Abstract
Introduction
An internal hernia is a protrusion of bowel through a normal or abnormal orifice in the peritoneum or mesentery. Although they are considered as a rare cause of intestinal obstruction, paraduodenal hernias are the most common type of congenital hernias.
Methods
A literature search using PubMed was performed to identify all published cases of left paraduodenal hernia (LPDH).
Results
In Literature search between 1980 and 2012 using PubMed revealed only 44 case reports before the present one. Median age was 47 years (range 18 – 82 years). Nearly 50% reported previous mild symptoms. Two-third of patients required emergency surgery in form of laparotomy or laparoscopic repair. Reduction of hernia contents with widening or suture repair of the hernia orifice were the most common standards in surgical management of LPDH.
Conclusion
Intestinal obstruction secondary to internal hernias is a rare presentation. High index of suspicion and preoperative imaging are essential to make an early diagnosis in order to improve outcome.
Similar content being viewed by others
Introduction
Internal hernia is, either congenital or acquired, a rare cause of small-bowel obstruction, with a reported incidence of less than 2%[1]. Paraduodenal hernias, which are a type of internal hernia, occur due to malrotation of midgut and form a potential space near the ligament of Treitz[2]. Incidental finding at laparotomy or on imaging is the most common presentation of these hernias[3]. Nevertheless, Paraduodenal hernias can lead to bowel obstruction, ischemia, and perforation with a high mortality. Left paraduodenal hernia (LPDH) is the most common types of congenital hernias and accounts for more than 40% of all cases[4]. Clinical diagnosis of LPDH is a real challenge as symptoms are entirely nonspecific. Therefore, a timely and correct diagnosis with a rapid diagnostic tool is mandatory[5]. In this review we discuss the clinical presentation and management of small bowel obstruction secondary to LPDH.
Case presentation
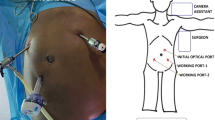
A 47 –year-old Caucasian male admitted with increasing severe colicky abdominal pain and bile stained vomiting of 2 days duration. He had no previous significant past medical or surgical history. He also denied any history of weight loss, or recent changes in his bowel habit. However, He described at least 4 previous episodes of upper abdominal distension and vomiting with spontaneous resolution over the previous 2 years. On examination, the patient appeared in moderate pain with normal vital signs. Abdominal examination revealed abdominal distension with a tender mass in the left upper quadrant. Laboratory studies were essentially normal. An urgent abdominal CT scan confirmed the diagnosis of small bowel obstruction secondary to what looked like a hernia into the left paraduodenal fossa (fossa of Landzert) (Figure 1). At laparotomy, a hernia sac of 25 cm in diameter arising from a defect just to the left of the fourth part of the duodenum was found, consistent with a LPDH (Figure 2A). The intestinal loops were herniated through that congenital defect and were not spontaneously reducible. A band containing the inferior mesenteric vein was deemed necessary to divide at the time in order to widen the orifice of the defect and to retrieve the dilated small bowel from the hernia sac (Figure 2B). The hernia sac was excised completely down to the base at the mesentery of large bowel (Figure 2C). The patient had uneventful postoperative recovery and discharged home 5 days later. At 8 weeks post-surgery, he was back to full normal activities with a well-healed laparotomy scar.
Discussion
Internal herniation of the small bowel is a relatively rare cause of intestinal obstruction and accounts for less than 2% of all causes[1]. Among all congenital hernias, paraduodenal hernias are the most common type with an overall incidence of approximately 50% of all internal hernias[1, 4, 6]. LPDH (hernia of Lanzert) is about three times more common than the right counterpart (Waldayer’s hernia)[7]. LPDH arises from the fossa of Landzert, a congenital defect which presents in approximately 2% of the population, located to the left of the fourth part of the duodenum, posterior to the inferior mesenteric vein and left branches of the middle colic artery (Figure 2A)[2, 8, 9]. Small bowel loops (usually jujenum) prolapse posteroinferiorly through the fossa to the left of the fourth part of the duodenum into the left portion of the transverse mesocolon. Hence, the herniated small bowel loops may become trapped within this mesenteric sac (Figure 2C)[4, 10].
Literature search between 1980 and 2012 using PubMed revealed only 44 case reports before the present one[2, 5, 11–49] (Table 1). Median age at presentation was 47 (range of 18–82 years old) with male to female ratio of 3:1. In this review, patients often presented with symptoms and signs of typical of internal hernias complicated by bowel obstruction, strangulation, and/or necrosis. Besides, 43% of patients reported a prior history of recurring abdominal pain with symptoms. Only three cases presented with a palpable mass in the left upper quadrant at time of presentation.
Radiological diagnosis of LPDH prior to surgery was achieved in 43% of patients. On CT scan, typical appearance of LPDH is an encapsulated sac containing clusters of dilated small bowel loops at or above the ligament of Treitz with a mass like effect compressing the posterior gastric wall and distal part of the duodenum. Besides, there is engorgement and crowding of the mesenteric vessels with frequent right displacement of the main mesenteric trunk and depression of the transverse colon (Figure 1).
Once a LPDH is identified, operative treatment is necessary, as patients with a LPDH have a 50% lifetime risk of developing small bowel obstruction with a 20–50% mortality rate for acute presentations[6, 8]. In this review, 28 patients (67%) underwent emergency surgery. Of those 43 patients, 15 patients had laparoscopic repair of LPDH. Surgical intervention included reduction of the herniated small bowel loops and closure of the hernia orifice with non-absorbable sutures or a mesh[5, 24]. A different possibility was to widen the hernia orifice to prevent future incarceration of bowel loops[5]. Often, there is a close anatomical relationship between the inferior mesenteric vein which bound the hernia anteriorly, and the hernia orifice[5, 24]. Therefore, division of the inferior mesenteric vessels at the neck of the sac may be necessary, as in this case, when the incarcerated bowel could not be reduced easily from the hernia[24].
Conclusion
Left paraduodenal fossa hernia is a relatively a rare cause of small bowel obstruction. In young patients with recurrent small bowel obstruction with no previous surgical history, it is crucial to consider internal hernias in the differential diagnosis. Furthermore, a timely and correct diagnosis is together with prompt surgical intervention is essential for achieving patient’s cure and prevents future complications.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
Blachar A, Federle MP, Dodson SF: Internal hernia: clinical and imaging findings in 17 patients with emphasis on CT criteria. Radiology. 2001, 218 (1): 68-74.
Berardi RS: Paraduodenal hernias. Surg Gynecol Obstet. 1981, 152 (1): 99-110.
Olazabal A, Guasch I, Casas D: Case report: CT diagnosis of nonobstructive left paraduodenal hernia. Clin Radiol. 1992, 46 (4): 288-289. 10.1016/S0009-9260(05)80175-8.
Martin LC, Merkle EM, Thompson WM: Review of internal hernias: radiographic and clinical findings. AJR Am J Roentgenol. 2006, 186 (3): 703-717. 10.2214/AJR.05.0644.
Khalaileh A: Left laparoscopic paraduodenal hernia repair. Surg Endosc. 2010, 24 (6): 1486-1489. 10.1007/s00464-009-0794-7.
Blachar A: Radiologist performance in the diagnosis of internal hernia by using specific CT findings with emphasis on transmesenteric hernia. Radiology. 2001, 221 (2): 422-428. 10.1148/radiol.2212010126.
Khan MA, Lo AY, Vande Maele DM: Paraduodenal hernia. Am Surg. 1998, 64 (12): 1218-1222.
Zonca P: Treitz's hernia. Hernia. 2008, 12 (5): 531-534. 10.1007/s10029-008-0339-3.
Willwerth BM, Zollinger RM, Izant RJ: Congenital mesocolic (paraduodenal) hernia. Embryologic basis of repair. Am J Surg. 1974, 128 (3): 358-361. 10.1016/0002-9610(74)90173-1.
Armstrong O: Internal hernias: anatomical basis and clinical relevance. Surg Radiol Anat. 2007, 29 (4): 333-337. 10.1007/s00276-007-0212-6.
Chatterjee S, Kumar S, Gupta S: Acute intestinal obstruction: a rare aetiology. Case Rep Surg. 2012, 2012: 501209-
Hafeez Bhatti AB, Khan MA: Left paraduodenal hernia: a rare cause of large bowel obstruction and gangrene. J Coll Physicians Surg Pak. 2012, 22 (4): 250-251.
Akbulut S: Unusual cause of intestinal obstruction: left paraduodenal hernia. Case Report Med. 2012, 2012: 529246-
Hussein M: Laparoscopic repair of a left paraduodenal hernia presenting with acute bowel obstruction: report of a case. Surg Laparosc Endosc Percutan Tech. 2012, 22 (1): e28-e30. 10.1097/SLE.0b013e31823f3798.
Fernandez-Rey CL, Martinez-Alvarez C, Concejo-Cutoli P: Acute abdomen secondary to left paraduodenal hernia: diagnostic by multislice computer tomography. Rev Esp Enferm Dig. 2011, 103 (1): 38-39.
Downes R, Cawich SO: A case of a paraduodenal hernia. Int J Surg Case Rep. 2010, 1 (2): 19-21. 10.1016/j.ijscr.2010.06.003.
Parmar BP, Parmar RS: Laparoscopic management of left paraduodenal hernia. J Minim Access Surg. 2010, 6 (4): 122-124. 10.4103/0972-9941.72601.
Yun MY: Left paraduodenal hernia presenting with atypical symptoms. Yonsei Med J. 51 (5): 787-789.
Uchiyama S: An unusual variant of a left paraduodenal hernia diagnosed and treated by laparoscopic surgery: report of a case. Surg Today. 2009, 39 (6): 533-535. 10.1007/s00595-008-3875-7.
Poultsides GA: Image of the month. Left paraduodenal hernia. Arch Surg. 2009, 144 (3): 287-288.
Kuzinkovas V: Paraduodenal hernia: a rare cause of abdominal pain. Can J Surg. 2008, 51 (6): E127-E128.
Peters SA: Radiology for the surgeon: Soft-tissue case 60. Can J Surg. 2008, 51 (2): 151-152.
Jeong GA: Laparoscopic repair of paraduodenal hernia: comparison with conventional open repair. Surg Laparosc Endosc Percutan Tech. 2008, 18 (6): 611-615. 10.1097/SLE.0b013e3181825733.
Palanivelu C: Laparoscopic management of paraduodenal hernias: mesh and mesh-less repairs. A report of four cases. Hernia. 2008, 12 (6): 649-653. 10.1007/s10029-008-0376-y.
Shoji T: Left paraduodenal hernia successfully treated with laparoscopic surgery: a case report. Case Rep Gastroenterol. 2007, 1 (1): 71-76. 10.1159/000107595.
Papaziogas B: Idiopathic hypertrophic pyloric stenosis combined with left paraduodenal hernia in an adult. Med Princ Pract. 2007, 16 (2): 151-154. 10.1159/000098370.
Moon CH, Chung MH, Lin KM: Diagnostic laparoscopy and laparoscopic repair of a left paraduodenal hernia can shorten hospital stay. JSLS. 2006, 10 (1): 90-93.
Brehm V, Smithuis R, Doornebosch PG: A left paraduodenal hernia causing acute bowel obstruction: a case report. Acta Chir Belg. 2006, 106 (4): 436-437.
Thoma M: Left paraduodenal hernia: a case report. Acta Chir Belg. 2006, 106 (4): 433-435.
Cingi A: Left-sided paraduodenal hernia: report of a case. Surg Today. 2006, 36 (7): 651-654. 10.1007/s00595-006-3205-x.
Kurachi K: Left paraduodenal hernia in an adult complicated by ascending colon cancer: a case report. World J Gastroenterol. 2006, 12 (11): 1795-1797.
Huang YM: Left paraduodenal hernia presenting as recurrent small bowel obstruction. World J Gastroenterol. 2005, 11 (41): 6557-6559.
Ovali GY: Transient left paraduodenal hernia. Comput Med Imaging Graph. 2005, 29 (6): 459-461. 10.1016/j.compmedimag.2004.09.019.
Fukunaga M: Laparoscopic surgery for left paraduodenal hernia. J Laparoendosc Adv Surg Tech A. 2004, 14 (2): 111-115. 10.1089/109264204322973907.
Rollins MD, Glasgow RE: Left paraduodenal hernia. J Am Coll Surg. 2004, 198 (3): 492-493. 10.1016/j.jamcollsurg.2003.07.025.
Patti R: Paraduodenal hernia: an uncommon cause of recurrent abdominal pain. G Chir. 2004, 25 (5): 183-186.
Catalano OA: Internal hernia with volvulus and intussusception: case report. Abdom Imaging. 2004, 29 (2): 164-165. 10.1007/s00261-003-0122-y.
Goodney PP, Pindyck F: Paraduodenal hernia and jejunal diverticulosis. J Gastroenterol Hepatol. 2004, 19 (2): 229-231. 10.1111/j.1440-1746.2004.02859.x.
Tong RS, Sengupta S, Tjandra JJ: Left paraduodenal hernia: case report and review of the literature. ANZ J Surg. 2002, 72 (1): 69-71. 10.1046/j.1445-2197.2002.02300.x.
Nishida T: Unusual type of left paraduodenal hernia caused by a separated peritoneal membrane. J Gastroenterol. 2002, 37 (9): 742-744. 10.1007/s005350200121.
Patil R, Smith C, Brown MD: Paraduodenal hernia presenting as unexplained recurrent abdominal pain. Am J Gastroenterol. 1999, 94 (12): 3614-3615. 10.1111/j.1572-0241.1999.01617.x.
Schaffler GJ: Anterior and upward displacement of the inferior mesenteric vein:a new diagnostic clue to left paraduodenal hernias?. Abdom Imaging. 1999, 24 (1): 29-31. 10.1007/s002619900435.
Uematsu T: Laparoscopic repair of a paraduodenal hernia. Surg Endosc. 1998, 12 (1): 50-52. 10.1007/s004649900591.
Hirasaki S: Unusual variant of left paraduodenal hernia herniated into the mesocolic fossa leading to jejunal strangulation. J Gastroenterol. 1998, 33 (5): 734-738. 10.1007/s005350050164.
McDonagh T, Jelinek GA: Two cases of paraduodenal hernia, a rare internal hernia. J Accid Emerg Med. 1996, 13 (1): 64-68. 10.1136/emj.13.1.64.
Suchato C, Pekanan P, Panjapiyakul C: CT findings in symptomatic left paraduodenal hernia. Abdom Imaging. 1996, 21 (2): 148-149. 10.1007/s002619900031.
Warshauer DM, Mauro MA: CT diagnosis of paraduodenal hernia. Gastrointest Radiol. 1992, 17 (1): 13-15. 10.1007/BF01888498.
Du Toit DF, Pretorius CF: Left paraduodenal hernia with acute abdominal symptoms. A case report. S Afr Med J. 1986, 70 (4): 233-234.
Tireli M: Left paraduodenal hernia. Br J Surg. 1982, 69 (2): 114-10.1002/bjs.1800690219.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
WAK, SA, JB, and TER prepared the manuscript. TER outlined the manuscript’s layout and supervised the work. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
This article is published under license to BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Al-Khyatt, W., Aggarwal, S., Birchall, J. et al. Acute intestinal obstruction secondary to left paraduodenal hernia: a case report and literature review. World J Emerg Surg 8, 5 (2013). https://doi.org/10.1186/1749-7922-8-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1749-7922-8-5