Abstract
Background
Van der Woude syndrome is the most common among syndromes which include cleft lip and/or cleft palate as one of the presentations. It is usually caused by mutations in the interferon regulatory factor 6 (IRF6) gene.
Case presentation
We previously reported on a patient with suspected deletion of the IRF6 gene. Using the Affymetrix Human SNP 6.0 Array, the interstitial deletion has been confirmed and found to be approximately 2.327–2.334 Mb within the 1q32.2 region. Although several known genes were deleted, the patient has no other phenotype apart from the orofacial presentations typical of VWS. The same deletion was not present in either parent and his two siblings were also phenotypically normal.
Conclusions
Other than IRF6, the genes which are deleted in this patient appear to be insensitive to copy number and haploinsufficiency. We compared the deletion in this patient with another case which was also mapped by high resolution array but had additional phenotypic features.
Similar content being viewed by others
Background
Cleft lip and/or cleft palate are common congenital birth defects which can occur in isolation or as part of a syndromic disorder. Among the more than 300 syndromes with orofacial clefting as one of the associated features, Van der Woude syndrome (VWS; MIM #119300) is the most common, accounting for approximately 2% of all cases. Except for the presence of paramedian lower lip pits and hypodontia, the presentation closely resembles that of isolated cleft lip and/or cleft palate. The inheritance pattern is autosomal dominant with the frequency at approximately one in 35,000 –100,000.
In 2002, the gene involved in VWS was identified as that encoding the interferon regulatory factor 6 (IRF6), a member of the interferon regulatory factor family of transcription factors [1]. The study identified 46 mutations in IRF6 in patients with VWS and another 13 in patients with popliteal pterygium syndrome (PPS; MIM 119500). The PPS phenotype includes other congenital anomalies such as webbing of the skin, bifid scrotum, syndactyly of the fingers or toes in addition to orofacial clefting.
The two different syndromic disorders are caused by mutations in the same gene but the resulting phenotype depends on the exact nucleotide or amino acid involved and the position of the mutation. The mechanism is suggested to be haploinsufficiency for VWS and dominant-negative for PPS [1]. Most of the identified mutations in VWS are nonsense and missense mutations found in exons which encode the DNA-binding or protein-binding domains. In the case of PPS, except for one nonsense mutation (Q393X), the rest involve substitutions of amino acid residues in the DNA-binding domain which makes direct contact with DNA. In vitro binding assays with the IRF6 protein showed that the 12 of the 13 mutations identified in VWS/PPS patients and mapped within the DNA-binding domain inhibited DNA binding. For mutations within the protein-binding region, six out of seven inhibited transcriptional activation completely, while the remaining one had the opposite effect [2].
Mutations in IRF6 have been identified in VWS patients from different ethnic groups. Most cases of VWS are inherited. Although penetrance is incomplete, it is still high at approximately 92%. Sequence analysis of the IRF6 coding region (exons 1–9) can detect mutations in 70% of patients with the VWS phenotype, of which 80% of the mutations would be within the protein-coding exons 3–9. In less than 2% of individuals with VWS, the entire IRF6 gene is deleted [3].
We previously described a case of de novo deletion as observed by the loss of paternal alleles and complete homozygosity of IRF6 gene polymorphisms. The reduced gene dosage was confirmed by MLPA [4]. In this paper, we described the mapping of the deletion in this patient using a high resolution single nucleotide polymorphism (SNP) array.
Case presentation
The patient is the eldest of three children of healthy unrelated parents of Chinese ancestry. There was no significant family history of cleft lip and palate. He was previously found to have features consistent with Van der Woude Syndrome due to the presence of cleft lip and palate and lower lip pits.
DNA was extracted from frozen whole blood samples using the Gentra Puregene Blood Kit (Gentra Systems Inc., Minneapolis, USA). It was checked for quantity and purity using the NanoDrop Spectrophotometer (NanoDrop Technologies, Wilmington, USA). Genome-wide Human SNP 6.0 Array (Affymetrix Inc., Santa Clara, USA) containing more than 906,600 SNPs and more than 946,600 copy number probes was used. Labeling, hybridization, washing, scanning and image extraction were performed by an Affymetrix certified service laboratory according to manufacturer’s instructions. Data was analyzed using Chromosome Analysis Suite.
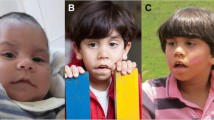
Based on the analysis results for all chromosomes, there was a copy number loss in 1q32 from at least position 205,941,798 to position 208,274,440 (NCBI36/hg18 or 207,875,175−210,207,817 for GR37/hg19). The size is at least 2,332 kb involving 1,894 markers (1,113 SNP and 781 CNV markers) (Figure 1A). The last SNP with normal copy number is rs1830762 (genotype called as “GA”) at position 205,940,895. The first SNP with altered copy number is rs4844614 (genotype called as “GG”) at position 205,942,060. The last SNP with altered copy number is rs227193 (genotype called as “AA”) at position 208,279,047. The first SNP with normal copy number is rs12561877 (genotype called as “CT”) at position 208,282,037. The proximal breakpoint is within Variation_3328, while the distal breakpoint is between varation_34766 and variation_9388 and within intron 4 of the synaptotagmin 14 (SYT14) trafficking gene. Both parental samples were also tested in the same experiment on different arrays. There was no similar deletion in either parent (Figures 1B and C).
Information obtained from the online databases showed that nine annotated genes (including IRF6) were completely deleted and two more were partially deleted. There were several more hypothetical genes and microRNAs (Table 1). Besides the identified genes, there are other sequences with open reading frames and hypothetical proteins within the deleted region such as LOC729533 (FAM72A), LOC440712 (C1 orf186), HCA56, C1orf116, pfkfb2, YOD1, AXX229788, EU154352, LOC148696, AK123177, KIAA0463, LOC642587, DM004461, LOC148304 (C1 orf74) and C1 orf107.
Discussion
The VWS locus was first mapped to the chromosomal region 1q32-41 [7] before mutations in the IRF6 gene were identified in patients with VWS and PPS [1]. Although SNPs in the gene have been associated with non-syndromic cleft lip and/or cleft palate [8], no other syndrome has been linked to the gene. While most identified mutations in VWS families were single nucleotide substitutions, there are a few cases of deletions. Most of the latter were small within-gene deletions which ranged from 5 to18 bp [1]. There was one report of a 17-kb deletion involving exons 4–9 in a Japanese family [9].
There is no recognized microdeletion syndrome for this chromosomal region, indicating that pathogenic genomic imbalance in this region is rare. For larger deletions which include additional genes outside of the IRF6 genomic region, there are only four previous reports (Table 2): a Mexican girl with cytogenetically visible deletion from 1q32-41 [10], submicroscopic deletions in two families VWS1473 and VWS771 [7, 11], and a Malay girl whose deletion was mapped by oligonucleotide-based comparative genomic hybridization (CGH) [12]. The patient in this report will be only the fifth case in the series (Table 2). A CGH study using BAC arrays detected microdeletions involving 1q32.2 in five cases (including VWS1473 and VWS771) but no information was provided on the size and breakpoints for each case [13].
In the present case, the breakpoint for the proximal end of the deletion is within a segment known as variation_3328 which is a copy number polymorphism (CNV). The distal breakpoint is within a large intron of the STY14 gene. Some of the genes in the deleted region are associated with conditions listed in Online Mendelian Inheritance in Men (OMIM). They are CR1L with SLE susceptibility, CD46 with measles, LAMB3 with epidermolysis bullosa (OMIM #226650 and 226700), and HSD11B1 with cortisone reductase deficiency. However, this patient has no other clinically significant pathology. There is no psychomotor delay or intellectual disability commonly found in patients with microdeletions involving multiple genes, therefore it appears that the other deleted genes are not sensitive to copy number changes. Indeed this is consistent with the scores for Hapoinsufficiency Index (HI) according to the DECIPHER database [6]. The IRF6 gene which has the most significant HI index is also the only gene which could be linked to the patient’s phenotype.
For the four previously reported VWS families/cases with deletions, the extent of the deletion in the case with microscopic deletion is unknown (Case 1 in Table 2). The other three deletions have been mapped by molecular methods. The distal breakpoint in VWS1473 and VWS771 (Case 2 and Case 3 in Table 2) appeared to be within the SYT14 gene, similar to that found in the present case (Figure 2). However, the proximal breakpoint is different for the three cases, with the present case having the largest deletion extending beyond D1S245 at the proximal end of the chromosome. This marker was not deleted in the other two families VWS1473 and VWS771. The deletion in the 22-month-old Malay girl (Case 4 in Table 2) did not share similar breakpoints at either end with any of the documented cases. The deletion started at a more telomeric position and extended further towards the telomere. Interestingly, it was also a de novo occurrence on the paternal chromosome as in the present case [4, 12]. For family VWS1473, the deletion was on the maternally derived chromosome as the maternal allele was missing for D1S3753 [7].
Developmental delay and dysmorphism was reported for Case 1. Family VWS 1473 (Case 2) involved affected members over three generations [11]. This is the only family with developmental and psychomotor delay out of over 300 VWS families studied. Along with cleft lip/palate and lip pits, all affected relatives exhibited various forms of developmental delay. There is one other report of a child with VWS features and also presenting with mental retardation but there was no karyotype information [14]. Segregation of the VWS phenotype with intellectual disability in these three instances suggests that there is a gene involved in cognitive development in the region, and it is due to a dominant mutation and not haploinsufficiency. The 2.3 Mb microdeletion in our patient is bigger than that found in VWS1473 (Case 2 in Table 2) but he has normal intelligence. He has been followed up closely for the last 20 years and there is no evidence of other clinically significant condition. The loss of so many genes with no additional phenotypic consequence other than VWS at birth is surprising but is consistent with studies showing that the other genes deleted are unlikely to be haploinsufficient.
The largest deletion reported thus far is 2.98 Mb (Case 4 in Table 2) detected using an Agilent 400 K CGH array [12]. At the time of the report, the 22-month old child was meeting developmental milestones with no evidence of developmental delay. There were dysmorphic features (including syndactyly also seen in PPS) and some indication of growth retardation. This deletion is distinct from others in that both proximal and distal breakpoints are different from previously reported cases. The only deleted genes shared are CAMK1G, G0S2, TRAF31P3, and IRF6. The distal end extends much further and includes at least 10 more genes, three of which had Haploinsufficiency Index (HI index) of less than 10, indicating that they are dosage sensitive and expected to have phenotypic effect (Table 1). However, none of the three genes have been linked to the dysmorphic features observed in this patient. Interestingly, the Development Disorder Genotype-Phenotype Database (DDG2P) lists IRF6 as one of the genes associated with developmental disorders [15]. It is the only gene within the deleted which is listed as having evidence of developmental delay in multiple cases. However, there is no evidence of developmental delay for both our patient and the patient with the 2.98 Mb deletion.
Conclusions
The deletion in our patient appeared to be a very rare event with only two other de novo cases reported. Our data suggest that other than IRF6, the genes that were deleted were not affected by haploinsufficiency.
Consent
Approval to conduct the study was granted by the SingHealth Institutional Review Board. Written informed consent was obtained from the patients’ parents.
Authors’ information
1Principal Scientist (ECT) and Senior Medical Technologist (ECPL), KK Research Centre, KK Women’s and Children’s Hospital, 100 Bukit Timah Road, Singapore 229899. 2Adjunct Associate Professor, Office of Clinical Sciences, Duke-NUS Graduate Medical School Singapore, 8 College Road, Singapore 169857. 3Emeritus Consultant, Department of Plastic, Reconstructive & Aesthetic Surgery, Singapore General Hospital, Outram Road, Singapore 169608.
Abbreviations
- BAC:
-
Bacterial artificial chromosome
- Bp:
-
Basepairs
- CNV:
-
Copy number variant
- HI:
-
Haploinsufficiency
- Mb:
-
Million basepairs
- MIM:
-
Mendelian inheritance in Men
- PPS:
-
Popliteal pterygium syndrome
- SNP:
-
Single nucleotide polymorphism
- VWS:
-
Van der Woude syndrome.
References
Kondo S, Schutte BC, Richardson RJ, Bjork BC, Knight AS, Watanabe Y, Howard E, de Lima RL, Daack-Hirsch S, Sander A, et al.: Mutations in IRF6 cause Van der Woude and popliteal pterygium syndromes. Nat Genet 2002, 32: 285–289. 10.1038/ng985
Little HJ, Rorick NK, Su LI, Baldock C, Malhotra S, Jowitt T, Gakhar L, Subramanian R, Schutte BC, Dixon MJ, Shore P: Missense mutations that cause Van der Woude syndrome and popliteal pterygium syndrome affect the DNA-binding and transcriptional activation functions of IRF6. Hum Mol Genet 2009, 18: 535–545.
IRF6-Related disorders. http://www.ncbi.nlm.nih.gov/books/NBK1407/
Tan EC, Lim EC, Yap SH, Lee ST, Cheng J, Por YC, Yeow V: Identification of IRF6 gene variants in three families with Van der Woude syndrome. Int J Mol Med 2008, 21: 747–751.
UCSC genome browser. http://genome.ucsc.edu/cgi-bin/hgGateway
DECIPHER. https://decipher.sanger.ac.uk
Schutte BC, Basart AM, Watanabe Y, Laffin JJ, Coppage K, Bjork BC, Daack-Hirsch S, Patil S, Dixon MJ, Murray JC: Microdeletions at chromosome bands 1q32-q41 as a cause of Van der Woude syndrome. Am J Med Genet 1999, 84: 145–150. 10.1002/(SICI)1096-8628(19990521)84:2<145::AID-AJMG11>3.0.CO;2-L
Zucchero TM, Cooper ME, Maher BS, Daack-Hirsch S, Nepomuceno B, Ribeiro L, Caprau D, Christensen K, Suzuki Y, Machida J, et al.: Interferon regulatory factor 6 (IRF6) gene variants and the risk of isolated cleft lip or palate. N Engl J Med 2004, 351: 769–780. 10.1056/NEJMoa032909
Kayano S, Kure S, Suzuki Y, Kanno K, Aoki Y, Kondo S, Schutte BC, Murray JC, Yamada A, Matsubara Y: Novel IRF6 mutations in Japanese patients with Van der Woude syndrome: two missense mutations (R45Q and P396S) and a 17-kb deletion. J Hum Genet 2003, 48: 622–628. 10.1007/s10038-003-0089-0
Bocian M, Walker AP: Lip pits and deletion 1q32–41. Am J Med Genet 1987, 26: 437–443. 10.1002/ajmg.1320260223
Sander A, Schmelzle R, Murray J: Evidence for a microdeletion in 1q32–41 involving the gene responsible for Van der Woude syndrome. Hum Mol Genet 1994, 3: 575–578. 10.1093/hmg/3.4.575
Salahshourifar I, Halim AS, Sulaiman WA, Ariffin R, Naili Muhamad Nor N, Zilfalil BA: De novo interstitial deletion of 1q32.2-q32.3 including the entire IRF6 gene in a patient with oral cleft and other dysmorphic features. Cytogenet Genome Res 2011, 134: 83–87. 10.1159/000325541
Osoegawa K, Vessere GM, Utami KH, Mansilla MA, Johnson MK, Riley BM, L'Heureux J, Pfundt R, Staaf J, van der Vliet WA, et al.: Identification of novel candidate genes associated with cleft lip and palate using array comparative genomic hybridisation. J Med Genet 2008, 45: 81–86.
Ugwu BT, Momoh JT: Van der Woude syndrome with mental retardation: case report. East Afr Med J 2001, 78: 111–112.
Developmental disorders genotype-phenotype database. https://decipher.sanger.ac.uk/ddd/ddd_genes
Acknowledgements
We are grateful to the patient and his parents for participating in this study. This work was supported by project grant KRAU151/09 from KK Women’s and Children’s Hospital and NMRC/PPG/KKH12010-Theme3 from the National Medical Research Council, Ministry of Health, Republic of Singapore.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare no competing interests.
Authors’ contributions
ECT planned the study, obtained the funding, did the analysis and drafted the manuscript. ECPL assisted in the analysis and preparation of the figures. STL did the clinical characterization and helped to draft the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Tan, EC., Lim, E.C. & Lee, ST. De novo 2.3 Mb microdeletion of 1q32.2 involving the Van der Woude Syndrome locus. Mol Cytogenet 6, 31 (2013). https://doi.org/10.1186/1755-8166-6-31
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1755-8166-6-31