Abstract
Background
Pramipexole exists as two isomers. The S(-) enantiomer is a potent D3/D2 receptor agonist and is extensively used in the management of PD. In contrast, the R(+) enantiomer is virtually devoid of any of the DA agonist effects. Very limited studies are available to characterize the pharmacological spectrum of the R(+) enantiomer of pramipexole.
Results
Using differentiated SH-SY5Y neuroblastoma cells as an experimental model, here we show that S(-) and R(+) pramipexole are endowed with equipotent efficacy in preventing cell death induced by H2O2 and inhibiting mitochondrial reactive oxygen species generation. Both pramipexole enantiomers prevented mitochondrial ROS generation with a potency about ten times higher then that elicited for neuroprotection.
Conclusions
These results support the concept of both S(-) and R(+) pramipexole enantiomers as mitochondria-targeted antioxidants and suggest that the antioxidant, neuroprotective activity of these drugs is independent of both the chiral 6-propylamino group in the pramipexole molecule and the DA receptor stimulation.
Similar content being viewed by others
Background
Parkinson's disease (PD) is the most common neurodegenerative movement disorder. The primary cause of the disorder is the progressive loss of the pigmented dopaminergic neurons in the substantia nigra pars compacta (SNpc) accompanied by the appearance of intracytoplasmic inclusions known as Lewy bodies [1–3].
To date, the etiopathogenesis of nigral dopaminergic neuron loss in PD is unknown. However, the presence of ongoing oxidative stress as the result of compromised antioxidant defence mechanisms and generation of radical oxygen species (ROS) in the SNpc of the parkinsonian brain are considered to be important Pathogenic mechanisms [3, 4]. ROS can react with cellular macromolecules through oxidation and cause the cells to undergo dysfunction and eventually lead to necrosis or apoptosis. The control of the redox environment of the cell provides an additional regulation in the signal transduction pathways which are redox sensitive. Therefore, an effective anti-parkinsonian therapy should not only alleviate the disease associated symptoms, but should also stop the progressive dopaminergic cell death in the SN.
Modification of the rate of PD progression is currently a highly debated topic. Increased oxidative stress is indeed thought to be involved in the nigral cell death which is a well established peculiar neuropathological feature of PD. These mechanisms have been proven in vitro and in animal models, but their relevance in humans remains speculative [5, 6]. However, several dopamine (DA) agonists of the DA D2-receptor family (including D2 and D3 subtypes) have recently been shown to possess neuroprotective properties in different in vitro and in vivo experimental PD models [7, 8]. At cellular level, independent groups have demonstrated decreased free radical production and an amelioration of DA neuronal loss following DA agonist treatment [9–17]. Interestingly, not all the neuroprotective effects were clearly mediated by DA-receptor stimulation.
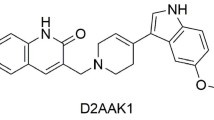
Pramipexole (2-amino-4,5,6,7-tetrahydro-6-propylaminobenzathiazole) is a non-ergot DA agonist that has been successfully applied to the treatment of Parkinson's disease. Pramipexole exhibits a high affinity for the D2 and D3 DA receptor subtypes but little or no affinity for the D1 receptor family. The neuroprotective effects elicited by this drug have directly and/or indirectly been associated with antioxidant effects, mitochondrial stabilization or induction of the antiapoptotic Bcl-2 family [18–21]. In particular, Le et al., [18] reported that pramipexole protected DAergic MES 23.5 cell line against DA, 6-OH-DA and hydrogen peroxide (H2O2)-induced cytotoxicity possibly through antioxidant effects, and such neuroprotection was independent from DA receptor stimulation not being prevented by selective D2 or D3 antagonists. Similar results were obtained by Fujta et al., [20] and Uberti et al [22], who demonstrated that pramipexole inhibited generation of H2O2-induced reactive oxygen species in PC12 cells and SH-SY5Y neuroblastoma cells, respectively, in a DA receptor independent way. Recent data also demonstrated neuroprotection by pramipexole against β-amyloid ROS generation and toxicity [19, 22].
Pramipexole exists as two isomers. The S(-) enantiomer is a potent D2/D3receptor agonist and is extensively used in the management of PD. In contrast, the R(+) enantiomer is virtually devoid of any of the DA agonist effects. Very limited studies are available to characterize the pharmacological spectrum of the R(+) enantiomer of pramipexole [19, 22–27].
Here we show that S(-) and R(+) pramipexole are endowed with equipotent efficacy in preventing cell death induced by H2O2 and act as mitochondria-targeted antioxidants.
Results
Neuroprotection against H2O2
SH-SY5Y neuroblastoma cell lines were differentiated with 10 μM all-trans retinoic acid for 1 week to acquire a neuronal phenotype. Cells were then challenged with 1 mM H2O2 for 5 min then cells returned to fresh medium for additional 24 h. H2O2 caused a reduction in cell viability of about 70% in comparison with untreated control cells (figure 1). As shown in figure 1A, treatment of the cells with increasing concentrations of S(-) or R(+) pramipexole dose-dependently prevented the viability impairment induced by H2O2. The tested drugs showed equipotent efficacy with calculated IC50 values of 8.8 ± 0.9 μM and 9.2 ± 0.6 μM for S(-) and R(+) pramipexole enantiomer, respectively. The neuroprotective effects of both pramipexole enantiomers were not prevented by preincubation of the cells with 10 μM phenoxybenzamine (data not shown), 10 μM haloperidol or 10 μM (-) sulpiride (Figure 1B). Haloperidol and sulpiride treatments did not induce cell viability modifications (data not shown).
Neuroprotective effects of pramipexole (PPX) enatiomers against H 2 O 2 -induced cell death. A) Differentiated SH-SY5Y cells were exposed to different concentrations of S(-) PPX (gray bars) and R(+) PPX (black bars) for 1 h before being exposed to 1 mM H2O2 for 10 min. Cell viability was evaluated 24 h after by MTT assay B) Cells were exposed to 50 μM μM S(-) PPX or R(+) PPX in the presence or absence of 10 μM haloperidol (H) or 10 μM (-) sulpiride (S). Data represent means ± SEM of at least three different experiments and are from three separate cell preparations. *, p < 0.01 vs H2O2 alone values.
Inhibition of mitochondrial ROS generation
The effects of pramipexole and its R(+) enantiomer have been studied in an experimental model of mitochondrial ROS generation by video-rate confocal microscopy in living neuronal cells. This model allows detection of ROS levels specifically generated in mitochondria and is based on the CM-DCF formation after laser light stimulation [28–30]. Figure 2A, upper panel, shows the results from a representative experiment. Mitochondrial ROS generation was evaluated in cells after increasing exposure to laser at different intensity. In a parallel experiment (lower panels), cells were preincubated with Vitamin E (2 μl/100 ml) for 30 min before the laser excitation. Fluorescence emission intensity was calculated as average grey level value per pixel and corrected for background. Data are reported in the graph reported in Figure 2B. The results clearly show that Vitamin E prevented laser-induced ROS generation in mitochondria of differentiated SH-SY5Y neuronal cells.
Detection of mitochondrial ROS generation. A) Upper panel. Representative pictures from cells exposed to increasing laser intensity, as indicated. CM-DCF fluorescence intensity (green) was selectively recorded in mitochondria (red). Lower panel. Cells were preincubated with Vitamin E (2 ng/100 μl) for 30 min before the laser excitation (white bars in panel B). Fluorescence emission intensity was calculated as average grey level value per pixel and corrected for background. Bars in panel B represent the means ± SEM of at least three different experiments and are from three separate cell preparations. *, p < 0.01 vs the corresponding control values.
Using the same experimental paradigm, we tested the effects of different concentrations of S(-) and R(+) pramipexole in laser-induced mitochondria ROS generation. As shown in figure 3, both S(-) and R(+) pramipexole dose-dependently prevented laser-induced ROS generation in mitochondria of differentiated SH-SY5Y neuronal cells. When calculated as inhibition of ROS generation after 9% laser intensity, both drugs showed similar potency with IC50 values of 0.91 ± 0.14 μM and 0.85 ± 0.21 μM for S(-) and R(+) pramipexole enantiomer, respectively. The prevention of mitochondrial ROS generation induced by both pramipexole enantiomers was not affected by preincubation of the cells with 10 μM phenoxybenzamine (data not shown), 10 μM haloperidol or 10 μM (-) sulpiride (Figure 4). Haloperidol and sulpiride treatments did not modify laser-induced increase in ROS production (data not shown).
Inhibition of mitochondrial ROS generation by pramipexole (PPX) enantiomers. Cells were exposed to different concentrations, as indicated in the bottom, of S(-) PPX (upper panel) and R(+) PPX (lower panel) for 1 h before being exposed to laser. Mitochondrial ROS generation was evaluated as in figure 2. Data represent means ± SEM of at least three different experiments and are from three separate cell preparations. *, p < 0.05 and **, p < 0.001 vs the corresponding control values (black bars).
Lack of effect of DA receptor antagonists on the inhibition of mitochondrial ROS generation induced by pramipexole (PPX) enantiomers. Cells were exposed to 10 μM S(-) PPX (gray bars) and R(+) PPX (white bars) for 1 h in the absence or presence of 10 μM haloperidol (H) or 10 μM (-) sulpiride (S) before being exposed to laser. Mitochondrial ROS generation was evaluated as in figure 2. Data represent means ± SEM of at least three different experiments and are from three separate cell preparations. *, p < 0.01 vs the corresponding control values (black bars).
Discussion
Pramipexole exists as two stereoisomers. The S(-) enantiomer is a potent D2/D3 receptor agonist and is extensively used in the management of PD. In contrast, the R(+) enantiomer is virtually devoid of any of the DA agonist effects. A growing number of experimental data indicate an antioxidant property of pramipexole enantiomers, evidenced by equal antioxidant efficacy toward H2O2 and nitric oxide [24] and equipotent efficacy in preventing viability impairment induced by H2O2 and mithocondrial ROS generation (present results). We found S(-) and R(+) pramipexole enantiomers relatively weak H2O2 scavengers, with apparent IC50 values in the low micromolar range. Our data are consistent with previous data showing neuroprotection elicited by the S(-) and R(+) enantiomers against different neurotoxic agents [9, 22–27]. In our study, S(-) and R(+) pramipexole enantiomer showed equipotent efficacy suggesting that the neuroprotective effects against H2O2 in differentiated SH-SY5Y neuroblastoma cells were DA receptor independent.
Although this study did not examine the precise site of action of pramipexole, several finding implicate the permeability transition pore (PTP) as a possible target of this drug [19, 24, 25]. Apart from binding to DA receptors, pramipexole has in fact been shown to enter and accumulate in mitochondria driven by the mitochondrial membrane potential [24]. Targeting to mitochondria has also been recently demonstrated by patch clamp studies showing inhibition of PTP by pramipexole [25]. PTP inhibition by pramipexole was further supported by experimental data obtained in functional intact mitochondria showing that this drug abolished Ca++-triggered swelling [25]. By video-rate confocal microscopy in living neuronal cells, we found that both S(-) and R(+) pramipexole enantiomers prevented laser-induced ROS generation in mitochondria of differentiated SH-SY5Y neuronal cells. Interestingly, both pramipexole enantiomers prevented mitochondrial ROS generation with a potency about ten times higher then that elicited for neuroprotection.
The apparent discrepancy between the different potencies of pramipexole enantiomers in preventing mitochondrial ROS generation (about 0.9 μM) and inhibiting H2O2-triggered viability impairment (about 8 μM) may be related to the different experimental models. In fact, H2O2 itself is not a radical but reacts with iron to form hydroxyl radicals, the most reactive oxygen species. Thus, in our experimental paradigm, ROS are generated both intra- and extracellularly and causes apoptosis by the induction of several intracellular converging pathways involving lipid peroxidation, protein oxidation and DNA damage. We hypothesize that accumulation of promipexole enantiomers in the mitochondria [23, 24] may limit their scavenger properties to specific subcellular compartments. Although accumulation of pramipexole into mitochondria has not been definitely established, the high potency of these drugs in preventing mitochondrial ROS generation strongly suggest the mitochondria as their primary site of action.
Conclusions
These results support the concept of both S(-) and R(+) pramipexole enantiomers as mitochondria-targeted antioxidants and suggest that the antioxidant, neuroprotective activity of these drugs is independent of both the chiral 6-propylamino group in the pramipexole molecule and the DA receptor stimulation.
Methods
Cell culture
The human neuroblastoma cell line SH-SY5Y was routinely cultured in Ham's F12 and Dulbecco modified Eagle's medium (DMEM) in a ratio of 1:1, supplemented with 10% (v/v) foetal calf serum, 2 mM glutamine, 50 μg/ml penicillin, and 100 μg/ml streptomycin and kept at 37°C in humidified 5% CO2/95% atmosphere. For differentiation, cultured cells were treated for one week with 10 μM all trans retinoic acid. To obtain reproducible results, SH-SY5Y cells ranging from passage 18 to passage 25 were used for all the experiments.
Drug treatment
S(-) and R(+) pramipexole were dissolved in water and added to the culture media 1 h before H2O2 pulse or laser light stimulation. IC50 values for S(-) and R(+) pramipexole enantiomer were calculated using at least 5 data points. Haloperidol and sulpiride were added to the culture media 1 h before pramipexole. Vitamin E (2 ng/100 μl) was added to the culture media 30 min before the laser excitation. All drugs were from Sigma. S(-) and R(+) pramipexole were kindly supplied by Boehringer Ingelheim GmbH, Germany.
Evaluation of cell viability
Cell viability was measured by quantitative colorimetric assay with MTT (3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyltetrazolium bromide), showing the mitochondrial activity of living cells. Differentiated SH-SY5Y neuronal cells in 96-well plates were challenged with H2O2 for 5 min, then 500 μg/ml MTT was added in each well and cells were incubated at 37°C for additional 3 h. MTT was removed, and cells were lysed with dimethyl sulfoxide. The absorbance at 595 nm was measured using a Bio-Rad 3350 microplate reader. Control cells were treated in the same way without H2O2, and the values of different absorbances were expressed as a percentage of control. All the drugs and reagents concentrations are to be considered as final concentrations.
Reactive oxygen species detection
SH-SY5Y neuroblastoma cells were first differentiated in neuronal-like phenotype by treatment with retinoic acid for 7 days; then, according to Koopman et al. [28], cells were loaded with 5-choloromethyl-2',7'-dichlorodihydrofluorescein (CM-H2DCF) and its oxidative conversion into CM-DCF was monitored by video-rate confocal microscopy and real-time image averaging after increasing laser intensities. For mitochondria localization, cells were also loaded with Mitotracker Deep Red. Cells were then excited at increasing laser intensity and CM-DCF fluorescence intensity was selectively recorded in mitochondria. Fluorescence emission intensity was calculated as average grey level value per pixel and corrected for background.
Statistical evaluation
Results were given as mean ± standard error mean values. Statistical significance of differences was determined by one way ANOVA, followed by Bonferroni's multiple comparison test as post-hoc analysis. A probability of less than 0.05 was considered as a significant difference.
References
Davie CA: A review of Parkinson's disease. Br Med Bull. 2008, 86: 109-127. 10.1093/bmb/ldn013.
McKeith IG, Mosimann UP: Dementia with Lewy bodies and Parkinson's disease. Parkinsonism and Related Disorders. 2004, 10: S15-S18. 10.1016/j.parkreldis.2003.12.005.
Adams JD, Odunze IN: Oxygen free radicals and Parkinson's disease. Free Radic Biol Med. 1991, 10: 161-169. 10.1016/0891-5849(91)90009-R.
Olanow CW: A radical hypothesis for neurodegeneration. Trends Neurosci. 1993, 16: 439-444. 10.1016/0166-2236(93)90070-3.
Schapira AH: Neuroprotection in PD - a role for dopamine agonists?. Neurology. 2003, 61: S34-S42.
Jenner P: Dopamine agonists, receptor selectivity and dyskinesia induction in Parkinson's disease. Curr Opin Neurol. 2003, 16: S3-S7. 10.1097/00019052-200312001-00002.
Ferrari-Toninelli G, Bonini SA, Cenini G, Maccarinelli G, Grilli M, Uberti D, Memo M: Dopamine receptor agonists for protection and repair in Parkinson's disease. Curr Top Med Chem. 2008, 8: 1089-1099. 10.2174/156802608785161402.
Radad K, Gille G, Rausch WD: Short review on dopamine agonists: insight into clinical and research studies relevant to Parkinson's disease. Pharmacol Rep. 2005, 57 (6): 701-712.
Gassen M, Glinka Y, Pinchasi B, Youdim MB: Apomorphine is a highly potent free radical scavenger in rat brain mitochondrial fraction. Eur J Pharmacol. 1996, 308 (2): 219-225. 10.1016/0014-2999(96)00291-9.
Kondo T, Ito T, Sugita Y: Bromocriptine scavenges methamphetamine-induced hydroxyl radicals and attenuates dopamine depletion in mouse striatum. Ann NY Acad Sci. 1994, 738: 222-229.
Ogawa N, Tanaka K, Asanuma M, Kawai M, Masumizu T, Kohno M, Mori A: Bromocriptine protects mice against 6-hydroxydopamine and scavenges hydroxyl free radicals in vitro. Brain Res. 1994, 657: 207-213. 10.1016/0006-8993(94)90969-5.
Takashima H, Tsujihata M, Kishikawa M, Freed WJ: Bromocriptine protects dopaminergic neurons from levodopa-induced toxicity by stimulating D(2)receptors. Exp Neurol. 1999, 159: 98-104. 10.1006/exnr.1999.7122.
Ferger B, Teismann P, Mierau J: The dopamine agonist pramipexole scavenges hydroxyl free radicals induced by striatal application of 6-hydroxydopamine in rats: an in vivo microdialysis study. Brain Res. 2000, 883: 216-223. 10.1016/S0006-8993(00)02929-2.
Uberti D, Carsana T, Francisconi S, Ferrari-Toninelli G, Canonico PL, Memo M: A novel mechanism for pergolide-induced neuroprotection: inhibition of NF-kappaB nuclear translocation. Biochem Pharmacol. 2004, 67: 1743-1750. 10.1016/j.bcp.2004.01.012.
Iida M, Miyazaki I, Tanaka K, Kabuto H, Iwata-Ichikawa E, Ogawa N: Dopamine D2 receptor-mediated antioxidant and neuroprotective effects of ropinirole, a dopamine agonist. Brain Res. 1999, 838: 51-59. 10.1016/S0006-8993(99)01688-1.
Tanaka K, Miyazaki I, Fujita N, Haque ME, Asanuma M, Ogawa N: Molecular mechanism in activation of glutathione system by ropinirole, a selective dopamine D2 agonist. Neurochem Res. 2001, 26: 31-36. 10.1023/A:1007672414239.
Uberti D, Bianchi I, Olivari L, Ferrari-Toninelli G, Bonini SA, Memo M: Dopaminergic agonists: possibile neurorescue drugs endowed with independent and synergistic multisites of action. Neurochem Res. 2007, 32: 1726-1729. 10.1007/s11064-007-9350-9.
Le WD, Jankovic J, Xie W, Appel SH: Antioxidant property of pramipexole independent of dopamine receptor activation in neuroprotection. J Neural Transm. 2000, 107: 1165-73. 10.1007/s007020070030.
Abramova NA, Cassarino DS, Khan SM, Painter TW, Bennett JP: Inhibition by R(+) or S(-) pramipexole of caspase activation and cell death induced by methylpyridinium ion or beta amyloid peptide in SH-SY5Y neuroblastoma. J Neurosci Res. 2002, 67: 494-500. 10.1002/jnr.10127.
Fujita Y, Izawa Y, Ali N, Kanematsu Y, Tsuchiya K, Hamano S, Tamaki T, Yoshizumi M: Pramipexole protects against H2O2-induced PC12 cell death. Naunyn Schmiedebergs Arch Pharmacol. 2006, 372: 257-66. 10.1007/s00210-005-0025-2.
Iravani MM, Sadeghian M, Leung CC, Tel BC, Rose S, Shapira AH, Jenner P: Continuous subcutaneous infusion of pramipexole protects against lipopolysaccharide-induced dopaminergic cell death without affecting the inflammatory response. Exp Neurol. 2008, 212: 522-531. 10.1016/j.expneurol.2008.04.037.
Uberti D, Bianchi I, Olivari L, Ferrari-Toninelli G, Canonico P, Memo M: Pramipexole prevents neurotoxicity induced by oligomers of beta-amyloid. Eur J Pharmacol. 2007, 569 (3): 194-196. 10.1016/j.ejphar.2007.05.009.
Cassarino DS, Fall CP, Smith TS, Bennett JP: Pramipexole reduces reactive oxygen species production in vivo and in vitro and inhibits the mitochondrial permeability transition produced by the parkinsonian neurotoxin methylpyridinium ion. J Neurochem. 1998, 71: 295-301.
Danzeisen R, Schwalenstoecker B, Gillardon F, Buerger E, Krzykalla V, Klinder K, Schild L, Hengerer B, Ludolph AC, Dorner-Ciossek C, Kussmaul L: Targeted antioxidant and neuroprotective properties of the dopamine agonist pramipexole and ist nondopaminergic enantiomer SND919CL2x [(+)2-amino-4,5,6,7-tetrahydro-6-L-propylamino-benzathiazole Dihydrochloride]. J Pharmacol Exp Ther. 2006, 316: 189-199. 10.1124/jpet.105.092312.
Sayeed I, Parvez S, Winkler-Stuck K, Seitz G, Trieu I, Wallesch CW, Schönfeld P, Siemen D: Patch clamp reveals powerful blockade of the mitochondrial permeability transition pore by the D2-receptor agonist pramipexole. FASEB J. 2006, 20 (3): 556-8.
Gribkoff VK, Bozik ME: KNS-760704 [(6R)-4,5,6,7-tetrahydro-N6-propyl-2, 6-benzohiazole-diamine dihydrochloride monohydrate] for the treatment of Amyotrphic Lateral Sclerosis. CNS Neuroscience & Ther. 2008, 14: 215-226. 10.1111/j.1755-5949.2008.00048.x.
Gu M, Iravani M, Cooper JM, Jenner P, Shapira AHV: Pramipexole protects against apoptotic cell death by non-dopaminergic mechanisms. J Neurochem. 2004, 91: 1075-1081. 10.1111/j.1471-4159.2004.02804.x.
Koopman WJH, Verkaart S, van Emst-de Vries SE, Grefte S, Smeitink JAM, Willems PHGM: Simultaneous quantification of oxidative stress and cell spreading using 5-(and 6-)-chloromethyl-2'-7'-dichlorofluorescein. Cytometry Part A. 2006, 69A: 1184-1192. 10.1002/cyto.a.20348.
Gomes A, Fernandes E, Lima JLFC: Fluorescence probes used for detection of reactive oxygen species. J Biochem Biophys Methods. 2005, 65: 45-80. 10.1016/j.jbbm.2005.10.003.
Swift LM, Sarvazyan N: Localization of dichlorofluorescein in cardiac myocytes: Implications for assessment of oxidative stress. Am J Physiol Heart Circ Physiol. 2000, 278: H982-H990.
Acknowledgements
This research was supported in part by a grant from Boehringer Igelheim.
Author information
Authors and Affiliations
Corresponding author
Additional information
Authors' contributions
GFT, GM and DU conducted and managed the study and analyzed the imaging data, MM drafted the manuscript. EB and MM participated in the design and coordination of the project. All authors cooperatively designed the project and discussed data interpretation. All authors participated in critical editing of the manuscript.
Authors’ original submitted files for images
Below are the links to the authors’ original submitted files for images.
Rights and permissions
Open Access This article is published under license to BioMed Central Ltd. This is an Open Access article is distributed under the terms of the Creative Commons Attribution License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Ferrari-Toninelli, G., Maccarinelli, G., Uberti, D. et al. Mitochondria-targeted antioxidant effects of S(-) and R(+) pramipexole. BMC Pharmacol 10, 2 (2010). https://doi.org/10.1186/1471-2210-10-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/1471-2210-10-2