Abstract
Background
The evidence base of clinical interventions in paediatric hospitals of developing countries has not been formally assessed. We performed this study to determine the proportion of evidence-based therapeutic interventions in a paediatric referral hospital of a developing country
Methods
The medical records of 167 patients admitted in one-month period were revised. Primary diagnosis and primary therapeutic interventions were determined for each patient. A systematic search was performed to assess the level of evidence for each intervention. Therapeutic interventions were classified using the Ellis score and the Oxford Centre for Evidence Based Medicine Levels of Evidence
Results
Any dehydration due to diarrhoea (59 cases) and pneumonia (42 cases) were the most frequent diagnoses. Based on Ellis score, level I evidence supported the primary therapeutic intervention in 21%, level II in 73% and level III in 6% cases. Using the Oxford classification 16%, 8%, 1% and 75% therapeutic interventions corresponded to grades A, B, C, and D recommendations, respectively. Overall, according to Ellis score, 94% interventions were evidence based. However, out of the total, 75% interventions were based on expert opinion or basic sciences. Most children with mild to moderate dehydration (52 cases) were inappropriately treated with slow intravenous fluids, and most children with non-complicated community acquired pneumonia (42 cases) received intravenous antibiotics
Conclusions
Most interventions were inappropriate, despite the availability of effective therapy for several of them. Diarrhoeal dehydration and community acquired pneumonia were the most common diagnoses and were inappropriately managed. Existing effective interventions for dehydration and pneumonia need to be put into practice at referral hospitals of developing countries. For the remaining problems, there is the need to conduct appropriate clinical studies. Caution must be taken when assigning the level of evidence supporting therapeutic interventions, as commonly used classifications may be misleading
Similar content being viewed by others
Background
Previous studies have shown that medical interventions based on scientific evidence range from 10 to 80% [1–4]. These studies were performed in a broad spectrum of patients and settings in developed countries.
In paediatric practice, the proportion of evidence based interventions reported ranges from 75 to 91% [5–8]. These studies are clearly relevant to the quality of care in developed countries, with strong health systems, widely available high technology and qualified human resources. However, health services in developing countries are frequently weak, and they face too often severe lack of expensive technology. In addition, the level of qualification of health personnel may vary greatly within health facilities, even at referral level and in urban areas. Moreover, the prevalent childhood illnesses in developed countries are not necessarily those prevalent in developing countries.
The assessment of quality of care at referral level for severely ill children is an important component of the efforts for reducing the child mortality rate in poor countries, for reducing the burden on health systems and for investing money in favour of high priority health interventions [9, 10]. Thus we were prompted to assess the proportion of interventions based on sound scientific base in a paediatric referral setting of a developing country.
Methods
Referral care provided to children hospitalized in the paediatric department of the Instituto Especializado de Salud del Niño (IESN) was assessed for evidence base. IESN is a national paediatric hospital with more than 500 inpatient beds, serving mostly patients from deprived socioeconomic areas of Lima and inner cities of the country.
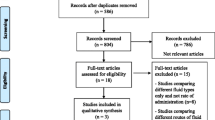
The clinical records of 195 children aged 1 month through 16 years old and hospitalized during January 2003 were initially revised.
One of the investigators (NYC) assessed the clinical records of children and assigned to each one a primary diagnosis and one or more primary therapeutic interventions, on the basis of the main clinical features and/or definitive diagnostic laboratory aids. Patients in whom a primary diagnosis was not possible to determine or those without a clear diagnosis were excluded.
The primary intervention was defined as the treatment or other manoeuvre that represented the most important attempt to cure, alleviate, or care for the patient in respect of his or her primary diagnosis [3].
To determine the level of evidence for each primary intervention, Cochrane reviews were searched. If there was not such a systematic review, a search through PubMed (MEDLINE) was performed by one of the investigators (NYC). All Cochrane reviews were searched through their own search tools. For PubMed, the period of search was 1966 through 2002. The key words used included those related to the primary diagnosis (e.g., pneumonia). Limits: "Title", "All child: 0–18 years". Publication type was sequentially searched for "Practice Guideline", "Meta-Analysis", "Randomized Controlled Trial" and "Review". Articles in English or Spanish were included. The National Guideline Clearinghouse was additionally visited for additional references. Published recommendations for judging the quality of guidelines were used for deciding the selection of the guidelines [11]. In addition, Clinical Evidence was used whenever deemed pertinent.
The level of evidence assigned to interventions was based on Ellis score (levels I, II and III) and the Oxford Centre for Evidence Based Medicine Levels of Evidence (grades A, B, C and D) [3, 12]. Ellis score considers one or more interventions for a given diagnosis as one primary intervention. For comparison purposes we ranked each individual intervention through Oxford classification.
As a next step to our study, we planned the dissemination of the results among the hospital policy makers and the suggestion of corrective courses of action for those interventions needing improvement.
Results
Results of the search strategies for PubMed are included as an appendix [See Additional File 1]. A guideline on management of pain in sickle cell disease was found in the National Guideline Clearinghouse website and the results of the search are also shown at the end of the appendix [See Additional File 1].
Overall, one hundred and ninety five clinical records were revised. Twenty eight clinical records were excluded because of undefined primary diagnosis (Table 1). One hundred and sixty seven remaining clinical records were further assessed. The most frequent primary diagnoses are shown in Table 2, being diarrhoeal dehydration and pneumonia the main causes for hospitalization. The childhood prevalent diseases are quite constant throughout the year at our hospital and thus it is unlikely that the results would have been different if we had chosen another study period.
Out of 167 primary interventions, 21% were supported by level I evidence, 73% were level II, and 6% were ranked as level III, according to Ellis classification [3]. Table 3 shows that most interventions classified as level I are referred to acute asthma exacerbations. Nebulized beta-agonists and systemic corticosteroids in bronchiolitis, and antibiotics for acute otitis media were considered level I according to Ellis. They were classified as D{5} according to Oxford Centre for Evidence Based Medicine Levels of Evidence (Table 3) [12].
Most assessed interventions were considered as level II (Table 4). Diarrhoeal dehydration and community-acquired pneumonia were the predominant diagnoses. Considering each prescription separately (fluid restriction, furosemide, spironolactone and captopril in heart failure, for example) we obtained 146 interventions. When we assessed them through the Oxford classification, 11% interventions were classified as grade B, 1% as grade C, and 88% as grade D. Appropriate interventions for the same diagnoses presented in Table 4 and ranked by Oxford classification are shown in Table 5.
Overtly unsubstantiated therapy according to Ellis classification is shown in Table 6. Considering levels I and II evidence-based therapy, 94% of therapeutic interventions were evidence based through Ellis classification. Using the Oxford classification, we obtained 193 individualized therapeutic interventions, that were classified as Grades A (16%), B (8%), C (1%), and D (75%).
Comparison of grade of recommendation of the prescribed intervention with the appropriate one is shown in Table 7. It will be used as summary evidence documenting our current hospital health care quality standard.
Discussion
In this study 94% of therapeutic interventions were evidence-based by Ellis score. It may seem encouraging that more than 90% of therapeutic decisions in a referral paediatric hospital of a developing country are evidence based. However, the level II of evidence from Ellis includes interventions based in cohort studies, case-control studies, case series, expert's opinion, and even those based in basic sciences. We attempted therefore to classify the primary interventions according to more specific criteria. Using the Oxford classification, 75% of therapeutic interventions were based in expert opinions or in basic sciences (Grade of Recommendation D).
Some limitations of our study include the possible author' bias when assigning the primary diagnosis and primary intervention. The assignment of diagnosis by the clinician may have been influenced by both the choice of treatment and the available evidence. Only one of us classified the primary intervention. In addition, we evaluated only a primary intervention for a single primary diagnosis. Actually, many patients had more than one diagnosis and obviously more than one therapeutic intervention.
We used as evidence-base for rating the interventions assessed in our study, guidelines and evidence-based resources published in the developed world. This raises the issue of whether they are fully applicable to our setting. The most prevalent conditions found were diarrhoeal dehydration and community acquired pneumonia. For both of them we used British produced guidelines [20, 21] because there were not Cochrane reviews on them and because the guidelines fulfilled recommended criteria for methodological quality of published guidelines [11]. The main recommendation of the guidelines on diarrhoea favours rapid oral rehydration over intravenous rehydration for children with mild to moderate dehydration [20]. This recommendation is based on several studies performed in both developed and developing countries and thus it can be applicable to both settings. The only concern on the applicability from setting to setting is that related to the osmolarity of the oral rehydration solution (ORS). The guidelines recommend a solution with 60 mmol/l of sodium, whereas a recent expert consensus found sufficient evidence to recommend the universal use of an ORS containing 75 mmol/l of sodium [49].
Regarding community acquired pneumonia, the British guidelines recommend antibiotic treatment for all children with pneumonia, due to the difficulties in identifying the aetiology, and they also specify criteria for hospitalization [21]. These recommendations are in agreement with the World Health Organization published guidelines [50]. The main difference is that the WHO guidelines rest on fast breathing and chest retraction for the diagnosis of pneumonia, whereas the British guidelines emphasize the role of chest x-rays. Chest x-rays are widely available in referral hospitals in developing countries and thus they should be used in addition to the clinical findings.
We acknowledge that the evidence derived from studies performed in developed countries should be translated with caution to developing settings. However, when the native research is scarce or of low quality, we think that the transfer of knowledge from the developed countries is an acceptable approach, as far as the particular characteristics of patients in developing countries are considered on an individual basis.
Dehydration due to diarrhoea and pneumonia were the most frequent diagnoses. Oral rehydration for diarrhoeal dehydration and antibiotics for pneumonia are considered as interventions with sufficient evidence for implementing them widely [9, 10]. In our study, all children with mild to moderate dehydration were treated with slow intravenous infusion, and most children with uncomplicated community acquired pneumonia received intravenous antibiotics.
In addition to their enormous potential for saving lives, outpatient antibiotic therapy for pneumonia and outpatient oral rehydration can drastically reduce the rate of hospitalizations, the hospital stay, the hospital mortality rate, and the costs incurred. At our hospital, the mean stay time for hospitalized children is 4.7 days, and the mean crude mortality rate is 3.6%. We estimated the cost of managing hospitalized children with pneumonia and diarrhoeal dehydration as US$ 10.6/day and US$ 8.6/day, respectively. These costs are referred only to hospital bed and laboratory tests. A substantial amount of money could be saved treating these conditions on an outpatient basis.
We planned the dissemination of our results among the hospital policy makers. The tools that will be suggested for improving the standards include the development and systematic application of locally produced guidelines and/or the adaptation of published guidelines. A useful alternative that has been experienced for several years at our inpatient ward unit is to make available personal computers connected to Internet for attending physicians, residents and interns, and to encourage the use of online evidence-based resources. This last alternative may work better, particularly where there are motivated physicians who are able to lead the efforts for improving the health care standards. However, the ultimate decision to systematically introduce and monitor the suggested changes will rest on hospital managers. Such changes should also depend on taking into account the role of several other determinants of the clinical decision making by individual practitioners, such as continuous training, motivation, time, availability of drugs, equipments and supplies, supervision, and long-term health system strengthening strategies.
Conclusions
Caution must be taken when assigning the level of evidence that supports therapeutic interventions, as commonly used classifications may be misleading. Existing effective interventions for dehydration and pneumonia are not being implemented in developing countries, even at referral level, and thus there is the need to change the current medical interventional behaviours. For the remaining diagnoses, the majority of assessed interventions were based on weak or non-existent evidence, highlighting the need to conduct appropriate clinical studies.
References
Office of Technology Assessment of the Congress of the United States: Assessing the efficacy and safety of medical technologies. 1978, Washington, DC: US Government Printing Office
Dubinsky M, Ferguson JH: Analysis of the National Institutes of Health Medicare Coverage Assessment. Int J Technol Assess Health Care. 1990, 6: 480-488.
Ellis J, Mulligan I, Rowe J, Sackett DL: Inpatient general medicine is evidence based. Lancet. 1995, 346: 407-410. 10.1016/S0140-6736(95)92781-6.
Gill P, Dowell AC, Neall RD, Smith N, Heywood P, Wilson AE: Evidence based general practice: a retrospective study of interventions in one training practice. BMJ. 1996, 312: 819-821.
Kenny SE, Shankar KR, Rintala R, Lamont GL, Lloyd DA: Evidence based surgery: interventions in a regional paediatric surgical unit. Arch Dis Child. 1997, 76: 50-55.
Rudolf MC, Lyth N, Bundle A, Rowland G, Kelly A, Bosson S: A search for the evidence supporting community paediatric practice. Arch Dis Child. 1999, 80: 257-261.
Curley AE, Tubman TR, Halliday HL: Tratamiento de los recién nacidos de muy bajo peso al nacer ¿Se basa en la evidencia?. An Esp de Ped. 2000, 52: 554-560.
Moyer VA, Gist AK, Elliott AJ: Is the practice of paediatric inpatient medicine evidence based?. J Paediatr Child Health. 2002, 38: 347-351. 10.1046/j.1440-1754.2002.00006.x.
Jones G, Steketee RW, Black RE, Bhutta ZA, Morris SS, the Bellagio Child Survival Study Group: How many child deaths can we prevent this year?. Lancet. 2003, 362: 65-71. 10.1016/S0140-6736(03)13811-1.
The Bellagio Study Group on Child Survival: Knowledge into action for child survival. Lancet. 2003, 362: 323-27. 10.1016/S0140-6736(03)13977-3.
Naylor CD, Guyatt G: Users' guides to the medical literature. XI. How to use an article about a clinical utilization review. Evidence-Based Medicine Working Group. JAMA. 1996, 275: 1435-1439. 10.1001/jama.275.18.1435.
Levels of Evidence and Grades of Recommendation. [http://www.cebm.net/levels_of_evidence.asp]
Asthma and Other Wheezing Disorders in Children. [http://www.clinicalevidence.com/ceweb/conditions/chd/0302/0302.jsp]
Bronchiolitis. [http://www.clinicalevidence.com/ceweb/conditionpdf/0308.pdf]
American Academy of Pediatrics: The Neurodiagnostic Evaluation of the Child with a First Simple Febrile Seizure. Pediatrics. 1996, 97: 769-775.
Stevens D, Smith L, Bruss J, et al: Randomized comparison of Linezolid (PNU-100766) versus oxacillin-dicloxacillin for treatment of complicated skin and soft tissue infections. Antimicrob Agents Chemoter. 2000, 44: 3408-3413. 10.1128/AAC.44.12.3408-3413.2000.
Acute Otitis Media. [http://www.clinicalevidence.com/ceweb/conditionpdf/0301.pdf]
Osmond M, Evans D: Croup. In Clinical Evidence: A compendium of the best available evidence for effective health care. Edited by: Godlee F. 2000, London. BMJ Publishing Group, 195-205.
Jongsuksuntigul P, Jeradit C, Pornpattanakul S, Charanasri U: A comparative study on the efficacy of albendazole and mebendazole in the treatment of ascariasis, hookworm infection and trichuriasis. Southeast Asian J Trop Med Public Health. 1993, 24: 724-729.
Armon K, Stephenson T, MacFaul R, Eccleston P, Werneke U: An evidence and consensus based guideline for acute diarrhoea management. Arch Dis Child. 2001, 85: 132-142. 10.1136/adc.85.2.132.
British Thoracic Society of Standards of Care Committee: BTS Guidelines for the Management of Community Acquired Pneumonia in Childhood. Thorax. 2002, i1-24. Suppl 1
Uretsky BF, Pina I, Quigg RJ, Brill JV, MacInerney EJ, Mintzer R, Armstrong PW: Beyond drug therapy: Non-pharmacologic care of the patient with advanced heart failure. Am Heart J. 1998, 135: 264-284.
Pitt B, Zannad F, Remme WJ, Cody R, Castaigne A, Perez A, Palensky J, Wittes J, for The Randomized Aldactone Evaluation Study Investigators: The effect of spironolactone on morbidity and mortality in patients with severe heart failure. N Engl J Med. 1999, 341: 709-717. 10.1056/NEJM199909023411001.
Rheuban KS, Carpenter MA, Ayers CA, Gutgesell HP: Acute hemodynamic effects of converting enzyme inhibition in infants with congestive heart failure. J Pediatr. 1990, 117: 668-670.
Krasnoff AR, Mangione RA: Blood products used in the treatment of hemophilia. Hosp Pharm. 1982, 17: 598-599.
Smith M: Cyanosis in the infant. In Handbook of Pediatric Emergencies. Edited by: Baldwin G. 2001, Philadelphia: Lippincott Williams and Wilkins, 277-280. 3
Zar H, Cotton M: Nosocomial pneumonia in pediatric patients. Practical problems and rational solutions. Pediatr Drugs. 2002, 4: 73-83.
Guideline for the management of acute and chronic pain in sickle cell disease. [http://www.guidelines.gov/summary/summary.aspx?doc_id=2621&nbr=1847&string=sickle-cell+AND+anemia]
Krishna Kumar R: A Practical approach for the diagnosis and management of dilated cardiomyopathy. Indian J Pediatr. 2002, 69: 341-350.
Bengur AR, Beekman RH, Rochini AP, Crowley DC, Schork MA, Rosenthal A: Acute hemodynamic effects of captopril in children with a congestive or restrictive cardiomyopathy. Circulation. 1991, 83: 523-527.
Canadian Pediatric Society Statement: Management of the pediatric patient with generalized convulsive status epilepticus in the emergency department. Pediatrics & Child Health. 1996, 1: 151-155.
Appleton R, Martland T, Phillips B: Drug management for acute tonic-clonic convulsions including convulsive status epilepticus in children (Cochrane Review). In: The Cochrane Library. 2003, Oxford: Update Software, 1
El Bashir H, Laundy M, Booy R: Diagnosis and treatment of bacterial meningitis. Arch Dis Child. 2003, 88: 615-620. 10.1136/adc.88.7.615.
World Health Organization: The management of bloody diarrhoea in young children. 1994, Geneva; WHO/CDD/94.49
Pisani E, Bartoletti R, Trinchieri A, Rizzo M: Lomefloxacin versus ciprofloxacin in the treatment of complicated urinary tract infections: a multicenter study. J Chemother. 1996, 8: 210-213.
Al-Omran M, Groof A, Wilke D: Enteral versus parenteral nutrition for acute pancreatitis (Cochrane Review). In: The Cochrane Library. 2003, Oxford: Update Software, 1
Pietzak M, Thomas D: Pancreatitis in childhood. Pediatr Rev. 2000, 21: 406-412.
Mayumi T, Ura H, Arata S, Kitamura N, Kiriyama I, Shibuya K, Sekimoto M, Nago N, Hirota M, Yoshida M, Ito Y, Hirata K, Takada T, Working Group for the Practical Guidelines for Acute Pancreatitis. Japanese Society of Emergency Abdominal Medicine: Evidence-based clinical practice guidelines for acute pancreatitis: proposals. J Hepatobiliary Pancreat Surg. 2002, 9: 413-422. 10.1007/s005340200051.
Beamon RF, Siegel CJ, Landers G, Green V: Hydrocarbon ingestion in children: a six-year retrospective study. JACEP. 1976, 5: 771-775.
Mencías E: Intoxicaciones por productos industriales: hidrocarburos. JANO Medicina y Humanidades. 1998, 54: 38-42.
DiMarco JP, Miles W, Akhtar M, Milstein S, Sharma AD, Platia E, McGovern B, Scheinman MM, Govier WC, The Adenosine for PSVT Study Group: Adenosine for paroxysmal supraventricular tachycardia: dose ranging and comparison with verapamil. Assessment in placebo-controlled, multicenter trials. Ann Intern Med. 1990, 113: 104-110.
Jacobson SJ, Griffiths K, Diamond S, Winders P, Sgro M, Feldman W, Macarthur C: A randomized controlled trial of penicillin vs clindamycin for the treatment of aspiration pneumonia in children. Arch Pediatr Adolesc Med. 1997, 151: 701-704.
Daaboul Y, Vern BA, Blend MJ: Brain SPECT imaging and treatment with IVIG in acute post-infectious cerebellar ataxia: case report. Neurol Res. 1998, 20: 85-88.
George JN, Woolf SH, Raskob GE, Wasser JS, Aledort LM, Ballem PJ, Blanchette VS, Bussel JB, Cines DB, Kelton JG, Lichtin AE, McMillan R, Okerbloom JA, Regan DH, Warrier I: Idiopathic Thrombocytopenic Purpura: A practice guideline developed by explicit methods for the American Society of Hematology. Blood. 1996, 88: 3-40.
Sonmez K, Demirogullari B, Ekingen G, Turkyilmaz Z, Karabulut R, Basaklar AC, Kale N: Randomized, placebo-controlled treatment of anal fissure by lidocaine, EMLA, and GTN in children. J Pediatr Surg. 2002, 37: 1313-1316. 10.1053/jpsu.2002.34997.
Kenny SE, Irvine T, Driver CP, Nunn AT, Losty PD, Jones MO, Turnock RR, Lamont GL, Lloyd DA: Double blind randomized controlled trial of topical glyceryl trinitrate in anal fissure. Arch Dis Child. 2001, 85: 404-407. 10.1136/adc.85.5.404.
Durongpisitkul K, Gururaj VJ, Park JM, Martin CF: The prevention of coronary artery aneurysm in Kawasaki disease: a meta-analysis on the efficacy of aspirin and immunoglobulin treatment. Pediatrics. 1995, 96: 1057-1061.
Masaru T, Stanford S: Prevalence of coronary artery abnormalities in Kawasaki disease is highly dependent on gamma globulin dose but independent of salicylate dose. J Pediatr. 1997, 131: 888-893.
Reduced Osmolarity Oral Rehydration Salts (ORS) Formulation. Report from a Meeting of Experts Jointly Organized by UNICEF and WHO. [http://www.who.int/child-adolescent-health/New_Publications/NEWS/Expert_consultation.htm]
World Health Organization: Acute respiratory infections in children: case management in small hospitals in developing countries. 1990, Geneva; WHO/ARI90.5
Pre-publication history
The pre-publication history for this paper can be accessed here:http://www.biomedcentral.com/1472-6963/4/40/prepub
Acknowledgements
We gratefully acknowledge the contribution of Drs. Felipe Lindo Pérez and Carlos Alamo Solís for their suggestions to earlier manuscript drafts. Mr. Armando Barrientos provided statistical support.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The author(s) declare that they have no competing interests.
Authors' contributions
NYC and LH conceived and designed the study. All authors analyzed and interpreted the data and contributed to earlier drafts of the manuscript.
Electronic supplementary material
12913_2004_99_MOESM1_ESM.doc
Additional File 1: "Appendix: Literature search results" details of the Medline (PubMed) search strategy and of the results are provided in this additional file. The selected articles are in black, bold characters. In addition, the search results from the National Guideline Clearinghouse website are provided for painful crisis in sickle cell anaemia. (DOC 2 MB)
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Carreazo, N.Y., Bada, C.A., Chalco, J.P. et al. Audit of therapeutic interventions in inpatient children using two scores: are they evidence-based in developing countries?. BMC Health Serv Res 4, 40 (2004). https://doi.org/10.1186/1472-6963-4-40
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1472-6963-4-40