Abstract
Purpose
TNM Stage 3B encompasses a wide range of primary tumor and nodal metastatic tumor burden. This study aimed to evaluate the prognostic value of quantitative FDG PET/CT parameters in patients with newly diagnosed Stage 3B Non-Small Cell Lung Cancer (NSCLC).
Materials and Methods
Institutional review board approved retrospective study identified patients diagnosed with Stage 3B NSCLC (8th edition TNM classification) on baseline FDG PET/CT at two medical centers (Medical centers A and B), between Feb 2004 and Dec 2014. Patients were excluded if they had prior NSCLC treatment or recent diagnosis of a second primary cancer. Quantitative FDG PET/CT parameters including whole body metabolic tumor volume (MTVwb), total lesion glycolysis (TLGwb), and maximum standardized uptake value (SUVmaxwb) were measured from baseline PET/CT using Edge method with Mimvista software. The primary endpoint was overall survival (OS). Cox proportional hazard regression and Kaplan-Meier overall survival analyses were used to test for an association between OS and quantitative FDG PET/CT parameters. The distributions of MTVwb, TLGwb, SUVmaxwb were skewed, so a natural logarithm transformation was applied and the transformed variables [(ln(MTVwb), ln(TLGwb), and ln(SUVmaxwb)] were used in the analysis.
Results
The training set included 110 patients from center A with Stage 3B NSCLC. 78.2% of patients expired during follow-up. Median OS was 14 months. 1-year, 2-year, and 5-year OS was 56.5%, 34.6% and 13.9%, respectively. Univariate Cox regression analysis showed no significant difference in OS on the basis of age, gender, histology, ln(TLGwb), or ln(SUVmaxwb). ln(MTVwb) was positively associated with OS [hazard ratio (HR) of 1.23, p = 0.037]. This association persisted on multivariate Cox regression analysis (HR 1.28, p = 0.043), with adjustments for age, gender, treatment and tumor histology. External validation with 44 patients from center B confirmed increasing MTVwb was associated significantly worse OS. An MTVwb cut-off point of 85.6 mL significantly stratified Stage 3B NSCLC patient prognosis.
Conclusion
MTVwb is a prognostic marker for OS in patients with Stage 3B NSCLC, independent of age, gender, treatment, and tumor histology.
Similar content being viewed by others
Explore related subjects
Find the latest articles, discoveries, and news in related topics.Introduction
Lung cancer is the leading cause of cancer death within the United States (Siegel et al., 2016). The TNM staging system developed by the American Joint Committee on Cancer (AJCC)/Union for International Cancer Control (UICC) is the primary means for classifying patient disease status and predicting patient prognosis, with the most recent 8th edition recently introduced by the International Association for the Study of Lung Cancer (IASLC) (Detterbeck et al., 2016; Asamura et al., 2015; Rami-Porta et al., 2015; Goldstraw et al., 2016). Stage 3B Non-small Cell Lung Cancer (NSCLC) now comprises patients without distant metastases (M0) who have stage T3 or T4 primary disease, with ipsilateral mediastinal and/or subcarinal nodal metastases (N2), as well as patients with T1 or T2 primary disease with metastases in scalene, supraclavicular, contralateral mediastinal or contralateral hilar lymph nodes (N3). In other words, Stage 3B encompasses a wide range of primary tumor burden, including patients with primary tumors ranging from <1 cm (T1a) to ≥7 cm (T4) in greatest dimension and N0 to N3 nodal metastases.
For patients with locally advanced lung cancer, fluorodeoxyglucose (FDG) positron emission tomography/computed tomography (PET/CT) enables detection of CT-occult, metabolically active tumor. Maximum standardized uptake value (SUVmax) is an established measurement of maximal tumor metabolic activity and facilitates identification of tumor metastases, but it fails to take into account total tumor abundance/burden. Quantitative FDG measurements, namely the amount of whole body metabolic tumor volume (MTVwb) and total lesion glycolysis (TLGwb), may be used to quantify both total tumor burden and metabolic activity. These parameters have been found to be associated with OS for both surgical and non-surgical NSCLC patients, after adjusting for clinical stage (Liao et al., 2012a; Zhang et al., 2013a; Zhang et al., 2013b). These PET/CT metrics have yet to be evaluated for Stage 3B NSCLC patients (Ohri et al., 2015).
Patients with Stage 3B NSCLC are rarely surgical candidates due to mediastinal invasion or extensive nodal disease, and are routinely treated with combined radiation and chemotherapy, though options are constantly evolving to cater to a more individualized patient-centered therapeutic approach (Rocco et al., 2016). The overall survival (OS) of Stage 3B NSCLC patients at 2 and 5 years is 44% and 26%, respectively (Goldstraw et al., 2016). If we can identify additional prognostic markers for these patients, we may be able to better stratify Stage 3B NSCLC patients, and determine who is more likely to benefit from more aggressive therapy.
Here we aimed to evaluate the prognostic value of MTVwb, TLGwb, and SUVmaxwb, on baseline FDG PET/CT in patients with Stage 3B NSCLC.
Materials and methods
This Health Insurance Portability and Accountability Act compliant retrospective study received institutional review board approval. The need for informed consent was waived.
Patient cohort
Utilizing a retrospective search of our health information system, patients were included if they met both of the following inclusion criteria: a. diagnosed with Stage 3B NSCLC in accordance with the 8th edition of the TNM classification system; and b. received baseline staging PET/CT between February 2004 and Dec 2014. Patients were excluded if they either: 1. received prior lung cancer treatment, including chemotherapy, radiation, or surgery; or 2. had a second primary cancer diagnosed from 5 years before to 2 months after the FDG PET/CT scan conducted for NSCLC diagnosis and staging. 110 consecutive patients were identified from center A and served as the training set. The external validation set included 44 patients managed and imaged at institution B from 2008 to 2014. These patients received a FDG PET/CT within 3 months of starting radiation therapy.
Patient demographics, clinical information, and follow-up were collected from the health information system. Patients were censored at date of last contact.
PET/CT acquisition
Imaging was performed on a Siemens mCT scanner (Siemens Healthcare, Knoxville, Tenn) or Reveal HD scanner (CTI, Knoxville, Tenn). All patients fasted for a minimum of 4 h prior to imaging, confirmed by fingerstick serum blood glucose levels <200 mg/dl. Patients were injected with 370-555 MBq 18F–FDG. At center A (the training dataset), whole body PET/CT imaging was acquired approximately 90 min later. At center B (the validation dataset), patients were scanned approximately 60 min later. Concomitant low-dose non-contrast or diagnostic CT extending from the skull base to thighs was performed for anatomic localization and attenuation correction.
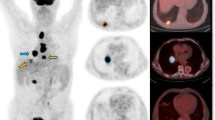
PET/CT tumor volume, SUVmaxwb, MTVwb, and TLGwb were measured using the PET Edge tool of MIMvista software as illustrated in Fig. 1, using semi-automated tumor segmentation, as previously described (Liao et al., 2012a).
Whole-body PET images of a 59 year-old male with newly diagnosed squamous cell carcinoma, stage IIIB (T4N2M0). This study was performed for initial staging. Colored regions of interest (ROIs) show the tumor contours. The MTVwb in mL is the sum of tumor volumes in all ROIs. Axial image (a), sagittal image (b), coronal image (c) and maximal intensity projection image (d)
Briefly, SUVmax for each tumor lesion was defined as: \( \frac{\mathrm{decayed}\ \mathrm{corrected}\ \mathrm{activity}/\mathrm{tissue}\ \mathrm{volume}}{\mathrm{injected}\ \mathrm{dose}/\mathrm{injected}\ \mathrm{weight}} \). SUVmaxwb was taken to be the largest SUVmax among all tumor lesions identified on baseline staging PET/CT. MTVwb was defined as the total segmented volume of all FDG-avid tumors in the body. TLG for a single tumor lesion is the product of MTV and the average SUV for the lesion. TLGwb was calculated as the sum of the TLGs of all segmented tumor.
Statistical analysis
Statistical analyses were performed using Stata Software version 14. OS was considered the primary endpoint and defined as the time from baseline PET/CT to time of any cause mortality. Analysis was conducted using natural-logarithm transformed values of the PET parameters [(ln(MTVwb), ln(TLGwb), and ln(SUVmaxwb)] in order to achieve a near-normal distribution of independent variables. Univariate and multivariate analyses were performed with Cox proportional hazard regression models to test for an association with the primary end point, OS. P-value of <0.05 from a two-tailed test was considered significant. Survival curves were plotted using the Kaplan-Meier method.
Results
Model fitting
The model was fitted using the training dataset of 110 patients with Stage 3B NSCLC (41% adenocarcinoma; 32% squamous cell; 27% other histologic sub-type) who met the inclusion criteria, with patient characteristics summarized in Table 1. The median patient age was 67.3 (range 31.4–83.9) years. There were 47 Caucasian patients, 60 African American patients and 3 Asian patients. The majority of patients (69%) were managed non-surgically (with chemotherapy and/or radiation), while 22% received surgical treatment, and 9% did not treatment. 86/110 patients expired during follow-up. The median OS was 14 months. 1-year, 2-year, and 5-year OS was 56.5%, 34.6% and 13.9%, respectively. The median follow-up among survivors was 26.0 months (inter-quartile range 13.6 to 57.1 months).
Univariate Cox regression analysis showed no significant difference in OS on the basis of age, gender, or histology (Table 2). Surgical treatment (24/110 patients) was associated with improved OS, as compared to the no treatment and non-surgical treatment groups. Some of the PET/CT variables, ln(TLGWB) and ln(SUVWB), were not associated with OS.
However, ln(MTVwb) was positively associated with OS, with a hazard ratio (HR) of 1.23 with 95% confidence interval (95% CI) of 1.01–1.49, (p = 0.037). This association persisted on multivariate Cox regression analysis with a HR of 1.28 (95% CI =1.01–1.64, p = 0.043), after adjustment for age, gender, treatment and tumor histology (Table 3).
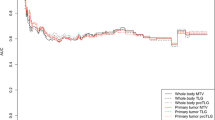
The training dataset was segmented by the median MTVwb of 85.6 mL, Kaplan-Meier survival curves (Fig. 2) demonstrate decreased OS among patients with MTVwb greater than or equal to the median, when compared to those patients with MTVwb less than the median (p = 0.021). The median OS was 9.5 months in patients with MTVwb greater than or equal to the median, while the median OS was 17.3 months in patients with MTVwb less than the median.
Kaplan-Meier overall survival curves of the training dataset of 110 patients with TNM Stage 3B NSCLC, stratified by the median MTVwb of 85.6 mL. The dashed line indicates patient group with MTVwb greater than or equal to 85.6 ml with median OS of 9.5 months. The solid line indicates patient group with MTVwb less than 85.6 ml with median OS of 17.3 months. The difference is statistically significant with p = 0.02
Model validation
To validate the model, a separate analysis was performed using a dataset of 44 patients who were imaged and managed from medical center B. These 44 patients received radiation-based treatment. The median OS was 20 months and 1-year, 2-year, and 5-year OS was 60%, 45% and 38%, respectively. 24/44 patients (55%) expired during follow-up. The median follow-up among survivors was 30.7 months (inter-quartile range 12.7 o 49.1 months).
With a univariate Cox regression model, there was significant positive correlation of ln(MTVwb) with OS, HR of 1.83 (95% CI = 1.14–2.94, p = 0.012). For 7 of 44 patients, the SUVmax and TLGwb were not available due to missing accurate weight information during PET/CT acquisition. Univariate Cox regression analysis in the remaining 37 patients demonstrated no statistically significant association of ln(TLGwb) (HR = 1.37, 95% CI = 0.94–2.00, p = 0.1) and ln(SUVmaxwb) (HR = 1.30, 95% CI = 0.53–3.17, p = 0.57) with OS. After adjusting for tumor histology, there remained significant positive correlation with ln(MTVwb) and OS, with HR of 1.78 (95% CI = 1.01–2.90, p = 0.02). The results provided further evidence for the prognostic value of ln(MTVwb). Kaplan-Meier survival curves with groups defined by the median MTVwb from the training set (85.6 mL) further demonstrated significantly lower OS among patients with MTVwb ≥85.6 mL, when compared to those with MTVwb <85.6 mL (p = 0.028; Fig. 3). The median OS was 13.9 months in patients MTVwb ≥85.6 mL. For patients with MTVwb <85.6 mL, the median OS could not be determined because more than 50% of patients were alive at the last follow-up (median follow-up of 30.7 months).
Kaplan-Meier overall survival curves of the validation dataset of 44 patients with TNM stage 3B NSCLC, stratified by the median MTVwb of the training dataset, 85.6 mL. The dashed line represents the patient group with MTVwb ≥85.6 ml with median OS of 13.9 months. The solid line represents the patient group with MTVwb <85.6 ml with median OS not reached during follow-up period. The groups were significantly different with p = 0.03
Discussion
Quantitative PET/CT parameters are increasingly used to better stratify patients with cancer. Multiple studies have evaluated the association of primary tumor and whole body MTV, TLG, and SUVmax with respect to OS, though this has yet to be evaluated for Stage 3B NSCLC (8th edition TNM classification) (Liao et al., 2012a; Zhang et al., 2013a; Zhang et al., 2013b; Ohri et al., 2015; Liao et al., 2012b; Chung et al., 2014; Im et al., 2015; Hyun et al., 2013; Hyun et al., 2014; Carvalho et al., 2013; Kim et al., 2012; Abelson et al., 2012; Satoh et al., 2014; Winther-Larsen et al., 2016; Yoo et al., 2012; Zhu et al., 2016; Vu et al., 2013; Lee et al., 2007). We sought to better delineate prognosis among patients with Stage 3B NSCLC by utilizing MTVwb, SUVmaxwb, and TLGwb.
Among patients with Stage 3B NSCLC, greater MTVwb was associated with shorter OS, independent of age, sex, and histology. This was further validated by an external dataset of 44 patients treated with radiation-based treatment at outside hospitals. Other studies have shown that OS significantly decreases with every 1 cm increase in primary tumor burden and with increasing number and extent of nodal metastases, which prompted recent changes to the TNM classification (Asamura et al., 2015; Goldstraw et al., 2016). Thus, it is not surprising that quantitative PET/CT measures of whole body tumor burden are similarly associated with OS.
Here we did not find a significant association between SUVmaxwb or TLGwb and OS in patients with Stage 3B NSCLC. SUVmaxwb is a maximum single voxel measurement, so it may not be representative of the entire disease process. Additionally, SUVmaxwb is not representative of the total extent of tumor burden. Though TLGwb incorporates MTVwb, it was not statistically significantly associated with OS in this sample of patients with Stage 3B NSCLC, despite the estimated HR of 1.13. The lack of statistical significance is most likely due to the small sample size in this study, as opposed to a true lack of association with survival.
Among the Stage 3B NSCLC patients in the training cohort, the 2-year and 5-year OS was 34.6% and 13.9%, lower than the survival observed in the IASLC database (44% and 26%, respectively) (Goldstraw et al., 2016). However, our validation dataset had 2- and 5-year survival of 45%, 38%, which is more similar to the IASLC database. One explanation for the difference in OS may be related to socioeconomic status: Center A serves a predominantly low-income neighborhood, a factor that has been previously associated with worse OS (Aldrich et al., 2013). Furthermore, the training dataset included 10 patients who had no treatment, which is likely to lower OS.
The training dataset had a significantly higher proportion of African American patients (55%) than other studies, like the 1996–2007 Florida Cancer Data System registry of 98,541 patients with NSCLC, which was only 7.4% African American (Tannenbaum et al., 2014). Although our study included a disproportionate number of African Americans compared to both other registries and the national population, prior work by Aldrich et al., has shown that lung cancer survival is independent of race, when adjusting for stage and socioeconomic status (Aldrich et al., 2013).
Limitations
Due to the retrospective design of this study, it was not possible to control the type of surgery, chemotherapy or radiation that patients received. Treatment for each patient was determined at the discretion of the surgeon and oncologist and, ultimately, by the patient. In addition, PET/CT has limited sensitivity to detect lesions which are less than 1 cm in diameter or which have low metabolic uptake, likely resulting in a slight under measurement of MTVwb and TLGwb. Since patients in the validation dataset were exclusively treated with radiation-based treatment, and the significant association between OS and MTVwb persists, this strongly suggests the robust prognostic value of MTVwb.
In summary, among patients with Stage 3B NSCLC increasing MTVwb measured on baseline FDG PET/CT is associated with worse OS in both univariate and multivariate cox regression analysis, as seen in both the training and validation datasets. Currently, PET/CT volumetric parameters do not affect clinical management, but hopefully the developing knowledge regarding the values of these measurements may allow more targeted treatment for patients with more or less aggressive disease. Regardless, identifying which patients are more likely to survive to 2 or 5 years may be extremely valuable to patients, who may be planning the final months or years of their life.
Conclusion
MTVwb is a prognostic marker for OS in patients with Stage 3B NSCLC, independent of age, gender, treatment, and tumor histology.
Abbreviations
- AJCC:
-
American Joint Committee on Cancer
- CT:
-
Computed tomography
- FDG:
-
2-deoxy-2-[18F]fluoro-D-glucose
- HR:
-
Hazard ratio
- IASLC:
-
International Association for the Study of Lung Cancer
- MBq:
-
Megabecquerel
- MTVwb:
-
Whole-body metabolic tumor volume
- NSCLC:
-
Non-small cell lung cancer
- OS:
-
Overall survival
- PET:
-
Positron emission tomography
- SUVmaxwb:
-
Maximum standardized uptake value
- TLGwb:
-
Whole body total lesion glycolysis
- TNM:
-
Tumor-node-metastases
- UICC:
-
Union for International Cancer Control
References
Siegel RL, Miller KD, Jemal A (2016) Cancer statistics, 2016. CA Cancer J Clin 66(1):7–30
Detterbeck FC, Chansky K, Groome P et al (2016) The IASLC Lung Cancer Staging Project: Methodology and Validation Used in the Development of Proposals for Revision of the Stage Classification of NSCLC in the Forthcoming (Eighth) Edition of the TNM Classification of Lung Cancer. J Thorac Oncol 11(9):1433–1446
Asamura H, Chansky K, Crowley J et al (2015) The International Association for the Study of Lung Cancer Lung Cancer Staging Project: Proposals for the Revision of the N Descriptors in the Forthcoming 8th Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 10(12):1675–1684
Rami-Porta R, Bolejack V, Crowley J et al (2015) The IASLC Lung Cancer Staging Project: Proposals for the Revisions of the T Descriptors in the Forthcoming Eighth Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 10(7):990–1003
Goldstraw P, Chansky K, Crowley J et al (2016) The IASLC Lung Cancer Staging Project: Proposals for Revision of the TNM Stage Groupings in the Forthcoming (Eighth) Edition of the TNM Classification for Lung Cancer. J Thorac Oncol 11(1):39–51
Liao S, Penney BC, Wroblewski K et al (2012a) Prognostic value of metabolic tumor burden on 18F-FDG PET in nonsurgical patients with non-small cell lung cancer. Eur J Nucl Med Mol Imaging 39(1):27–38
Zhang H, Wroblewski K, Liao S et al (2013a) Prognostic value of metabolic tumor burden from (18)F-FDG PET in surgical patients with non-small-cell lung cancer. Acad Radiol 20(1):32–40
Zhang H, Wroblewski K, Appelbaum D, Pu Y (2013b) Independent prognostic value of whole-body metabolic tumor burden from FDG-PET in non-small cell lung cancer. Int J Comput Assist Radiol Surg 8(2):181–191
Ohri N, Duan F, Machtay M et al (2015) Pretreatment FDG-PET metrics in stage III non-small cell lung cancer: ACRIN 6668/RTOG 0235. J Natl Cancer Inst 107(4):djv004. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4402361/pdf/djv004.pdf
Rocco G, Morabito A, Leone A, Muto P, Fiore F, Budillon A (2016) Management of non-small cell lung cancer in the era of personalized medicine. Int J Biochem Cell Biol 78:173–179
Liao S, Penney BC, Zhang H, Suzuki K, Pu Y (2012b) Prognostic value of the quantitative metabolic volumetric measurement on 18F-FDG PET/CT in Stage IV nonsurgical small-cell lung cancer. Acad Radiol 19(1):69–77
Chung HW, Lee KY, Kim HJ, Kim WS, So Y (2014) FDG PET/CT metabolic tumor volume and total lesion glycolysis predict prognosis in patients with advanced lung adenocarcinoma. J Cancer Res Clin Oncol 140(1):89–98
Im HJ, Pak K, Cheon GJ et al (2015) Prognostic value of volumetric parameters of (18)F-FDG PET in non-small-cell lung cancer: a meta-analysis. Eur J Nucl Med Mol Imaging 42(2):241–251
Hyun SH, Choi JY, Kim K et al (2013) Volume-based parameters of (18)F-fluorodeoxyglucose positron emission tomography/computed tomography improve outcome prediction in early-stage non-small cell lung cancer after surgical resection. Ann Surg 257(2):364–370
Hyun SH, Ahn HK, Kim H et al (2014) Volume-based assessment by (18)F-FDG PET/CT predicts survival in patients with stage III non-small-cell lung cancer. Eur J Nucl Med Mol Imaging 41(1):50–58
Carvalho S, Leijenaar RT, Velazquez ER et al (2013) Prognostic value of metabolic metrics extracted from baseline positron emission tomography images in non-small cell lung cancer. Acta Oncol 52(7):1398–1404
Kim K, Kim SJ, Kim IJ, Kim YS, Pak K, Kim H (2012) Prognostic value of volumetric parameters measured by F-18 FDG PET/CT in surgically resected non-small-cell lung cancer. Nucl Med Commun 33(6):613–620
Abelson JA, Murphy JD, Trakul N et al (2012) Metabolic imaging metrics correlate with survival in early stage lung cancer treated with stereotactic ablative radiotherapy. Lung Cancer 78(3):219–224
Satoh Y, Onishi H, Nambu A, Araki T (2014) Volume-based parameters measured by using FDG PET/CT in patients with stage I NSCLC treated with stereotactic body radiation therapy: prognostic value. Radiology 270(1):275–281
Winther-Larsen A, Fledelius J, Sorensen BS, Meldgaard P (2016) Metabolic tumor burden as marker of outcome in advanced EGFR wild-type NSCLC patients treated with erlotinib. Lung Cancer 94:81–87
Yoo SW, Kim J, Chong A et al (2012) Metabolic Tumor Volume Measured by F-18 FDG PET/CT can Further Stratify the Prognosis of Patients with Stage IV Non-Small Cell Lung Cancer. Nucl Med Mol Imaging 46(4):286–293
Zhu X, Liao C, Penney BC et al (2017) Prognostic value of quantitative PET/CT in patients with a nonsmall cell lung cancer and another primary cancer. Nucl Med Commun 38(2):185–192
Vu CC, Matthews R, Kim B, Franceschi D, Bilfinger TV, Moore WH (2013) Prognostic value of metabolic tumor volume and total lesion glycolysis from (1)(8)F-FDG PET/CT in patients undergoing stereotactic body radiation therapy for stage I non-small-cell lung cancer. Nucl Med Commun 34(10):959–963
Lee P, Weerasuriya DK, Lavori PW et al (2007) Metabolic tumor burden predicts for disease progression and death in lung cancer. Int J Radiat Oncol Biol Phys 69(2):328–333
Tannenbaum SL, Koru-Sengul T, Zhao W, Miao F, Byrne MM (2014) Survival disparities in non-small cell lung cancer by race, ethnicity, and socioeconomic status. Cancer J 20(4):237–245
Aldrich MC, Grogan EL, Munro HM, Signorello LB, Blot WJ (2013) Stage-adjusted lung cancer survival does not differ between low-income Blacks and Whites. J Thorac Oncol 8(10):1248–1254
Acknowledgements
N/A
Funding
This work was supported in part by a grant (R21 CA181885) from the National Cancer Institute of the National Institutes of Health.
Availability of data and materials
The data supporting the findings can be found in the corresponding author’s institution.
Author information
Authors and Affiliations
Contributions
Guarantors of integrity of entire study: BZD, F-MK and YP. Study concepts/study design or data acquisition or data analysis/interpretation: all authors; Manuscript drafting or manuscript revision for important intellectual content: all authors. Approval of final version of submitted manuscript: all authors; Agrees to ensure any questions related to the work are appropriately resolved by all authors; Literature research: BZD, F-MK and YP. Clinical studies: CZ, LX, HL, LY, YL, YP. Statistical analysis: YP and F-MK. Manuscript editing: all authors.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was approved by our Institutional Review Board of the University of Chicago, which waived the requirement for informed consent and all methods were carried out in accordance with relevant guidelines and regulations.
Consent for publication
N/A
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Dashevsky, B.Z., Zhang, C., Yan, L. et al. Whole body metabolic tumor volume is a prognostic marker in patients with newly diagnosed stage 3B non-small cell lung cancer, confirmed with external validation. European J Hybrid Imaging 1, 8 (2017). https://doi.org/10.1186/s41824-017-0013-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s41824-017-0013-z