Abstract
Background
Rheumatoid arthritis is a chronic disabling autoimmune disease with predilection to synovial joints and many extraarticular manifestations. Disease-modifying anti-rheumatic drugs are the cornerstone and initial therapy in rheumatoid arthritis. Although medication adherence is crucial for successful therapy, non-adherence is a substantial problem in some. This study aimed to determine the adherence rate of treatment with disease-modifying anti-rheumatic drugs among patients with rheumatoid arthritis in an Egyptian university hospital. In this study, seventy-three adult rheumatoid arthritis patients who are on disease-modifying anti-rheumatic drugs treatment for at least 6 months were included in this study. After full history and clinical examination, assessment of the adherence rate to disease-modifying anti-rheumatic drugs was done using the Clinician Rating Scale. Measuring the quality of life using the Health Assessment Questionnaire Disability Index and screening for depression and anxiety using the Hospital Anxiety and Depression Scale were done. The socio-economic level of the patients was assessed by socio-economic status scale.
Results
In the current study, 65.1% of the patients were highly adherent to their disease-modifying anti-rheumatic drug (DMARD) medications, while 26% showed middle level of adherence. There was a significant difference between medication adherence and anxiety, but not with other demographic data, clinical data, disease activity, or socio-economic level.
Conclusion
In this study, no significant difference was found between medication adherence and demographic, clinical, or socio-economic data. However, anxiety was significantly related to DMARD adherence in the studied group. Age and HAQ-DI were found to be strong predictors to medication adherence in our RA patients. Further studies should be conducted on a large number of patients with rheumatoid arthritis to become generalizable to a broader population.
Similar content being viewed by others
Background
Rheumatoid arthritis (RA) is a chronic progressive autoimmune disease that causes inflammation and destruction of synovial joints. It has a strong impact on people’s everyday lives. Patients with RA suffer from pain, limited mobility, and disability besides experiencing a decreased quality of life [1].
Despite the great advances in the treatment of RA with biological therapy, disease-modifying anti-rheumatic drugs (DMARDs) remain the cornerstone and initial therapy in this disease [2]. These drugs have shown to retard disease progression including joint destruction.
Early application of DMARDs has revealed significant benefit when compared with their use later in the course of the disease although even early DMARD therapy does not fully prevent disease progression in the majority of the patients [3].
It is believed that adherence to treatment is crucial for successful therapy; however, non-adherence is a substantial problem in patients with chronic rheumatic conditions, including RA [4].
Medication adherence refers to the patient’s act of conforming to the recommendations made by health care providers with respect to timing, dosage, and frequency of medication-taking [5].
Medication adherence can be divided into three major components: (a) initiation when the patient takes the first dose of a prescribed medication, (b) persistence defined as the length of time a patient fills prescriptions without permissible gaps, and (c) execution adherence defined as the extent to which a patient’s actual dosing corresponds to the prescribed dosing regimen, from initiation until the last dose is taken [6].
Adherence to treatment improves the outcome and affects several widely used indices [Disease Activity Score (DAS28) and Clinical Disease Activity Index (CDAI)] [7].
Previous studies have reported that DMARD non-adherence results in more disease activity, loss of function, and a lower quality of life [8, 9].
Method
Aim of the study
The study aimed to determine the adherence rate of treatment with DMARDs among patients with RA.
Study design
This observational clinical study was conducted in the outpatient clinic of the Rheumatology and Rehabilitation Department at our University Hospital. Seventy-three adult RA patients (68 females and 5 males) who fulfilled the 2010 ACR/EULAR classification criteria for RA [10] and selected by quota sample were included in the study. The researchers started to collect data from January to June 2019; each interview took 20–30 min.
Inclusion criteria
This study included RA patients aged ≥ 18 years, on current treatment with one or more of DMARDs of at least 6 months duration and with cognitive level enabling them to interact actively in the study. Patients with other rheumatic diseases, end-stage organ failure, and cognitive impairment were excluded from the study.
Ethical considerations
This study has been approved by the local ethics committee of our Faculty of Medicine and conforms to the guidelines of the Declaration of Helsinki. Clinical trial registration number of the study is NCT03316027. Written consent was obtained from each studied subject.
Process
Full history and clinical examination of all patients were done with calculation of the disease activity using DAS-28 ESR scoring [11, 12]. A DAS-28 of greater than 5.1 = high active disease, 3.2 to 5.1 = moderate activity, 2.6 to 3.2 = low activity, and less than 2.6 = remission.
All patients were reviewed for completing 4 standardized interview-questionnaires as follows:
-
1.
Clinician Rating Scale (CRS)
It is an ordinal scale of 1–7 to quantify the clinician’s assessment of the level of adherence shown by the patient. Higher numbers represent greater adherence [13, 14].
-
2.
Health Assessment Questionnaire Disability Index (HAQ-DI)
Functional disability was evaluated by the HAQ-DI, which included 20 questions in 8 sub-dimensions: dressing and grooming, arising, eating, walking, hygiene, reach, grip, and common daily activities. The response alternatives were 0 grade, able without any difficulty; 1 grade, able with some difficulty; 2 grades, able with much difficulty; and 3 grades, unable.Scoring system: The 8 scores of the 8 sub-dimensions are summed and divided by 8. In the event that one sub-dimension is not completed by a subject, the summed score would be divided by 7. The HAQ-DI score is not calculated when the patient provides answers in fewer than six sub-dimensions. The HAQ-DI score ranged from 0 to 3, with higher scores indicating more disability. Functional disability was defined as the HAQ-DI score ≥ 1 according to a previous study [15].
-
3.
Hospital Anxiety and Depression Scale (HADS)
A 14-item questionnaire was used to detect anxiety (7 items) and depression (7 items). Each item had a 4-point Likert scale and was scored between 0 and 3 grades, e.g., “I can sit at ease and feel relaxed ", with responses of 0 = definitely, 1 = usually, 2 = not often, and 3 = not at all; each sub-scale was constructed by summation.Scoring system: The HADS ranged from 0 to 21, a score between 0 and 7 suggests “no case,” 8 to 10 represent a “borderline case,” and 11 to 21 indicate a “case of anxiety/depression.” These cutoff points have been validated against clinical interviews with sensitivity and specificity approximately 0.80. Recent studies have reported good internal consistency for both anxiety (0.89) and depression (0.86) sub-scales [16, 17]. The Arabic version of the questionnaire was used [18].
-
4.
Socio-economic status scale
Designed by Abd-El-Tawab [19] to assess socio-economic status of the family and included the following:
-
(a)
Personal characteristics of the patients such as age, sex, residence, and marital status
-
(b)
Patient’s and his wife/her husband level of education
-
(c)
Patient’s and his wife/her husband occupation
-
(d)
Total family monthly income
-
(e)
Lifestyle of the family
Scoring system: The scores for these items were fed into a mathematical formula to produce the socio-economic score. The total score was divided into 3 scales as high, moderate, and low [20].
Validity and reliability
The evaluation of data collection tools was done by three experts from the Rheumatology and Rehabilitation Department at our University Hospital to measure the validity of the tools. Reliability was analyzed by Cronbach’s alpha the value was 0.87.
Methods of data collection
A pilot was carried out before starting data collection on 10% (7 patients) who excluded from sample. It is aimed to test the clarity of tools and to estimate the time required to fill questionnaires. The necessary modification was done according to result of pilot study.
Statistical analysis
Date entry and data analysis were done using Statistical Package for Social Science (SPSS) version 20. Data were presented as number, percentage, mean, and standard deviation. Also, Kruskal-Wallis test was used for comparing the differences between more than 2 groups. Multivariate linear regression modeling was used for prediction studying. P value was considered statistically significant when P < 0.05.
Results
The vast majority (93.2%) of patients were females and less than one third of them (31.5%) had age ranged from 50 to < 60 years old. Most of the studied patients were from rural areas and they were housewives (90.4%) for both. While (71.2%) of them were married and most of them (84.9%) were illiterate (Table 1)
It was clear that 82.19% of patients received hydroxychloroquine as a current medication followed by 61.64% who received leflunomide, while only 15.06% of patients received sulphasalazine. Fifty-four patients received combined DMARDS and none of the study patients received biologic treatment. It was found that 41.1% of studied patients had disease duration of less than 10 years and 46.6% of them had treatment duration of less than 10 years (Table 2).
Table 3 describes the Clinician Rating Scale (CRS) among studied patients. About one quarter of patients (24.7%) partially refused or only accepted minimum dose, while 13.7% of patients were occasionally reluctant and 20.5% of them were active participants and showed some responsibility for regimen following.
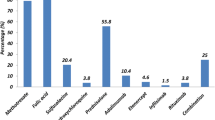
Figure 1 illustrates the medication adherence level among studied patients. We considered that the first two statements of the CRS were indicators of low adherence, the next 2 statements were denoting middle-level adherence, while the last 3 statements as indicators of high-level adherence. Depending on this assumption, it was observed that 42.5% of patients had a high level of adherence, while 31.5% of them had a low level, and 26.0% of them had middle level.
The clinical data of the studied patients are shown in Table 4 where 45.2% of the patients had moderate disease activity while 26.0% of them had high disease activity. Only 8.2% were in remission. As regards the health assessment of disability index level among studied patients, it was clear that 47.9% of patients had mild level of disability (0–< 1) and 27.4% of them had severe level (2–3), while 24.7% of them had moderate (1–< 2) level with mean ± SD (1.28 ± 0.98). Depression was found in 31.5% of cases, while borderline depression was found in 19.2% of patients. On the other hand, 21.9% of the patients had anxiety and 16.4% were having borderline anxiety.
Table 5 showed no statistically significant relation between medication adherence level and demographic characteristics, clinical data, HAQ-DI level, DAS-28 level depression, and socio-economic class among studied patients. However, anxiety was significantly related to adherence rate (P = 0.05).
Disease activity was significantly correlated with functional disability index, depression, and anxiety with P value of 0.000, 0.017, and 0.002, respectively, while it showed no significant association with the socio-economic level (not shown in tables).
Table 6 shows the results of the linear regression analysis of some clinical data with the medication adherence. It shows that both the age and HAQ-DI were significant predictors of the medication adherence with P value of 0.024 and 0.43, respectively.
Discussion
Rheumatoid arthritis (RA) is an autoimmune systemic disease that primarily causes inflammation of the synovial joints [21]. If left untreated, chronic inflammation of the joints causes articular destruction and bone erosions, leading to functional disabilities [22].
Disease-modifying anti-rheumatic drugs (DMARDs) remain the first treatment line of RA as they can retard the joint damage and deformities [23].
Noncompliance to the medications leads to poor disease control, increased morbidity, and recurrent hospital admission with consecutive increased utilization of health resources [24,25,26,27,28].
Several interacting factors can influence patients’ non-adherent behavior including disease-related factors, patient-related factors, health professional/health service-related factors, and therapy-related factors [29].
This study aimed for determining adherence rate to DMARDs among sample of Egyptian patients with RA.
In the current study, 42.5% of the studied patients were highly adherent to their DMARDs medications, while 26% were moderately adherent with a sum of 68.5%.
High adherence rate was also reported by Ragab et al. who found that 62.5% of RA patients were adherence DMARDs [30]. On the other hand, Prudente et al. found that (16.4%) of RA patients were adherent to treatment [31]. Suggested explanation of the recorded adherence rate in the current study is the close, monthly follow-up of RA patients in the outpatient clinic. During the follow-up visits, physicians perform medication reconciliation and emphasize the importance of medication adherence and rise patients’ awareness of the destructive nature of rheumatoid arthritis, so they have become keen to adhere to anti-rheumatic drugs to avoid deformities and disabilities. Another factor could be that some of the included patients received their medications through the government-funded public health system while others received it through the health insurance system. Therefore, the medication cost did not have a negative impact on their medication adherence.
In the current study, age seems to lack an influence on treatment adherence in RA patients. Similar results were reported by some investigators [29, 32]. while others found a better adherence rate among older patients than in younger ones [23, 33].
Xia et al. found no statistically significant differences between age, employment, disease duration, and DAS28 score in association with adherence rate, while monthly per capita income was found to have a significant correlation with adherence rate [34]. Moreover, Sharma et al. [35] found that low income and was statistically significant responsible for the non-adherence to the treatment (P < 0.0001) [31]. Other investigators have reported that age and disease duration were associated with medication adherence, and disease activity [36,37,38,39].
In the present study, and in line with several studies, no significant association was found between the disease duration and treatment adherence to anti-rheumatic drugs in RA patients [30, 32, 33]. Moreover, no statistically significant relation could be detected between medication adherence and disease activity expressed as DAS28-ESR and socio-economic class.
In concordance with these findings, Li et al. [40] found no significant difference between medication adherence and disease activity among RA patient [34], and Lorish et al. [41] reported that socio-economic level was not associated with adherence. However, Ragab et al. reported that DAS28 was found to correlate significantly with adherence (P = 0.001) [30].
As regards psychological abnormalities (depression and anxiety) among studied patients, the current study revealed that 31.5% and 21.9% of patients had depression and anxiety, respectively.
Zhang et al. found that 27.5% and 30.6% of his RA patients had depression and anxiety, respectively [42], whereas Xia et al. found higher percentage of depression and anxiety in RA patients (69% and 70%, respectively) [34].
A possible explanation of the low prevalence of depression/anxiety among studied patients could be attributed to the religious background that Egyptian patients have in the face of their illness, it can be also explained by the emotional support of the patients’ partners and families as most of the patients are married. Although several studies had reported the negative effect of depression on medication adherence [43,44,45], in this study, a statistically significant relation was found between medication adherence and anxiety (P = 0.05) but not with depression.
Although no significant relation was found between the demographic and clinical data in this study with the medication adherence, regression analysis was done between some of these data which was found to have significant impact on the medication adherence in previous literatures [46,47,48].
A large number of factors have been reported to influence medication adherence in RA patients but no consistent non-adherence risk profile was agreed upon by the researchers [49].
In this study, age and HAQ-DI were found to be predictors of medication adherence. This is consistent with the results reported by Cohen et al. who reported that older patients were more adherent to their medications. This could be explained by the relative more time the older people have to take care of their health, the relative more cooperation and interaction with the healthcare system, following with the physician appointments, and better belief in the importance of proper disease management [50]. Similar finding was reported by Park et al. [23].
We found that HAQ-DI was a significant predictor of medication adherence. Likewise, Hromadkova reported low drug compliance in patients with good QOL. A possible explanation is that low QOL may trigger the patient’s attention towards his health care system including compliance to clinic appointment and medication regimen [51].
We found non-significant influence of other factors like anxiety, disease duration, educational level, co-morbidities, and marital status on the medication adherence. This may be due to the small sample size (n = 73) and the multiple variables entered into the model that has reduced the statistical power.
Conclusion
Based on the results of the current study, it was concluded that more than two thirds of the studied patients had moderate to high adherence rate to their DMARDs medications and there is no statistically significant difference between medication adherence and demographic, clinical, or socio-economic data, while there is a significant relation between anxiety and medication adherence. Age and HAQ-DI were found to be strong predictors to medication adherence in our RA patients.
Recommendations
The current study recommended that the rheumatologist should build an open and trustworthy relationship with the patient, in which non-adherence can be openly discussed. When the rheumatologist has a trusting relation with the patient, they will be able to know if non-adherence is hampering the treatment goal. The effect of cumulative doses of corticosteroids on the psychological status of the patients should be considered. Investigation of other factors that could influence the medication adherence in different age groups such as the polypharmacy and nonintentional lack of adherence due to cognitive causes in elderly patients and drug availability and patients’ knowledge about the medication should be considered in future studies.
Lastly, further studies on a larger number of patients with rheumatoid arthritis are recommended to improve the statistical power, so that the results would be generalizable to a broader population.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- RA:
-
Rheumatoid arthritis
- DMARDs:
-
Disease-modifying anti-rheumatic drugs
- DAS28:
-
Disease Activity Score
- CDAI:
-
Clinical Disease Activity Index
- CRS:
-
Clinician Rating Scale
- HAQ-DI:
-
Health Assessment Questionnaire Disability Index
- HADS:
-
Hospital Anxiety and Depression Scale
- SPSS:
-
Statistical Package for Social Science
References
Matcham F, Scott I, Rayner L, Hotopf M, Kingsley G, Norton S, et al., editors (2014) King’s research portal. Semin Arthritis Rheum
Waimann CA, Marengo MF, de Achaval S, Cox VL, Garcia-Gonzalez A, Reveille JD et al (2013) Electronic monitoring of oral therapies in ethnically diverse and economically disadvantaged patients with rheumatoid arthritis: consequences of low adherence. Arthritis Rheum 65(6):1421–1429
Nell V, Machold K, Eberl G, Stamm T, Uffmann M, Smolen J (2004) Benefit of very early referral and very early therapy with disease-modifying anti-rheumatic drugs in patients with early rheumatoid arthritis. Rheumatology 43(7):906–914
Harrold LR, Andrade SE (eds) (2009) Medication adherence of patients with selected rheumatic conditions: a systematic review of the literature. Seminars in arthritis and rheumatism. Elsevier
Sabaté E (2017) Adherence to long-term therapies: evidence for action. World Health Organization 2003 WHO/MNC/03.01, Geneva
Vrijens B, De Geest S, Hughes DA, Przemyslaw K, Demonceau J, Ruppar T et al (2012) A new taxonomy for describing and defining adherence to medications. Br J Clin Pharmacol 73(5):691–705
Tanwar VS, Singh H, Saini A, Sukhija G, Arora S, Kalra A (2019) Rheumatoid Arthritis Disease Activity Index-5: an easy and effective way of monitoring patients with rheumatoid arthritis. Egypt Rheumatol Rehabil 46(4):269
Contreras-Yáñez I, Cabiedes J, Rull-Gabayet M, Pascual-Ramos V, De León SP (2010) Inadequate therapy behavior is associated to disease flares in patients with rheumatoid arthritis who have achieved remission with disease-modifying antirheumatic drugs. Am J Med Sci 340(4):282–290
Van den Bemt B (2009) Optimizing pharmacotherapy in patients with rheumatoid arthritis. An Individualized Approac https://repository.ubn.ru.nl/bitstream/handle/2066/81554/81554.pdf?sequence=1 Accessed 21 Mar 2020.
Aletaha D, Neogi T, Silman AJ, Funovits J, Felson DT, Bingham CO III et al (2010) 2010 rheumatoid arthritis classification criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum 62(9):2569–2581
Prevoo M, Van'T Hof MA, Kuper H, Van Leeuwen M, Van De Putte L, Van Riel P (1995) Modified disease activity scores that include twenty-eight-joint counts development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthr Rheum 38(1):44–48
Wells G, Becker J, Teng J, Dougados M, Schiff M, Smolen J et al (2009) Validation of the 28-joint Disease Activity Score (DAS28) and European League Against Rheumatism response criteria based on C-reactive protein against disease progression in patients with rheumatoid arthritis, and comparison with the DAS28 based on erythrocyte sedimentation rate. Ann Rheum Dis 68(6):954–960
Kemp R, Hayward P, Applewhaite G, Everitt B, David A (1996) Compliance therapy in psychotic patients: randomised controlled trial. BMJ 312(7027):345–349
Kemp R, Kirov G, Everitt B, Hayward P, David A (1998) Randomised controlled trial of compliance therapy. 18-month follow-up. Br J Psychiatry 172:413–419
Bruce B, Fries JF (2003) The Stanford Health Assessment Questionnaire: a review of its history, issues, progress, and documentation. J Rheumatol 30(1):167–178
Zigmond AS, Snaith RP (1983) The Hospital Anxiety and Depression Scale. Acta Psychiatr Scand 67(6):361–370
Olssøn I, Mykletun A, Dahl AA (2005) The Hospital Anxiety and Depression Rating Scale: a cross-sectional study of psychometrics and case finding abilities in general practice. BMC Psychiatry 5(1):46
Terkawi AS, Tsang S, AlKahtani GJ, Al-Mousa SH, Al Musaed S, AlZoraigi US et al (2017) Development and validation of Arabic version of the Hospital Anxiety and Depression Scale. Saudi J Anaesth 11(Suppl 1):S11–S18. https://doi.org/10.4103/sja.SJA_43_17
Tawab A (2004)Socioeconomic Scale to Assess Socioeconomic Status of the Family. Faculty of Education, Assiut University.
Darweesh AEDM, Mohamed NAEM, Marzouk HK (2013) Psychological assessment of patients with myocardial infarction. Life Sci J 10(1):651–662
Smolen J, Aletaha D, McInnes I (2016) Rheumatoid arthritis 388, pg 2023. Lancet.
Bondt A, Hafkenscheid L, Falck D, Kuijper TM, Rombouts Y, Hazes JM et al (2018) ACPA IgG galactosylation associates with disease activity in pregnant patients with rheumatoid arthritis. Ann Rheum Dis 77(8):1130–1136
Park DC, Hertzog C, Leventhal H, Morrell RW, Leventhal E, Birchmore D et al (1999) Medication adherence in rheumatoid arthritis patients: older is wiser. J Am Geriatr Soc 47(2):172–183
DiMatteo MR, Giordani PJ, Lepper HS, Croghan TW (2002) Patient adherence and medical treatment outcomes a meta-analysis. Med Care 40(9):794–811
McDonnell PJ, Jacobs MR (2002) Hospital admissions resulting from preventable adverse drug reactions. Ann Pharmacother 36(9):1331–1336
Sokol MC, McGuigan KA, Verbrugge RR, Epstein RS (2005) Impact of medication adherence on hospitalization risk and healthcare cost. Med Care 43(6):521–530
Schiff GD, Fung S, Speroff T, McNutt RA (2003) Decompensated heart failure: symptoms, patterns of onset, and contributing factors. Am J Med 114(8):625–630
Jha AK, Aubert RE, Yao J, Teagarden JR, Epstein RS (2012) Greater adherence to diabetes drugs is linked to less hospital use and could save nearly $5 billion annually. Health Aff 31(8):1836–1846
Pasma A, vant Spijker A, Hazes JMW, Busschbach JJV, Luime JJ (2013) Factors associated with adherence to pharmaceutical treatment for rheumatoid arthritis patients: a systematic review. Semin Arthritis Rheum 43:18–28
Ragab OM, Zayed HS, Abdelaleem EA, Girgis AE (2017) Effect of early treatment with disease-modifying anti-rheumatic drugs and treatment adherence on disease outcome in rheumatoid arthritis patients. Egypt Rheumatol 39(2):69–74
Prudente LR, de Souza DJ, Ferreira TXAM, Lima DM, Silva NA, Saraiva G et al (2016) Medication adherence in patients in treatment for rheumatoid arthritis and systemic lupus erythematosus in a university hospital in Brazil. Patient Pref Adher 10:863–870
Müller R, Kallikorm R, Põlluste K, Lember M (2012) Compliance with treatment of rheumatoid arthritis. Rheumatol Int 32(10):3131–3135
Tuncay R, Eksioglu E, Cakir B, Gurcay E, Cakci A (2007) Factors affecting drug treatment compliance in patients with rheumatoid arthritis. Rheumatol Int 27(8):743–746
Xia Y, Yin R, Fu T, Zhang L, Zhang Q, Guo G et al (2016) Treatment adherence to disease-modifying antirheumatic drugs in Chinese patients with rheumatoid arthritis. Patient Pref Adher 10:735–742
Sharma S, Roshi VRT, Mahajan A (2015) A study evaluating adherence and compliance of anti-rheumatic drugs in women suffering from rheumatoid arthritis. J Clin Diagn Res 9(11):OC01
Curkendall S, Patel V, Gleeson M, Campbell R, Zagari M, Dubois R (2008) Compliance with biologic therapies for rheumatoid arthritis: do patient out-of-pocket payments matter? Arthritis Care Res 59(10):1519–1526
Garcia-Gonzalez A, Richardson M, Popa-Lisseanu MG, Cox V, Kallen MA, Janssen N et al (2008) Treatment adherence in patients with rheumatoid arthritis and systemic lupus erythematosus. Clin Rheumatol 27(7):883–889
Rauscher V, Englbrecht M, van der Heijde D, Schett G, Hueber AJ (2015) High degree of nonadherence to disease-modifying antirheumatic drugs in patients with rheumatoid arthritis. J Rheumatol 42(3):386–390
Bliddal H, Eriksen SA, Christensen R, Lorenzen T, Hansen MS, Østergaard M et al (2015) Adherence to methotrexate in rheumatoid arthritis: a Danish nationwide cohort study. Arthritis. 2015 https://doi.org/10.1155/2015/915142
Li L, Cui Y, Yin R, Chen S, Zhao Q, Chen H, et al (2017) Medication adherence has an impact on disease activity in rheumatoid arthritis: a systematic review and meta-analysis. Patient Prefer Adherence 11:1343
Lorish CD, Richards B, Brown S (1989) Missed medication doses in rheumatic arthritis patients: intentional and unintentional reasons. Arthritis Rheum 2(1):3–9
Zhang L, Xia Y, Zhang Q, Fu T, Yin R, Guo G et al (2017) The correlations of socioeconomic status, disease activity, quality of life, and depression/anxiety in Chinese patients with rheumatoid arthritis. Psychol Health Med 22(1):28–36
Julian LJ, Yelin E, Yazdany J, Panopalis P, Trupin L, Criswell LA et al (2009) Depression, medication adherence, and service utilization in systemic lupus erythematosus. Arthritis Care Res 61(2):240–246
JWG J, Silva J (2015) Psychological factors associated with response to treatment in rheumatoid arthritis. Curr Pharm Des 21(2):257–269
Cabrera-Marroquin R, Contreras-Yáñez I, Alcocer-Castillejos N, Pascual-Ramos V (2014) Major depressive episodes are associated with poor concordance with therapy in rheumatoid arthritis patients: the impact on disease outcomes. Clin Exp Rheumatol 32(6):904–913
Hope HF, Hyrich KL, Anderson J, Bluett J, Sergeant JC, Barton A et al (2020) The predictors of and reasons for non-adherence in an observational cohort of patients with rheumatoid arthritis commencing methotrexate. Rheumatology 59(1):213–223
Salt E, Frazier SK (2011) Predictors of medication adherence in patients with rheumatoid arthritis. Drug Dev Res 72(8):756–763
Smolen JS, Gladman D, McNeil HP, Mease PJ, Sieper J, Hojnik M et al (2019) Predicting adherence to therapy in rheumatoid arthritis, psoriatic arthritis or ankylosing spondylitis: a large cross-sectional study. RMD Open 5:e000585. https://doi.org/10.1136/rmdopen-2017-000585
Van Den Bemt BJ, Zwikker HE, Van Den Ende CH, Horne O, Haynes et al (2012) Medication adherence in patients with rheumatoid arthritis: a critical appraisal of the existing literature. Expert Rev Clin Immunol 8(4):337–351
Cohen MJ, Shaykevich S, Cawthon C, Kripalani S, Paasche-Orlow MK, Schnipper JL (2012) Predictors of medication adherence postdischarge: the impact of patient age, insurance status, and prior adherence. J Hosp Med 7(6):470–475
Hromadkova L, Soukup T, Vlcek J (2015) Quality of life and drug compliance: their interrelationship in rheumatic patients. J Eval Clin Pract 21(5):919–924
Acknowledgements
Not applicable
Funding
No funding from external organization or body was needed.
Author information
Authors and Affiliations
Contributions
SM: Conception and design, critical revision of the submitted protocol for important intellectual content, and writing the manuscript. TK: Administrative, technical or material support, and supervision. EM: Acquisition of data, analysis and interpretation of data, and statistical analysis. EE: Drafting of the submitted protocol and critical revision of the submitted protocol for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study has been approved by the local ethics committee of the Faculty of Medicine and conforms to the guidelines of the Declaration of Helsinki. Date of approval, 19 November 2017
Clinical trial registration number of the study is NCT03728231.
All studied subjects gave written consent to participate in the study.
Consent for publication
Not applicable
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
This article is published under an open access license. Please check the 'Copyright Information' section either on this page or in the PDF for details of this license and what re-use is permitted. If your intended use exceeds what is permitted by the license or if you are unable to locate the licence and re-use information, please contact the Rights and Permissions team.
About this article
Cite this article
Mahran, S.A., Khedr, T.M., Mohammed, E.M. et al. Medication adherence to disease-modifying anti-rheumatic drugs among patients with rheumatoid arthritis at Assiut University Hospital, Egypt. Egypt Rheumatol Rehabil 47, 3 (2020). https://doi.org/10.1186/s43166-020-00005-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s43166-020-00005-6