Abstract
Whereas HER2 amplification is a well-known phenomenon in breast tumours, its frequency and clinical importance in ovarian cancer have not been established. The aim of the study was to compare the frequency of HER2 amplification in hereditary (BRCA-positive) and sporadic (BRCA-negative) ovarian tumours and to estimate the association of this gene alteration on clinical outcome in ovarian cancer patients. We analysed HER2 amplification in 53 ovarian tumours: 20 from mutation carriers (18 in BRCA1 and 2 in BRCA2 gene) and 33 from non-carriers. Fluorescence in situ hybridization for HER2 was performed on 'touch' slides from frozen tumour samples or formalin-fixed, paraffin-embedded tissue. Our results indicate that high amplification (HER2: centromere ratio>5) is an infrequent phenomenon in ovarian tumours (6/53 cases). It occurs in both hereditary (4/20) and sporadic (2/33) tumours and no difference in the frequency of HER2 amplification exists between these groups. There is no significant difference in the clinical outcome of patients with HER2 amplified and non-amplified tumours (p = 0.3). Our results suggest a different biological role of HER2 amplification in ovarian and breast cancer.
Similar content being viewed by others
Introduction
HER2 amplification is a well-known phenomenon in breast tumours and its clinical importance is established in these malignancies. It was observed that patients with HER2-amplification in breast cancer tissue showed shorter disease-free time intervals and they benefit from therapy with the anti-Her-2/neu antibody, Herceptin [6, 19, 25].
It was suggested that the presence of amplification of HER2 is associated with the advanced clinical stage of ovarian cancer and does not occur in borderline and early stage disease [10, 29]. Some studies reported a significant difference in overall survival between women with HER2 negative and positive tumours [2, 7, 22] in contrast to later studies which demonstrated that HER2 over-expression had no relationship with prognosis [3, 5, 17, 21]. At present, there are few published reports of the clinical significance of HER2 amplification, demonstrated by the FISH techniques, in ovarian tumours, and the predictive value of HER2 assessment has not been demonstrated.
There is evidence that germline mutations in the BRCA1/2 genes confers increased susceptibility to breast and ovarian cancer. It is suggested that a germ-line mutation in the BRCA1 gene is associated with a significantly lower level of HER2 amplification in breast tumours [1, 9, 19, 25]. Similarly, it was noticed that BRCA-linked ovarian carcinomas and serous carcinoma of the peritoneum seemed to develop through a unique pathway of tumorigenesis that does not involve mutation in K-RAS or HER2 and C-MYC amplification [20, 24]. Some authors, however, did not notice differences in HER2 expression between BRCA-linked ovarian cancer carriers and ovarian cancer as control [15].
The aim of the study was to compare the frequency of HER2 amplification in hereditary and sporadic ovarian tumours and to estimate the influence of this gene alteration on clinical outcome in cancer patients.
Methods
In the present study we analysed 53 ovarian tumour tissue sections: 20 from BRCA mutation carriers and 33 from non-carriers. In the group of carriers there were 18 women with BRCA1 and two with BRCA2 germline mutation. All patients were diagnosed and operated on at the Department of Gynaecology, Institute of Obstetrics and Gynaecology, Medical University of Gdańsk. All cases represented a histological type of serous adenocarcinoma. There were four patients diagnosed in FIGO stage I, three in II, 35 in III and 11 in stage IV.
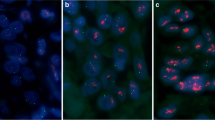
Fluorescence in situ hybridization (FISH) for HER2 was performed on 'touch' slides from frozen tumour samples or formalin-fixed, paraffin-embedded tissue slides.
HER2/NEU/Alphasatellite17 cocktail dual-color probe (Q-Biogene) was used for FISH analysis. The HER2/NEU probe labelled with Rhodamine contains DNA sequences specific for the HER2/NEU human gene locus and hybridized to human chromosome 17q12 and chromosome 17 enumeration probe labelled with Fluorescein contains α-satellite DNA that is targeted to the centromeric region of chromosome 17 (CEP17). Deparaffinization, in situ hybridization and staining were performed as per the manufacturer's protocols (Q-Biogene). Fluorescent signals were scored using a Zeiss Axioplan microscope with an ×100 planar objective, using a triple band-pass filter that permits simultaneous blue, green and red colours.
In each sample, an average of 100 non-overlapping interphase nuclei were scored. Because an increase in number of chromosome 17 homologues is a frequent phenomenon in ovarian tumours, the CE-P17 probe was used as an internal control in dual hybridization with the HER2/NEU probe. Tumours with a HER2/NEU: CEP17 signal ratio of <2 were considered to be non-amplified, whereas those with a ratio of 2 or greater were considered to have low amplification (2-3), moderate amplification (3.1-5), or high amplification (>5).
The Kaplan-Meier method and the log-rank test were used to identify predictors for outcome. Demographic and disease characteristics were compared between BRCA-associated and sporadic ovarian cancer patients and between HER2-amplified and non-amplified cases using the χ2 square test.
Results
FISH analysis demonstrated HER2 gene amplification in 10 (19%) cases (Table 1). Our results indicate that high amplification (HER2:centromere ratio>5) is an infrequent phenomenon in ovarian tumours. High amplification was observed in six (11%) out of 53 cases (two sporadic and four hereditary), whereas moderate and low amplification were observed in one (2%) and three (6%) tumours respectively.
No significant differences in the frequency of HER2 amplification were identified in hereditary (BRCA-positive) and sporadic (BRCA-negative) tumours (p = 0.2).
No association was observed between HER2 amplification and age of onset, serum Ca-125 level before therapy, FIGO stage, tumour grade and histological type. There was also no association between HER-positive and negative cases in outcome (overall survival and response to chemotherapy) (Fig. 1). Narrowing the examined group to FIGO III/IV patients (46 cases), we also did not notice any influence of HER2 status on outcome.
Discussion
Previous studies indicated that a high level of HER2 oncogene amplification did not occur or was not frequent in breast and ovarian tumours of BRCA mutation carriers. In contrast, HER2 was relatively highly amplified in sporadic breast or ovarian tumours [1, 9, 19, 20]. At present, there are few published papers on the frequency of HER2 amplification in hereditary and sporadic ovarian tumours. Our study did not reveal any difference in the frequency of HER2 amplification between BRCA-linked or sporadic ovarian cancers. Similar results were presented by Lakhani et al. [15] on the basis of immunochemical analysis of 178 BRCA1 and 29 BRCA2 mutation carriers and 235 controls.
The frequency of HER2 amplified breast and ovarian tumours varies depending on applied methods. There are two basic techniques applied for the examination of HER2 amplification: immunohistochemical (IHC) and fluorescence in situ hybridization (FISH). High concordance is observed between FISH and IHC results, especially in positive cases scored in IHC as 3+ and in negative cases. However, a substantial number of cases showed discrepant results from these two methods [13, 16, 23]. HER2 amplification/over-expression has been reported in 20-30% of human breast cancers and in 7-50% of ovarian cancers [3, 15, 18, 21, 26]. We decided to apply the FISH technique as it is a precise and reliable method. FISH offers a clear advantage over IHC, as it is reproducible and less susceptible to variations in tissue fixation and processing. It allows us to estimate the degree of amplification, gathering cases in groups depending on how many signals occur in the cellular nuclei. On the basis of published studies, we used the HER2/NEU:centromere 17 fluorescence ratio of 2 as the cutoff [8, 9, 17, 23].
On the basis of immunohistochemical analysis, it was observed that HER2 over-expression increased the risk of mortality in ovarian cancer patients [18]. Similar studies based on the chromogenic in situ hybridization (CISH) method revealed that amplification (>5 copies per cell) has a significant influence on survival [16]. Moreover, further results showed that HER2 over-expression has a prognostic value both in univariate and multivariate survival analysis [12, 28, 4, 11]. Some authors, however, did not observe a correlation between HER2 expression and survival or observed such a correlation only in selected groups of patients [5, 14, 21, 26, 27]. The multi-centre study provided on 361 Caucasian patients indicates that HER2 over-expression is a predictive factor for the response to first-line chemotherapy but has no significant influence on overall and disease-free survival independent of FIGO stage and tumour grade [21]. Our study, based on the FISH method, found neither an association between HER2 amplification and outcome nor any influence on response to chemotherapy. This study demonstrated that HER2 amplification in ovarian tumours was not a prognostic risk factor, suggesting a different biological role of HER2 from that previously demonstrated in breast cancer.
References
Adem C, Soderberg CL, Hafner K, Reynolds C, Slezak JM, Sinclair CS, Sellers TA, Schaid DJ, Couch F, Hartmann LC, Jenkins RB: ERBB2, TBX2, RPS6KB1, and MYC alterations in breast tissues of BRCA1 and BRCA2 mutation carriers. Genes Chromosomes Cancer 2004, 41: 1–11. 10.1002/gcc.20057
Berchuck A, Kamel A, Whitaker R, Kerns B, Olt G, Kinney R, Soper JT, Dodge R, Clarke-Pearson DL, Marks P, et al.: Overexpression of HER-2/neu is associated with poor survival in advanced epithelial ovarian cancer. Cancer Res 1990, 50: 4087–4091.
Bookman MA, Darcy KM, Clarke-Pearson D, Boothby RA, Horowitz IR: Evaluation of monoclonal humanized anti-HER2 antibody, trastuzumab, in patients with recurrent or refractory ovarian or primary peritoneal carcinoma with overexpression of HER2: a phase II trial of the Gynecologic Oncology Group. J Clin Oncol 2003, 21: 283–290. 10.1200/JCO.2003.10.104
Camilleri-Broet S, Hardy-Bessard AC, Le Tourneau A, Paraiso D, Levrel O, Leduc B, Bain S, Orfeuvre H, Audouin J, Pujade-Lauraine E, GINECO group: HER-2 overexpression is an independent marker of poor prognosis of advanced primary ovarian carcinoma: a multicenter study of the GINECO group. Ann Oncol 2004, 15: 104–112. 10.1093/annonc/mdh021
Chan JK, Loizzi V, Magistris A, Lin F, Rutgers J, Osann K, Disaia PJ, Berman ML: Differences in prognostic molecular markers between women over and under 45 years of age with advanced ovarian cancer. Clin Cancer Res 2004, 10: 8538–8543. 10.1158/1078-0432.CCR-04-0626
Espinosa AB, Tabernero MD, Garcia-Macias MC, Primo D, Bernal AG, Cruz JJ, Ramos M, Font de Mora J, Gomez Alonso A, Orfao A: Her-2/neu gene amplification in familial vs sporadic breast cancer. Impact on the behavior of the disease. Am J Clin Pathol 2003, 120: 917–27. 10.1309/5H778W5K75CMM03W
Felip E, Del Campo JM, Rubio D, Vidal MT, Colomer R, Bermejo B: Overexpression of c-erbB-2 in epithelial ovarian cancer. Prognostic value and relationship with response to chemotherapy. Cancer 1995, 75: 2147–2152. 10.1002/1097-0142(19950415)75:8<2147::AID-CNCR2820750818>3.0.CO;2-8
Gong Y, Booser DJ, Sneige N: Comparison of HER-2 status determined by fluorescence in situ hybridization in primary and metastatic breast carcinoma. Cancer 2005, 103: 1763–1769. 10.1002/cncr.20987
Grushko TA, Blackwood MA, Schumm PL, Hagos FG, Adeyanju MO, Feldman MD, Sanders MO, Weber BL, Olopade OI: Molecular-cytogenetic analysis of HER-2/neu gene in BRCA1 -associated breast cancers. Cancer Res 2002, 62: 1481–1488.
Heinrich JK, Bottcher-Luiz F, Andrade LL, Davidson S, Bonds L, Stephens J, Varella-Garcia M: HER-2 and cancer antigen 125 evaluation in ovarian borderline tumors by immunohistochemistry and fluorescence in situ hybridization. Int J Gynecol Cancer 2004, 14: 1078–1085. 10.1111/j.1048-891X.2004.14605.x
Hengstler JG, Lange J, Kett A, Dornhöfer N, Meinert R, Arand M, Knapstein PG, Becker R, Oesch F, Tanner B: Contribution of c-erbB-2 and topoisomerase IIa to chemoresistance in ovarian cancer. Cancer Res 1999, 59: 3206–3214.
Hogdall EV, Christensen L, Kjaer SK, Blaakaer J, Bock JE, Glud E, Nørgaard-Pedersen B, Høgdall CK: Distribution of HER-2 overexpression in ovarian carcinoma tissue and its prognostic value in patients with ovarian carcinoma: from the Danish MALOVA Ovarian Cancer Study. Cancer 2003, 98: 66–73. 10.1002/cncr.11476
Jacobs TW, Gown AM, Yaziji H, Barnes MJ, Schnitt SJ: Comparison of fluorescence in situ hybridization and immunohistochemistry for the evaluation of HER-2/neu in breast cancer. J Clin Oncol 1999, 17: 1974–1982.
Kupryjanczyk J, Madry R, Plisiecka-Halasa J, Bar J, Kraszewska E, Ziolkowska I, Timorek A, Stelmachow J, Emerich J, Jedryka M, Pluzanska A, Rzepka-Gorska I, Urbanski K, Zielinski J, Markowska J: TP53 status determines clinical significance of ERBB2 expression in ovarian cancer. Br J Cancer 2004, 91: 1916–1923. 10.1038/sj.bjc.6602238
Lakhani SR, Manek S, Penault-Llorca F, Flanagan A, Arnout L, Merrett S, McGuffog L, Steele D, Devilee P, Klijn JG, Meijers-Heijboer H, Radice P, Pilotti S, Nevanlinna H, Butzow R, Sobol H, Jacquemier J, Lyonet DS, Neuhausen SL, Weber B, Wagner T, Winqvist R, Bignon YJ, Monti F, Schmitt F, Lenoir G, Seitz S, Hamman U, Pharoah P, Lane G, Ponder B, Bishop DT, Easton DF: Pathology of ovarian cancers in BRCA1 and BRCA2 carriers. Clin Cancer Res 2004, 10: 2473–2481. 10.1158/1078-0432.CCR-1029-3
Lassus H, Leminen A, Vayrynen A, Cheng G, Gustafsson JÅ, Isola J, Butzow R: ERBB2 amplification is superior to protein expression status in predicting patient outcome in serous ovarian carcinoma. Gynecol Oncol 2004, 92: 31–39. 10.1016/j.ygyno.2003.10.010
Lee CH, Huntsman DG, Cheang MC, Parker RL, Brown L, Hoskins P, Miller D, Gilks CB: Assessment of Her-1, Her-2, And Her-3 expression and Her-2 amplification in advanced stage ovarian carcinoma. Int J Gynecol Pathol 2005, 24: 147–152. 10.1097/01.pgp.0000152026.39268.57
Nielsen JS, Jacobsen E, Holund B, Bertelsen K, Jakobsen A: Prognostic significance of p53, Her-2, and EGFR overexpression in borderline and epithelial ovarian cancer. Int J Gynecol Cancer 2004, 14: 1086–1096. 10.1111/j.1048-891X.2004.14606.x
Palacios J, Honrado E, Osorio A, Cazorla A, Sarrio D, Barroso A, Rodriguez S, Cigudosa JC, Diez O, Alonso C, Lerma E, Dopazo J, Rivas C, Benitez J: Phenotypic characterization of BRCA1 and BRCA2 tumors based in a tissue microarray study with 37 immunohistochemical markers. Breast Cancer Res Treat 2005, 90: 5–14. 10.1007/s10549-004-1536-0
Rhei E, Bogomolniy F, Federici MG, Maresco DL, Offit K, Robson ME, Saigo PE, Boyd J: Molecular genetic characterization of BRCA1- and BRCA2-linked hereditary ovarian cancers. Cancer Res 1998, 58: 3193–3196.
Riener EK, Arnold N, Kommoss F, Lauinger S, Pfisterer J: The prognostic and predictive value of immunohistochemically detected HER-2/neu overexpression in 361 patients with ovarian cancer: a multicenter study. Gynecol Oncol 2004, 95: 89–94. 10.1016/j.ygyno.2004.06.048
Rubin SC, Finstad CL, Wong GY, Almadrones L, Plante M, Lloyd KO: Prognostic significance of HER-2/neu expression in advanced epithelial ovarian cancer: a multivariate analysis. Am J Obstet Gynecol 1993, 168: 162–169.
Santin AD, Bellone S, Van Stedum S, Bushen W, De Las Casas LE, Korourian S, Tian E, Roman JJ, Burnett A, Pecorelli S: Determination of HER2/neu status in uterine serous papillary carcinoma: Comparative analysis of immunohistochemistry and fluorescence in situ hybridization. Gynecol Oncol 2005, 98: 24–30. 10.1016/j.ygyno.2005.03.041
Schorge JO, Muto MG, Lee SJ, Huang LW, Welch WR, Bell DA, Keung EZ, Berkowitz RS, Mok SC: BRCA1-related papillary serous carcinoma of the peritoneum has a unique molecular pathogenesis. Cancer Res 2000, 60: 1361–1364.
Sørlie T, Tibshirani R, Parker J, Hastie T, Marron JS, Nobel A, Deng S, Johnsen H, Pesich R, Geisler S, Demeter J, Perou CM, Lønning PE, Brown PO, Børresen-Dale AL, Botstein D: Repeated observation of breast tumor subtypes in independent gene expression data sets. Proc Natl Acad Sci USA 2003, 100: 8418–8423. 10.1073/pnas.0932692100
Tanabe H, Nishii H, Sakata A, Suzuki K, Mori Y, Shinozaki H, Watanabe A, Ochiai K, Yasuda M, Tanaka T: Overexpression of HER-2/neu is not a risk factor in ovarian clear cell adenocarcinoma. Gynecol Oncol 2004, 94: 735–739. 10.1016/j.ygyno.2004.05.055
Tanner B, Kreutz E, Weikel W, Meinert R, Oesch F, Knapstein PG, Becker R: Prognostic significance of c-erB-2 mRNA in ovarian carcinoma. Gynecol Oncol 1996, 62: 268–277. 10.1006/gyno.1996.0226
Verri E, Guglielmini P, Puntoni M, Perdelli L, Papadia A, Lorenzi P, Rubagotti A, Ragni N, Boccardo F: HER2/neu oncoprotein overexpression in epithelial ovarian cancer: evaluation of its prevalence and prognostic significance. Clinical study. Oncology 2005, 68: 154–161. 10.1159/000086958
Wu Y, Soslow RA, Marshall DS, Leitao M, Chen B: Her-2/neu expression and amplification in early stage ovarian surface epithelial neoplasms. Gynecol Oncol 2004, 95: 570–575. 10.1016/j.ygyno.2004.08.043
Acknowledgements
The study was financially supported by the State Committee for Scientific Research, Warsaw, Poland (projects No. 3P05A07024 and 3P05A02423).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Brożek, I., Kardaś, I., Ochman, K. et al. HER2 Amplification Has no Prognostic Value in Sporadic and Hereditary Ovarian Tumours. Hered Cancer Clin Pract 4, 39 (2006). https://doi.org/10.1186/1897-4287-4-1-39
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1897-4287-4-1-39