, Dávila N, Calle C. Stimulation by 1,25-dihydroxyvitamin D3 of insulin receptor expression and insulin responsiveness for glucose transport in U-937 human promonocytic cells. Endocr J. 2000;47(4):383–91. https://doi.org/10.1507/endocrj.47.383.
Liu PT, Stenger S, Li H, et al. Toll-like receptor triggering of a vitamin D-mediated human antimicrobial response. Science. 2006;311(5768):1770–3. https://doi.org/10.1126/science.1123933.
Calcium I of M (US) C to RDRI for VD, Ross AC, Taylor CL, Yaktine AL, Del Valle HB. Dietary Reference Intakes for Calcium and Vitamin D: National Academies Press; 2011. https://doi.org/10.17226/13050.
Amrein K, Scherkl M, Hoffmann M, Neuwersch-Sommeregger S, Köstenberger M, Tmava Berisha A, et al. Vitamin D deficiency 2.0: an update on the current status worldwide. Eur J Clin Nutr. 2020;74(11):1498–513. https://doi.org/10.1038/s41430-020-0558-y.
Harinarayan CV, Joshi SR. Vitamin D status in India - Its implications and remedial measures. J Assoc Physicians India. 2009;57(JAN):40–8 https://pubmed.ncbi.nlm.nih.gov/19753759/. Accessed March 1, 2021.
Aparna P, Muthathal S, Nongkynrih B, Gupta S. Vitamin D deficiency in India. J Fam Med Prim Care. 2018;7(2):324–30. https://doi.org/10.4103/jfmpc.jfmpc_78_18.
Lehtonen-Veromaa M, Möttönen T, Irjala K, Kärkkäinen M, Lamberg-Allardt C, Hakola P, et al. Vitamin D intake is low and hypovitaminosis D common in healthy 9- to 15-year-old Finnish girls. Eur J Clin Nutr. 1999;53(9):746–51. https://doi.org/10.1038/sj.ejcn.1600844.
Bemanalizadeh M, Heidari-Beni M, Ejtahed HS, Heshmat R, Baygi F, Seif E, et al. Association of serum 25-hydroxyvitamin D concentration with anthropometric measures in children and adolescents: the CASPIAN-V study. Eat Weight Disord. 2020:1–8. https://doi.org/10.1007/s40519-020-01067-3.
Gordon CM, DePeter KC, Feldman HA, Grace E, Emans SJ. Prevalence of vitamin D deficiency among healthy adolescents. Arch Pediatr Adolesc Med. 2004;158(6):531–7. https://doi.org/10.1001/archpedi.158.6.531.
Puri S, Marwaha RK, Agarwal N, Tandon N, Agarwal R, Grewal K, et al. Vitamin D status of apparently healthy schoolgirls from two different socioeconomic strata in Delhi: relation to nutrition and lifestyle. Br J Nutr. 2008;99(4):876–82. https://doi.org/10.1017/S0007114507831758.
Comprehensive National Nutrition Survey (2016–2018); 2018. https://nhm.gov.in/showfile.php?lid=712.
Aguiar M, Atapattu N, Bhatia V, et al. Global consensus recommendations on prevention and management of nutritional rickets. J Clin Endocrinol Metab. 2016;101(2):394–415. https://doi.org/10.1210/jc.2015-2175.
NFHS-4 (2015–16), INDIA.; 2017. http://www.rchiips.org/nfhs. Accessed February 14, 2019.
StataCorp. 2019.
Verdoia M, Schaffer A, Barbieri L, di Giovine G, Marino P, Suryapranata H, et al. Impact of gender difference on vitamin D status and its relationship with the extent of coronary artery disease. Nutr Metab Cardiovasc Dis. 2015;25(5):464–70. https://doi.org/10.1016/j.numecd.2015.01.009.
Al-Horani H, Abu Dayyih W, Mallah E, et al. Nationality, gender, age, and body mass index influences on Vitamin D concentration among elderly patients and young Iraqi and Jordanian in Jordan. Biochem Res Int. 2016;2016:1–8. https://doi.org/10.1155/2016/8920503.
Shchubelka K. Vitamin D status in adults and children in Transcarpathia, Ukraine in 2019. BMC Nutr. 2020;6(1):48. https://doi.org/10.1186/s40795-020-00380-5.
AlQuaiz AJM, Kazi A, Fouda M, Alyousefi N. Age and gender differences in the prevalence and correlates of vitamin D deficiency. Arch Osteoporos. 2018;13(1):1–11. https://doi.org/10.1007/s11657-018-0461-5.
Sanghera DK, Sapkota BR, Aston CE, Blackett PR. Vitamin D status, gender differences, and Cardiometabolic health disparities. Ann Nutr Metab. 2017;70(2):79–87. https://doi.org/10.1159/000458765.
Weather Maps: UV index India | WeatherOnline. https://www.weatheronline.in/cgi-app/weathercharts?LANG=in&CONT=inin&MAPS=uv. Accessed February 2, 2021.
Ananthaswamy HN. Sunlight and skin cancer. J Biomed Biotechnol. 2001;2001(2):49. https://doi.org/10.1155/S1110724301000122.
Mead MN. Benefits of Sunlight: A Bright Spot for Human Health. Environ Health Perspect. 2008;116(4). https://doi.org/10.1289/ehp.116-a160.
Barolet D, Christiaens F, Hamblin MR. Infrared and skin: friend or foe. J Photochem Photobiol B Biol. 2016;155:78–85. https://doi.org/10.1016/j.jphotobiol.2015.12.014.
Whiting SJ, Calvo MS. Vitamin D Fortification and Supplementation Policies to Correct Vitamin D Insufficiency/Deficiency Globally. In: Vitamin D: Fourth Edition, vol. 2: Elsevier Inc; 2017. p. 91–108. https://doi.org/10.1016/B978-0-12-809963-6.00062-6.
Cheney MC. Canadian experience with food fortification. In: Public Health Reviews, vol. 28: Public Health Rev; 2000. p. 171–7. https://pubmed.ncbi.nlm.nih.gov/11411271/. Accessed February 2, 2021.
Acknowledgments
The authors are deeply thankful to Population Council for sharing the data for this study.
Funding
The present study did not receive any financial support from any funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AM and CS were responsible for conceptualization and study design. AM collected the data, analyzed the data, and drafted the manuscript. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The ethical approval to the survey were provided by the Population Council’s International Review Board (New York, USA) and ethics committee of the Post Graduate Institute of Medical and Research (Chandigarh, India) [32]. For children less than 10 years old, written informed consent was taken from parent/caregiver. For adolescents 11–17 years old, the informed consent was taken from parents/caregiver as well as the adolescents. Written informed consent was taken from adolescents > 17 years of age. The blood sample collection was in accordance with the relevant guidelines and regulations [32].
Consent for publication
Not applicable.
Competing interests
None of the authors have any conflict of interest to declare.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplementary Table S1: Results of logistic regression assessing odds of vitamin D deficiency in categories of the controlled variables.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mustafa, A., Shekhar, C. Concentration levels of serum 25-Hydroxyvitamin-D and vitamin D deficiency among children and adolescents of India: a descriptive cross-sectional study. BMC Pediatr 21, 334 (2021). https://doi.org/10.1186/s12887-021-02803-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12887-021-02803-z