Abstract
Background
Meta-analysis of randomized trials has shown that postoperative radiotherapy (PORT) had a detrimental effect on overall survival (OS) in patients with resected N1 non–small cell lung cancer (NSCLC). Conversely, the locoregional recurrence (LR) rate is reported to be high without adjuvant PORT in these patients. We have evaluated the pattern of failure, actuarial risk and risk factors for LR in order to identify the subset of N1 NSCLC patients with the highest risk of LR. These patients could potentially benefit from PORT.
Methods
We conducted a retrospective study on 199 patients with pathologically confirmed T1–3N1M0 NSCLC who underwent surgery. None of the patients had positive surgical margins or received preoperative therapy or PORT. The median follow-up was 53.8 months. Complete mediastinal lymph node (MLN) dissection and examination was defined as ≥3 dissected and examined MLN stations; incomplete MLN dissection or examination (IMD) was defined as <3 dissected or examined MLN stations. The primary end point of this study was freedom from LR (FFLR). Differences between patient groups were compared and risk factors for LR were identified by univariate and multivariate analyses.
Results
LR was identified in 41 (20.6%) patients, distant metastasis (DM) was identified in 79 (39.7%) patients and concurrent LR and DM was identified in 25 (12.6%) patients. The 3- and 5-year OS rates in patients with resected N1 NSCLC were 78.4% and 65.6%, respectively. The corresponding FFLR rates were 80.8% and 77.3%, respectively. Univariate analyses identified that nonsmokers, ≤23 dissected lymph nodes, visceral pleural invasion and lymph node ratio >10% were significantly associated with lower FFLR rates (P < 0.05). Multivariate analyses further confirmed positive lymph nodes at station 10 and IMD as risk factors for LR (P < 0.05). The 5-year LR rate was highest in patients with both these risk factors (48%).
Conclusions
The incidence of LR in patients with surgically resected T1–3N1M0 NSCLC is high. Patients with IMD and positive lymph nodes at station 10 have the highest risk of LR, and may therefore benefit from adjuvant PORT. Further investigations of PORT in this subset of patients are warranted.
Similar content being viewed by others
Background
Surgery is the cornerstone of treatment for early-stage non–small cell lung cancer (NSCLC). Due to high recurrence rates following tumor resection, including radical surgery, studies have been carried out on the efficacy of adjuvant therapy. Several randomized trials and meta-analyses have confirmed that platinum-based adjuvant chemotherapy can improve overall survival (OS) in patients with stage II and IIIA NSCLC[1–4]; however, the role of postoperative radiotherapy (PORT) remains controversial. Although studies have found that PORT can reduce locoregional recurrence (LR), no survival benefit was observed. Moreover, meta-analyses of randomized trials and retrospective studies have reported that PORT had a detrimental effect on OS in patients with N0 and N1 NSCLC, despite being beneficial in patients with N2 disease[5–8]. As a consequence, PORT is often recommended for patients with resected pathological N2 disease, but not for those with N0 or N1 disease. However, these studies may have been compromised by limitations such as flaws in the study design and outdated radiation techniques.
The reported crude risk of LR for resected N1 disease is high[9–11], which suggests that a subset of N1 patients with high risk of LR may benefit from further local treatment after surgery. The purpose of the present study was to assess the clinical and pathological risk factors that influence LR in patients with resected N1 NSCLC in order to identify and select those patients at high risk of LR for further studies on PORT.
Methods
Study population
This retrospective medical record review study was approved by our institutional review board. The inclusion criteria were as follows: (1) pathologically confirmed T1–3N1M0 NSCLC, (2) consecutive treatment between January 2007 and December 2008 in our hospital, (3) anatomical pulmonary resection with lobecotomy, sleeve lobectomy, bilobecotomy or pneumonectomy and (4) complete records of clinical and pathological data. The exclusion criteria were as follows: (1) positive surgical margins, (2) prior neoadjuvant therapy involving chemotherapy, radiotherapy or PORT, (3) synchronous primary lung tumors or a history of lung cancer and (4) perioperative death. Patients were staged according to the 7th edition of the American Joint Committee on Cancer (AJCC) tumor-node-metastasis (TNM) classification system[12].
Definition of recurrence
The primary end point of this study was freedom from LR (FFLR). Local recurrence was defined as the recurrence of a tumor at the bronchial stump or anastomosis, and regional recurrence was defined as recurrence in the mediastinum, hilum or supraclavicular fossa. Other sites of recurrence, including contralateral lung and metastatic lymph nodes in the neck or axilla were defined as distant metastasis (DM). Concurrent recurrence was defined as LR and DM being detected within 30 days of each other; otherwise, it was considered sequential recurrence.
The diagnosis of disease recurrence and recurrence sites was based on a review of the medical records, including operative notes, follow-up imaging reports and cytological and pathological reports. All local recurrences were confirmed by sputum cytology or bronchoscopic biopsy. Nodal recurrences were confirmed by biopsy using ultrasound-guided fine-needle aspiration (FNA) or endobronchial ultrasound-guided transbronchial needle aspiration (EBUS-TBNA). New or enlarging lymph nodes (≥1 cm short axis) were confirmed by computed tomography (CT) or through hypermetabolism on positron-emission tomography (PET)-CT, which was found to be consistent with disease progression during subsequent clinical follow-ups. Sites of recurrent lymph nodes were identified using the lymph node map proposed by the International Association for the Study of Lung Cancer (IASLC)[13].
Follow-up
The median follow-up time was 53.8 months (range, 1.4–81.8 months). Physical examination, chest x-rays and/or CT scans and abdominal ultrasonography were performed every 3 months for the first 2 years following adjuvant chemotherapy, then every 6 months for 5 years and every year thereafter. PET-CT was performed if recurrent disease could not be identified or suspected by routine CT. Other tests were carried out at the discretion of the treating physician.
Of the 199 patients that were eligible for this study, 158 (79.4%) had received adjuvant platinum-based chemotherapy after surgery.
OS was measured from the date of surgery to the date of death from any cause; disease-free survival (DFS) was measured from the date of surgery to the date of LR, DM or death from any cause; FFLR was measured from the date of surgery to the date of identification of LR; freedom from DM (FFDM) was measured from the date of surgery to the date of identification of DM.
Statistical analysis
The Kaplan-Meier method was used to estimate OS, DFS, FFLR and FFDM. Differences between groups were calculated using the log-rank test. Receiver operating characteristic (ROC) curves were constructed, and the Youden Index was used to determine the optimal cut-off points for part of continuous variables, suh as number of dissected lymph nodes and lymph node ratio. Univariate and multivariate Cox regression analyses were performed to assess risk factors associated with LR. A P-value <0.05 was considered statistically significant.
Results
Patient characteristics
Patient characteristics and treatments are given in Table 1. The median number of dissected lymph nodes was 21 (range, 3–66). The median number of metastatic lymph nodes was 2 (range, 1–8). The number of dissected mediastinal lymph node (MLN) stations was evaluated from both surgical records and pathological reports; however, some of the results were inconsistent: 78 patients had <3 MLNs recorded in both reports; 86 patients had ≥3 MLNs recorded in both reports; and 35 patients had ≥2 dissected MLN stations recorded in their surgical records but <3 in their pathological reports.
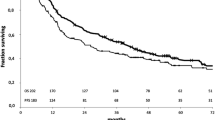
The 3- and 5-year OS rates were 78.4% and 65.6%, respectively, and the corresponding DFS rates were 55.3% and 45.7%, respectively (Figure 1). The 3-year and 5-year FFLR and FFDM rates were 80.8% and 77.3%, respectively and 65.9% and 57.4%, respectively (Figure 2). Tumor recurrence occurred in 95 patients (47.7%) by the last follow-up.
LR and DM were identified in 41 patients (20.6%) and 79 patients (39.7%), respectively (Figure 3). Concurrent LR and DM were identified in 25 patients (12.6%). Lung and pleura were the most common sites of DM (40 patients and 11 patients, respectively). Other DM sites were the brain (24 patients, 12.1%), bone (25 patients, 12.6%), liver (9 patients, 4.5%) and adrenal gland (4 patients, 2.0%).
Risk factors for LR
We evaluated patients’ clinical and pathological characteristics by univariate and multivariate analyses to identify factors that might be associated with FFLR (Table 1). The optimal cut-off points for the number of dissected lymph nodes and lymph node ratio (LNR) in relation to LR were determined by constructing ROC curves and calculating the maximal Youden index. Complete MLN dissection and examination (CMD) and incomplete MLN dissection or examination (IMD) were defined according to the number of MLN stations recorded in the surgical records and pathological reports. CMD was defined as ≥3 MLNs in both reports with a 5-year FFLR of 89%; IMD was defined as either <3 MLNs in both reports with a 5-year FFLR of 68.6% or as ≥3 MLNs in the surgical records and <3 MLNs in the pathological reports with a 5-year FFLR of 68%.
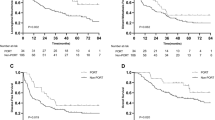
Univariate analyses identified the following factors as being associated with a lower FFLR rate: nonsmokers (P = 0.026), ≤23 dissected lymph nodes (P = 0.007), visceral pleural invasion (P = 0.025), LNR >10% (P = 0.027); positive lymph nodes at station 10 (P = 0.01; Figure 4) and IMD (P = 0.001; Figure 5). Other risk factors that showed a trend of lower FFLR included lymphovascular invasion (P = 0.088) and negative bronchoscopy findings (P = 0.08).
Comparison between patients with positive and negative lymph nodes at station 10. The difference in freedom from locoregional recurrence (FFLR) rates between patients with resected N1 non–small cell lung cancer and positive or negative lymph nodes (LNs) at station 10 is significant (P = 0.01), showing that a positive LN at station 10 is a risk factor for LR.
Comparison between patients with incomplete and complete mediastinal lymph node dissection and examination. The difference in freedom from locoregional recurrence (FFLR) rates between patients with complete mediastinal lymph node (MLN) dissection and examination (CMD) and incomplete MLN dissection or examination (IMD) is significant (P = 0.01), and shows that IMD is a greater risk factor for LR than positive lymph nodes at station 10 in patients with resected N1 non–small cell lung cancer.
Multivariate analyses showed that positive lymph nodes at station 10 (hazard ratio [HR], 0.527; 95% confidence interval [CI], 0.281–0.989; P = 0.046) and IMD (HR, 0.309; 95% CI, 0.142–0.671; P =0.003) were associated with a lower FFLR.
A combined model was generated to evaluate the LR in patents at different risk levels, based on the number of identified risk factors. The 3- and 5-year FFLR rates were as follows: in patients with negative lymph nodes at station 10 and CMD (n = 69), the rates were 90.1% and 88.1%, respectively; in patients with positive lymph nodes at station 10 and CMD (n = 17), the rates were 93.3% and 93.3%, respectively; in patients with negative lymph nodes at station 10 and IMD (n = 76), the rates were 81% and 75.9%, respectively; and in patients with positive lymph nodes at station 10 and IMD (n = 37), the rates were considerably lower at 55.7% and 52%, respectively. The differences in FFLR between patients with one, both or neither of these risk factors were statistically significant (P = 0.000; Figure 6).
Comparison of freedom from locoregional recurrence in patients with different risk factors. Comparison of freedom from locoregional recurrence (FFLR) in patients with resected N1 non–small cell lung cancer and either complete mediastinal lymph node (MLN) dissection and examination (CMD) or incomplete MLN dissection or examination (IMD), and negative lymph nodes (LNs) at station 10 or positive LNs at station 10, shows that those most at risk for LR have both IMD and positive LNs at station 10.
Discussion
The LR rate in patients with resected N1 NSCLC is reported to be 9%–46% (Table 2). In comparison, our data showed a 5-year LR rate of 22.7%. LR risk may now be higher as adjuvant chemotherapies can reduce or delay DM and thereby increase survival times. In addition, better LR control has been associated with improved OS in locally advanced NSCLC patients[14, 15], indicating that a decreased LR rate after surgery might also improve OS, which suggests that PORT could be beneficial in patients with resected N1 NSCLC who are at high risk for LR.
To date, studies on PORT have found no survival benefits for patients with resected N1 NSCLC, and therefore, PORT is not recommended for these patients. Moreover, compared with chemotherapy alone, PORT following adjuvant chemotherapy was found to be associated with detrimental survival in N1 disease patients in the Adjuvant Navelbine International Trialist Association (ANITA) randomized study[7]. The ANITA trial was a randomized study, but the patients that were recommended for PORT were selected by the researchers, so were not randomized[7]; consequently, patient selection bias may have been introduced into the results.
A meta-analysis has also reported similar detrimental effects of PORT in N1 NSCLC patients[8]; however, due to improved technologies, PORT may not be detrimental in all patients with N1 disease. The trials included in the meta-analysis had been carried out using older radiation techniques, such as those that delivered doses using wedges with opposed lateral portals with an excessive volume; used different fractionation schedules ranging from 1.8–3.0 Gy; used different total doses ranging from 30–60 Gy; or used cobalt-60, which has a worse biological efficacy and therapeutic ratio than those achieved with current linear accelerators[16–19]. Treatment-related morbidities and deaths were more prevalent with these outdated radiation techniques than with more modern techniques, which may account for the detrimental survival rates. This has been supported by two recent randomized trials on NSCLC, which investigated PORT with modern radiation techniques. The first showed that PORT was associated with lower LR and higher 5-year OS in patients with postoperative pathological N0 NSCLC[20]; the other found that PORT with modern techniques significantly reduced LR, although there no significant improvement in OS and DFS was observed in patients with postoperative pathological stage T1–3 N0–2 M0 NSCLC[21]. The toxicity of PORT was acceptable in both these trials. These findings suggest that PORT based on modern technologies may promote therapeutic efficacy and could be beneficial for patients with resected pathological N1 NSCLC who are at high risk for LR.
To our knowledge, our present study is the first to identify and report that IMD and positive lymph nodes at station 10 may be risk factors for LR in patients with resected N1 NSCLC, and as such, these patients may warrant further attention. Patients with positive lymph nodes at station 10 are at a higher risk for micrometastases in MLNs through the lymphatic drainage pathway of NSCLC. Studies have reported that the number of resected lymph nodes and the extent of dissected lymph node stations were associated with survival in patients with resectable NSCLC[22–24]. Several studies have recommended that at least six lymph nodes from three MLN stations should be excised[23, 25, 26]; however, others recommend resection of at least six lymph nodes from mediastinal stations and station 10 for accurate nodal staging and prediction of prognosis in patients with resected NI NSCLC[27, 28]. Taken together, these results suggest that the extent of dissected or examined MLN stations may be significantly associated with LR and verify the importance of performing sufficient MLN dissections or examinations.
In this study, we found that patients with resected NI NSCLC and <3 dissected or examined MLN stations had lower FFLR rates than those with ≥3 dissected and examinated MLN stations. Furthermore, our findings showed that the 5-year FFLR rate in patients with IMD (75.9%) was worse than that observed in patients with positive lymph nodes at station 10 (93.3%), indicating that IMD was the greater risk factor for LR (Figure 6). Patients with both risk factors had the highest 5-year LR rate (48%), which was comparable to reported values in resected N2 NSCLC[29]; these patients should therefore be recommended PORT. In contrast, patients with IMD alone should only be considered for PORT after careful consultation between the surgeon and radiation oncologist.
Tumor size has been shown to be a prognostic factor for survival in patients with NSCLC[30–32]. Saynak et al. and Lopez Guerra et al. reported that tumor size was independently associated with LR in resected N1 NSCLC patients[33, 34]. Other reports include three studies which found that lymphovascular invasion was a risk factor for LR in N1 NSCLC patients[33–35]. However, in the study by Lopez Guerra et al.[33], the number of patients with N1 NSCLC was small (16%) compared to the total sample population, and the 5-year LR was much lower (9%) than those reported in previous studies. Several studies have reported visceral pleural invasion as a risk factor for LR[33, 36, 37], and Varlotto et al. observed an increased risk of LR following adjuvant chemotherapy[38]. Surgical procedures, such as lobectomy or pneumonectomy and positive preoperative bronchoscopy have also been associated with a risk of LR in N1 NSCLC patients[30, 35, 39]. However, these reports are inconsistent, and their findings will need further confirmation before being used in patient selection for PORT in N1 NSCLC.
Our retrospective study had the following limitations: It was a single-institution study, and therefore may have had patient selection bias. Some of the patients underwent insufficient MLN dissection or examination, and may have been staged with N2 disease if they had undergone sufficient MLN dissection, which could have introduced staging bias. Patients with concurrent LR and DM may not accurately reflect the pattern of failure observed in this study, and LR that developed before or after DM may not have been identified promptly due to occult symptoms or incomplete radiologic examination. Despite these limitations, our findings support further investigations on the role of PORT in patients with resected N1 NSCLC who have the risk factors for LR identified in this study.
Conclusions
The incidence of LR in patients with surgically resected T1–3N1M0 NSCLC is high. Patients with both IMD and positive lymph nodes at station 10 are at the highest risk for LR, and potentially, the most likely to benefit from adjuvant PORT. Our findings indicate that further investigation of PORT is warranted in this subset of N1 NSCLC patients.
References
Arriagada R, Bergman B, Dunant A, Le Chevalier T, Pignon JP, Vansteenkiste J, International Adjuvant Lung Cancer Trial Collaborative G: Cisplatin-based adjuvant chemotherapy in patients with completely resected non-small-cell lung cancer. N Engl J Med 2004, 350: 351-360.
Douillard JY, Rosell R, De Lena M, Carpagnano F, Ramlau R, Gonzales-Larriba JL, Grodzki T, Pereira JR, Le Groumellec A, Lorusso V, et al.: Adjuvant vinorelbine plus cisplatin versus observation in patients with completely resected stage IB-IIIA non-small-cell lung cancer (Adjuvant Navelbine International Trialist Association [ANITA]): a randomised controlled trial. Lancet Oncol 2006, 7: 719-727. 10.1016/S1470-2045(06)70804-X
Pignon JP, Tribodet H, Scagliotti GV, Douillard JY, Shepherd FA, Stephens RJ, Dunant A, Torri V, Rosell R, Seymour L, et al.: Lung adjuvant cisplatin evaluation: a pooled analysis by the LACE collaborative group. J Clin Oncol 2008, 26: 3552-3559. 10.1200/JCO.2007.13.9030
Arriagada R, Auperin A, Burdett S, Higgins JP, Johnson DH, Le Chevalier T, Le Pechoux C, Parmar MK, Pignon JP, Group NM-aC, et al.: Adjuvant chemotherapy, with or without postoperative radiotherapy, in operable non-small-cell lung cancer: two meta-analyses of individual patient data. Lancet 2010, 375: 1267-1277.
Van Houtte P, Rocmans P, Smets P, Goffin JC, Lustman-Marechal J, Vanderhoeft P, Henry J: Postoperative radiation therapy in lung caner: a controlled trial after resection of curative design. Int J Radiat Oncol Biol Phys 1980, 6: 983-986. 10.1016/0360-3016(80)90105-4
Lally BE, Zelterman D, Colasanto JM, Haffty BG, Detterbeck FC, Wilson LD: Postoperative radiotherapy for stage II or III non-small-cell lung cancer using the surveillance, epidemiology, and end results database. J Clin Oncol 2006, 24: 2998-3006. 10.1200/JCO.2005.04.6110
Douillard JY, Rosell R, De Lena M, Riggi M, Hurteloup P, Mahe MA, Adjuvant Navelbine International Trialist A: Impact of postoperative radiation therapy on survival in patients with complete resection and stage I, II, or IIIA non-small-cell lung cancer treated with adjuvant chemotherapy: the adjuvant Navelbine International Trialist Association (ANITA) Randomized Trial. Int J Radiat Oncol Biol Phys 2008, 72: 695-701. 10.1016/j.ijrobp.2008.01.044
Postoperative radiotherapy in non-small-cell lung cancer: systematic review and meta-analysis of individual patient data from nine randomised controlled trials. PORT meta-analysis trialists group Lancet 1998, 352: 257-263.
Feng QF, Wang M, Wang LJ, Yang ZY, Zhang YG, Zhang DW, Yin WB: A study of postoperative radiotherapy in patients with non-small-cell lung cancer: a randomized trial. Int J Radiat Oncol Biol Phys 2000, 47: 925-929. 10.1016/S0360-3016(00)00509-5
Matsuoka K, Sumitomo S, Misaki N: Prognostic factors in patients with pathologic T1-2N1M0 disease in non-small cell carcinoma of the lung. J Thorac Oncol 2007, 2: 1098-1102. 10.1097/JTO.0b013e31815ba227
Saynak M, Higginson DS, Morris DE, Marks LB: Current status of postoperative radiation for non-small-cell lung cancer. Semin Radiat Oncol 2010, 20: 192-200. 10.1016/j.semradonc.2010.01.008
Edge SB, Compton CC: The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 2010, 17: 1471-1474. 10.1245/s10434-010-0985-4
Rusch VW, Asamura H, Watanabe H, Giroux DJ, Rami-Porta R, Goldstraw P: Members of ISC: The IASLC lung cancer staging project: a proposal for a new international lymph node map in the forthcoming seventh edition of the TNM classification for lung cancer. J Thorac Oncol 2009, 4: 568-577. 10.1097/JTO.0b013e3181a0d82e
Machtay M, Bae K, Movsas B, Paulus R, Gore EM, Komaki R, Albain K, Sause WT, Curran WJ: Higher biologically effective dose of radiotherapy is associated with improved outcomes for locally advanced non-small cell lung carcinoma treated with chemoradiation: an analysis of the Radiation Therapy Oncology Group. Int J Radiat Oncol Biol Phys 2012, 82: 425-434. 10.1016/j.ijrobp.2010.09.004
Machtay M, Paulus R, Moughan J, Komaki R, Bradley J, Choy H, Albain K, Movsas B, Sause WT, Curran WJ: Defining local-regional control and its importance in locally advanced non-small cell lung carcinoma: a radiation therapy oncology group analysis. J Thorac Oncol 2012, 7: 716-722. 10.1097/JTO.0b013e3182429682
Kopelson G, Choi NC: Radiation therapy for postoperative local-regionally recurrent lung cancer. Int J Radiat Oncol Biol Phys 1980, 6: 1503-1506. 10.1016/0360-3016(80)90007-3
Effects of postoperative mediastinal radiation on completely resected stage II and stage III epidermoid cancer of the lung. The lung cancer study group N Engl J Med 1986, 315: 1377-1381.
Stephens RJ, Girling DJ, Bleehen NM, Moghissi K, Yosef HM, Machin D: The role of post-operative radiotherapy in non-small-cell lung cancer: a multicentre randomised trial in patients with pathologically staged T1-2, N1-2, M0 disease. Medical research council lung cancer working party. Br J Cancer 1996, 74: 632-639. 10.1038/bjc.1996.413
Lafitte JJ, Ribet ME, Prevost BM, Gosselin BH, Copin MC, Brichet AH: Postresection irradiation for T2 N0 M0 non-small cell carcinoma: a prospective, randomized study. Ann Thorac Surg 1996, 62: 830-834. 10.1016/S0003-4975(96)00507-3
Trodella L, Granone P, Valente S, Valentini V, Balducci M, Mantini G, Turriziani A, Margaritora S, Cesario A, Ramella S, et al.: Adjuvant radiotherapy in non-small cell lung cancer with pathological stage I: definitive results of a phase III randomized trial. Radiother Oncol 2002, 62: 11-19. 10.1016/S0167-8140(01)00478-9
Mayer R, Smolle-Juettner FM, Szolar D, Stuecklschweiger GF, Quehenberger F, Friehs G, Hackl A: Postoperative radiotherapy in radically resected non-small cell lung cancer. Chest 1997, 112: 954-959. 10.1378/chest.112.4.954
Xu F, Qi L, Yue D, Wang C: The effect of the extent of lymph node dissection for stage IA non-small-cell lung cancer on patient disease-free survival. Clin Lung Cancer 2013, 14: 181-187. 10.1016/j.cllc.2012.09.002
Saji H, Tsuboi M, Yoshida K, Kato Y, Nomura M, Matsubayashi J, Nagao T, Kakihana M, Usuda J, Kajiwara N, et al.: Prognostic impact of number of resected and involved lymph nodes at complete resection on survival in non-small cell lung cancer. J Thorac Oncol 2011, 6: 1865-1871. 10.1097/JTO.0b013e31822a35c3
Nwogu CE, Groman A, Fahey D, Yendamuri S, Dexter E, Demmy TL, Miller A, Reid M: Number of lymph nodes and metastatic lymph node ratio are associated with survival in lung cancer. Ann Thorac Surg 2012, 93: 1614-1619. discussion 1619–1620 10.1016/j.athoracsur.2012.01.065
Little AG, Rusch VW, Bonner JA, Gaspar LE, Green MR, Webb WR, Stewart AK: Patterns of surgical care of lung cancer patients. Ann Thorac Surg 2005, 80: 2051-2056. discussion 2056 10.1016/j.athoracsur.2005.06.071
Ludwig MS, Goodman M, Miller DL, Johnstone PA: Postoperative survival and the number of lymph nodes sampled during resection of node-negative non-small cell lung cancer. Chest 2005, 128: 1545-1550. 10.1378/chest.128.3.1545
De Leyn P, Lardinois D, Van Schil P, Rami-Porta R, Passlick B, Zielinski M, Waller D, Lerut T, Weder W: Ests: European trends in preoperative and intraoperative nodal staging: ESTS guidelines. J Thorac Oncol 2007, 2: 357-361. 10.1097/01.JTO.0000263722.22686.1c
De Leyn P, Lardinois D, Van Schil PE, Rami-Porta R, Passlick B, Zielinski M, Waller DA, Lerut T, Weder W: ESTS guidelines for preoperative lymph node staging for non-small cell lung cancer. Eur J Cardiothorac Surg 2007, 32: 1-8. 10.1016/j.ejcts.2007.01.075
Dai H, Hui Z, Ji W, Liang J, Lu J, Ou G, Zhou Z, Feng Q, Xiao Z, Chen D, et al.: Postoperative radiotherapy for resected pathological stage IIIA-N2 non-small cell lung cancer: a retrospective study of 221 cases from a single institution. Oncologist 2011, 16: 641-650. 10.1634/theoncologist.2010-0343
Sawyer TE, Bonner JA, Gould PM, Foote RL, Deschamps C, Lange CM, Li H: Factors predicting patterns of recurrence after resection of N1 non-small cell lung carcinoma. Ann Thorac Surg 1999, 68: 1171-1176. 10.1016/S0003-4975(99)00678-5
Osaki T, Nagashima A, Yoshimatsu T, Tashima Y, Yasumoto K: Survival and characteristics of lymph node involvement in patients with N1 non-small cell lung cancer. Lung Cancer 2004, 43: 151-157. 10.1016/j.lungcan.2003.08.020
Martini N, Burt ME, Bains MS, McCormack PM, Rusch VW, Ginsberg RJ: Survival after resection of stage II non-small cell lung cancer. Ann Thorac Surg 1992, 54: 460-465. discussion 466 10.1016/0003-4975(92)90435-7
Lopez Guerra JL, Gomez DR, Lin SH, Levy LB, Zhuang Y, Komaki R, Jaen J, Vaporciyan AA, Swisher SG, Cox JD, et al.: Risk factors for local and regional recurrence in patients with resected N0-N1 non-small-cell lung cancer, with implications for patient selection for adjuvant radiation therapy. Ann Oncol 2013, 24: 67-74. 10.1093/annonc/mds274
Saynak M, Veeramachaneni NK, Hubbs JL, Nam J, Qaqish BF, Bailey JE, Chung W, Marks LB: Local failure after complete resection of N0-1 non-small cell lung cancer. Lung Cancer 2011, 71: 156-165. 10.1016/j.lungcan.2010.06.001
Kelsey CR, Marks LB, Hollis D, Hubbs JL, Ready NE, D'Amico TA, Boyd JA: Local recurrence after surgery for early stage lung cancer: an 11-year experience with 975 patients. Cancer 2009, 115: 5218-5227. 10.1002/cncr.24625
Higgins KA, Chino JP, Berry M, Ready N, Boyd J, Yoo DS, Kelsey CR: Local failure in resected N1 lung cancer: implications for adjuvant therapy. Int J Radiat Oncol Biol Phys 2012, 83: 727-733.
Fujimoto T, Cassivi SD, Yang P, Barnes SA, Nichols FC, Deschamps C, Allen MS, Pairolero PC: Completely resected N1 non-small cell lung cancer: factors affecting recurrence and long-term survival. J Thorac Cardiovasc Surg 2006, 132: 499-506. 10.1016/j.jtcvs.2006.04.019
Varlotto JM, Medford-Davis LN, Recht A, Flickinger JC, Schaefer E, DeCamp MM: Failure rates and patterns of recurrence in patients with resected N1 non-small-cell lung cancer. Int J Radiat Oncol Biol Phys 2011, 81: 353-359. 10.1016/j.ijrobp.2010.05.022
Ginsberg RJ, Rubinstein LV: Randomized trial of lobectomy versus limited resection for T1 N0 non-small cell lung cancer. Lung cancer study group. Ann Thorac Surg 1995, 60: 615-622. discussion 622–613 10.1016/0003-4975(95)00537-U
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
CF drafted the manuscript. SG, ZH, LJ, JML participated in data collection, and helped to analyze the data. JH, SG participated in the coordination of the study. LW conceived of the study, participated in its design. All authors made substantial contributions to acquisition and statistical analysis of data, and read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Fan, C., Gao, S., Hui, Z. et al. Risk factors for locoregional recurrence in patients with resected N1 non-small cell lung cancer: a retrospective study to identify patterns of failure and implications for adjuvant radiotherapy. Radiat Oncol 8, 286 (2013). https://doi.org/10.1186/1748-717X-8-286
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1748-717X-8-286