Abstract
We report a case of near fatal aortic thrombosis in a trauma patient homozygous for mutation of Factor V Leiden. He responded well to vascular surgery and intensive care unit management and was discharged successfully from the hospital one month later.
Similar content being viewed by others
Background
Thrombophilia may be described as a congenital or an acquired tendency to arterial and venous thrombosis. Mutation of Factor V Leiden (FVL) appears as a major predisposing factor for venous thromboembolism and has a high prevalence in the Caucasian population [1]. The relative risk (RR) for the first incident of venous thrombosis and the annual incidence (AI) values associated with this mutation are 7.0 and 0.06%, respectively, in heterozygotes. For homozygotes, RR and AI values are projected to be as high as 80 and 0.5-1.0%, respectively [2, 3].
The lifetime probability of developing thrombosis is 2.2 for carriers of the FVL mutation, which is quite low compared to carriers of antithrombin deficiency (8.1), protein S deficiency (8.5) and protein C deficiency (7.3) [4]. There is still debate regarding the utility of lifetime anticoagulation in patients with FVL, with one study randomizing patients on warfarin versus placebo showing a risk value reduction in recurrent venous thromboembolism of 76-80% in the warfarin group. According to the investigators, anticoagulation therapy should exceed a 3-month period after the first venous thromboembolic episode with conventional international normalized ratio (INR) target between 2 and 3 [5, 6]. Carriage of FVL mutation is highly linked to venous but not arterial thrombosis; however, there is growing evidence linking this mutation to an increased risk for arterial involvement, specifically for myocardial infarction [7–9]. We herein present a rare case of aortic thrombosis in a trauma patient that was found to be homozygous for FVL mutation.
Case presentation
A 32-year-old male, presented to the ER of an outside hospital complaining about numbness in both legs after being involved in a street fight 3 days ago. He was a non-smoker with non-significant previous medical history. Physical examination was unrevealing and vital signs were normal. Radiologic evaluation revealed only a fracture of the 10th left rib and the patient was discharged with instructions for bed rest.
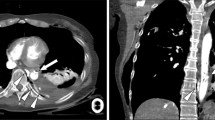
In the next 24 hours he gradually developed abdominal pain and complained about excessively numb and cold legs with normal urination and defecation. By the time he presented to the ER of the same hospital, he could not move his legs. On physical examination, there were no palpable pulses in all arterial sites of both lower extremities. An emergent CT angiography was performed revealing a large (5.8 cm length and 0.8 cm width) thrombus in the descending aorta, causing partial occlusion of its lumen (Figure 1), as well as an infra-renal thrombus extending into both iliac branches, causing complete lumen occlusion. He was started on intravenous drip of unfractionated heparin, clopidogrel and warfarin and a few hours later he was transferred to our department for further management.
A successful surgical recanalization was immediately performed by the vascular surgeons and postoperatively the patient was transferred intubated to our intensive care unit. He subsequently developed rhabdomyolysis with a peak creatine kinase (CK) and myoglobin levels of 130,000 U/L (with CK-MB value of 15,000 U/L) and 3,000, respectively. The LDH level was 6,545 U/L and liver function tests revealed AST and ALT levels of 1,297 and 340 U/L, respectively. He also developed acute renal failure (ARF), hyperkalemia and severe tibial compartment syndrome of the left leg necessitating fasciotomies.
Taking into account the patient's young age, complicated clinical course and laboratory hypercoagulative profile (PLTs were 625,000/ml and fibrinogen was 663 mg/dL), as well as the fact that he had no other clinical or imaging evidence of venous thrombosis, we decided to perform a thrombophilia work-up. The rapid and life-threatening course of the disease had understandably forced the referring physicians from the outside hospital to initiate aggressive anticoagulation therapy. This did not allow us to perform antithrombin III, protein C and S testing. However, the patient was found to carry a homozygous mutation for FVL and also heterozygous mutations for Factor XIII and beta-FIBR. Of interest, his family history was non-significant for thromboses. When renal function improved, we switched from unfractionated heparin to low-molecular weight heparin and administered warfarin aiming at a therapeutic target INR between 2 and 3.
During the rest of his ICU hospitalization he remained hemodynamically stable, his ARF responded well to continuous veno-venous hemodiafiltration and was finally extubated on day 15. The patient was transferred to the Vascular Surgery Department for further management and discharged from the hospital a month later.
Discussion
Cases of heterozygous FVL mutation causing arterial disease are rare and have been described mostly in neonates [10–12]. Other cases of aortic arch and peripheral arterial thrombosis have also been reported in adults [13, 14]. The synergistic effects of FVL mutation and other prothrombotic conditions such as homocystinemia, protein C and S deficiency, oral contraceptives and pregnancy have been also previously described [15].
There are cases of post-traumatic arterial thrombosis of several vascular sites (femoral, renal, cranial, abdominal), not necessarily associated with prothrombotic conditions [16–18]. The incidence of abdominal aortic trauma resulting from blunt force is only around 5% and interestingly the majority of thrombi occur in abdominal aorta [19].
A Medline search triggered by the current case report (literature review performed on April 2, 2011) and using the search terms "abdominal aortic thrombosis" AND "trauma" revealed 15 case reports and 2 case series. Thrombotic episodes were mainly associated with major blunt trauma in automobile accidents (predominantly during childhood), with no clear predisposing thrombotic factors. The low reported number of similar cases does not allow us to safely determine whether the finding of a hypercoagulable genetic profile in a trauma patient experiencing a thrombotic episode is causally linked or merely co-incidental. However, we support the notion that a thrombophilia work-up might be a prudent choice when extensive thromboses are observed in young trauma patients suffering low-impact traumatic injuries.
Conclusions
Homozygous mutation of FVL as well as the arterial site of the first thrombotic event are rare incidents. Although arterial thrombosis occurs commonly on sites of previous vascular pathology (i.e. an atherosclerotic plaque), recent clinical evidence suggests that in cases of extensive arterial thrombosis, a thrombophilia work-up may be required. Aggressive surgical management may be needed if the arterial incident is severe while the lifetime use of warfarin prophylaxis is still debated.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
References
Franchini M, Lippi G: Factor V Leiden and hemophilia. Thromb Res 2010, 125: 119-123. 10.1016/j.thromres.2009.11.003
Koster T, Rosendaal FR, de Ronde H, Briet E, Vandenbroucke JP, Bertina RM: Venous thrombosis due to poor anticoagulant response to activated protein C: Leiden Thrombophilia Study. Lancet 1993, 342: 1503-1506. 10.1016/S0140-6736(05)80081-9
Rosendaal FR, Koster T, Vandenbroucke JP, Reitsma PH: High risk of thrombosis in patients homozygous for factor V Leiden (activated protein C resistance). Blood 1995, 85: 1504-1508.
Martinelli I, Mannucci PM, De Stefano V, et al.: Different risks of thrombosis in four coagulation defects associated with inherited thrombophilia: a study of 150 families. Blood 1998, 92: 2353-2358.
Sarasin FP, Bounameaux H: Decision analysis model of prolonged oral anticoagulant treatment in factor V Leiden carriers with first episode of deep vein thrombosis. BMJ 1998, 316: 95-99.
Ridker PM, Goldhaber SZ, Danielson E, et al.: Long-term, low-intensity warfarin therapy for the prevention of recurrent venous thromboembolism. N Engl J Med 2003, 348: 1425-1434. 10.1056/NEJMoa035029
Dorweiler B, Neufang A, Kasper-Koenig W, Schinzel H, Schmiedt W, Oelert H: Arterial embolism to the upper extremity in a patient with factor V Leiden mutation (APC resistance)--a case report and review of the literature. Angiology 2003, 54: 125-130. 10.1177/000331970305400117
Middendorf K, Gohring P, Huehns TY, Seidel D, Steinbeck G, Nikol S: Prevalence of resistance against activated protein C resulting from factor V Leiden is significantly increased in myocardial infarction: investigation of 507 patients with myocardial infarction. Am Heart J 2004, 147: 897-904. 10.1016/j.ahj.2003.10.048
Mansourati J, Da Costa A, Munier S, et al.: Prevalence of factor V Leiden in patients with myocardial infarction and normal coronary angiography. Thromb Haemost 2000, 83: 822-825.
Patel RK, Ingram W, MacCarthy P, Arya R: Is homozygosity for factor V Leiden a risk factor for myocardial infarction in young women who smoke? Thromb Haemost 2005, 93: 616-661.
Doix S, Mahrousseh M, Jolak M, Laurent Y, Lorenzini JL, Binquet C, Zeller M, Cottin Y, Wolf JE: Factor V Leiden and myocardial infarction: a case, review of the literature with a meta-analysis. Ann Cardiol Angeiol (Paris) 2003, 52: 143-149. 10.1016/S0003-3928(02)00192-0
Metsvaht T, Hermlin T, Kern H, Kahre T, Starkopf J: Aortic arch thrombosis in a neonate with heterozygous carrier status of factor V Leiden mutation. Congenit Heart Dis 2006, 1: 40-45. 10.1111/j.1747-0803.2006.00007.x
Ng T, Brown JR, Edmondson RA, Tillyer ML: Catastrophic arterial thromboembolism associated with factor V Leiden. Eur J Vasc Endovasc Surg 2000, 19: 551-553. 10.1053/ejvs.1999.0971
Mandegar MH, Saidi B, Roshanali F: Extensive arterial thrombosis in a patient with factor V Leiden mutation. Interact Cardiovasc Thorac Surg 2010, 11: 127-129. 10.1510/icvts.2010.232710
Page C, Rubin LE, Gusberg RJ, Dardik A: Arterial thrombosis associated with heterozygous factor V Leiden disorder, hyperhomocysteinemia, and peripheral arterial disease: importance of synergistic factors. J Vasc Surg 2005, 42: 1014-1018. 10.1016/j.jvs.2005.06.019
Bahloul M, Abid D, Ketata H, Kallel H, Dammak H, Chelly H, Ben Hamida C, Mhiri MN, Bouaziz M: Traumatic unilateral renal artery thrombosis and protein C deficiency. A case report. J Mal Vasc 2006, 31: 277-279.
Leo LA, Grigoratos C, Spontoni P, Violo C, Balbarini A: An unusual case of traumatic occlusion of the left common femoral artery: a case report. J Cardiovasc Med (Hagerstown) 2010, in press.
Kim C, Jeon W, Shin T, Choi D, Kim J, Lee C, Choi J: Stent-assisted recanalisation of acute occlusive arteries in patients with acute limb ischaemia. Eur J Vasc Endovasc Surg 2010, 39: 89-96. 10.1016/j.ejvs.2009.09.023
Kepros J, Angood P, Jaffe CC, Rabinovici R: Aortic intimal injuries from blunt trauma: resolution profile in nonoperative management. J Trauma 2002, 52: 475-78. 10.1097/00005373-200203000-00010
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
TI and PK participated in patient management and data collection, TG participated in patient management, data collection and drafted the manuscript, TA carried out the thrombophilia work-up and AA participated in patient management, supervised and approved the manuscript. All authors read and approved the final manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Tsangaris, I., Tsaknis, G., Tsantes, A. et al. Life-threatening aortic thrombosis in a trauma patient homozygous for factor V Leiden mutation: Case report. Thrombosis J 9, 8 (2011). https://doi.org/10.1186/1477-9560-9-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1477-9560-9-8