Abstract
Background
Diagnosis of primary immunodeficiencies (PIDs) is complex and cumbersome yet important for the clinical management of the disease. Exome sequencing may provide a genetic diagnosis in a significant number of patients in a single genetic test.
Methods
In May 2013, we implemented exome sequencing in routine diagnostics for patients suffering from PIDs. This study reports the clinical utility and diagnostic yield for a heterogeneous group of 254 consecutively referred PID patients from 249 families. For the majority of patients, the clinical diagnosis was based on clinical criteria including rare and/or unusual severe bacterial, viral, or fungal infections, sometimes accompanied by autoimmune manifestations. Functional immune defects were interpreted in the context of aberrant immune cell populations, aberrant antibody levels, or combinations of these factors.
Results
For 62 patients (24%), exome sequencing identified pathogenic variants in well-established PID genes. An exome-wide analysis diagnosed 10 additional patients (4%), providing diagnoses for 72 patients (28%) from 68 families altogether. The genetic diagnosis directly indicated novel treatment options for 25 patients that received a diagnosis (34%).
Conclusion
Exome sequencing as a first-tier test for PIDs granted a diagnosis for 28% of patients. Importantly, molecularly defined diagnoses indicated altered therapeutic options in 34% of cases. In addition, exome sequencing harbors advantages over gene panels as a truly generic test for all genetic diseases, including in silico extension of existing gene lists and re-analysis of existing data.
Similar content being viewed by others
Background
Primary immunodeficiencies (PIDs) are genetically and phenotypically heterogeneous disorders characterized by an inborn increased susceptibility to infections. From the genetic perspective, over 300 genes have been identified as monogenic causes of PIDs [1,2,3,4]. The majority of pathogenic variants in PID genes are reported to cause disease in a purely autosomal recessive (AR) fashion (69%), compared to an autosomal dominant (AD) (20%), AR and AD (5%), and X-linked (XL) (6%) manner [1,2,3,4].
The phenotype of PID patients ranges from frequent or more severe relatively common infections to serious clinical manifestations due to rare pathogens that require immediate clinical care to prevent fatality [2]. In addition to infections, some patients with PIDs can also experience autoimmune or inflammatory conditions, as well as malignancy and developmental abnormalities [1, 2]. PIDs are divided in 10 specific subtypes according to the International Union of Immunological Societies (IUIS) PID classification [1]. The clinical variable phenotype of PIDs makes diagnosing patients based on their respective phenotypes challenging. A recent publication describes that 55% of 110 cases were misdiagnosed based on their initial clinical characteristics [5]. In order to prevent this, a more robust and rapid identification of the underlying genetic defect would be of great clinical benefit: a “genotype-first approach” may provide a molecularly defined diagnosis in a significant amount of cases.
Genetic diagnosis of PIDs has been available for a relatively long time, but until now it has been complicated by the need to pinpoint the gene of interest: invariably, this is linked to the correct (and often difficult) clinical diagnosis in the first place. Fortunately, the availability of rapid and cheap sequencing methodologies now allows for more unbiased genetic diagnostics. Exome sequencing in particular has been shown to be an effective tool to elucidate the genetic defect underlying other types of heterogeneous disorders [6, 7]. We performed exome sequencing to provide a genetic diagnosis for patients suffering from a broad range of immune deficits. The identification of the genetic basis of PIDs provides insight into the molecular mechanisms of these diseases and may offer customized treatment options [5, 8,9,10]. Compared to targeted enrichment approach, exome sequencing has several major advantages: first, the in silico exome gene panel can easily be adjusted upon identification of novel PID genes; second, exome-wide analysis allows analysis for variants in novel genes not included in the gene panel; third, exome sequencing allows genome-wide data access and hence more reliable detection of copy number variants (CNVs) and regions of homozygosity (ROH) [5, 11,12,13,14]. To reduce the complexity of the analysis and speed up the process, exome sequencing can be combined with an in silico analysis of a set of already known disease genes [15].
Due to large genetic and phenotypic heterogeneity of PIDs, and the rapidly increasing number of PID genes identified over the last years [1, 2, 16], we implemented exome sequencing as a single test in routine diagnostics for PIDs in 2013 in a large tertiary academic hospital (Radboud University Medical Center). From then until October 2016, a group of 254 consecutively referred patients suffering from PIDs have been tested by exome sequencing, and here we report on their genetic diagnostic outcome.
Methods
Samples
Between May 2013 and October 2016, 254 patient DNA samples (249 families) from the main referring clinics for exome sequencing to our diagnostic laboratory (160 from The Netherlands, 8 from Finland, and 81 from Saudi Arabia) were submitted for whole exome sequencing. The average age at testing was 21 years (range from 1 month to 79 years), and the male/female distribution was 117M/137F (details in Additional file 1: Table S1). Families were counseled and provided consent for “PID gene panel only” or “gene panel and exome-wide analysis” as presented here.
Exome sequencing procedure
Genomic DNA was isolated from whole blood. The experimental workflow of all exomes was performed at BGI Europe (Beijing Genome Institute Europe, Copenhagen, Denmark). Exonic regions were enriched using the Agilent (Agilent Technologies, CA, USA) SureSelect V4 (n = 85) or V5 (n = 169) kit and sequenced using an Illumina Hiseq (Illumina, CA, USA) sequencer with 101-bp paired end reads to a median coverage of > 75x. Sequenced reads were mapped to the hg19 reference genome using the mapping algorithm from BWA [17] (version 0.5.9-r16) and called by the GATK unified genotyper [18] (version 3.2-2). All variants were annotated using an in-house pipeline for exome analysis containing variant and gene-specific information, amongst which the variant population frequencies from > 5000 in-house exomes [7].
Exome variant interpretation
For the gene panel analysis, a bioinformatic in silico filter was applied to select for variants affecting the known > 300 PID genes [19]. This gene panel consisted of 263 established (OMIM) PID genes in 2013, expanding to 302 genes in 2016 (all earlier versions available) [19]. Variants were filtered for coding, non-synonymous variants with population frequencies below 1% in our in-house database (a database of > 5000 exomes), and evaluated regarding their possible pathogenicity. The latter was performed using population frequencies [20], nucleotide conservation scores (PhyloP), and in silico pathogenicity predictions (SIFT, Polyphen2, Mutationtaster) combined with genetic and phenotypic overlap with earlier described cases to estimate the contribution of the genetic variant to disease [21].
Eighty-one percent of diagnosis-negative patients provided consent for exome-wide analysis. All variants derived from exome sequencing were prioritized for coding, non-synonymous variants with population frequencies of ≤ 1% in-house and ≤ 5 homozygous occurrences reported in EXAC for autosomal recessive candidates, and allele counts of ≤ 10× in house or ≤ 20× in EXAC for autosomal dominant candidates [20]. The exome-wide analysis focused on variants in recently described genes and genes involved in immune pathways, based on GO terms, mouse knockout model phenotypes, or the Kyoto Encyclopedia of Genes and Genomes (KEGG). In addition, we filtered for variants in genes with known NCBI protein-protein interactions with known disease genes for similar phenotypes [22].
All identified genetic variants were judged on their possible pathogenicity based on guidelines of the Association for Clinical Genetic Science and the American College of Medical Genetics and Genomics [21, 23]. We only considered variants disease-causing if we found sufficient phenotypic overlap with earlier described cases based on OMIM [24]. In addition, we only report variants classified as class 5 (pathogenic), class 4 (likely pathogenic) (see Table 1 and Additional file 2: Table S2), or class 3 (uncertain significance) (see Additional file 3: Table S3), because the variants classified as class 2 (likely benign) or class 1 (benign) are probably tolerated [21, 23].
Homozygosity calling
Regions of homozygosity (ROH) were called using RareVariantVis [13]. Downstream filtering included filtering for larger (≥ 5 Mb) homozygous regions, in which ≥ 85% of all variants were called to be homozygous.
CNV calling
Copy number variant (CNV) calling was performed using CoNIFER to calculate RPKM-based absolute Z-scores [14, 25]. Rare copy number variants affecting PID-associated genes were followed up similarly as the earlier described single nucleotide variants (SNVs), small insertions, or deletions (indels).
Validation of detected variants and follow-up in families
All reported low-quality variant calls (GATK quality by depth < 500) were confirmed by standard Sanger sequencing. Patients with reported class 3 or class 4 variants were counseled to perform further analyses on their respective families. To gain more genetic evidence for causality of the variants, we have performed co-segregation analysis to confirm de novo mutations or carrier status in parents.
Immunophenotyping
For 75% of patients, the immunophenotypes were further characterized by determining one or more of the functional immunological defects. This included quantification of cellular subtypes and antibodies in whole blood, and measurement of cytokine production capacity upon in vitro stimulation assays. The latter experiments were performed similar to previous reports [26]. In brief, peripheral blood mononuclear cells (PBMCs) were isolated by density centrifugation and cultured with a medium or a medium supplemented with immune response-inducing ligands or heat-killed pathogens. Cytokine production capacity was measured using an enzyme-linked immunosorbent assay (ELISA).
Results
Patient cohort
In total, 254 patients from 249 families were referred for diagnostic exome sequencing. Two hundred nineteen patients presented with unusual bacterial, viral, or fungal infections or autoimmune manifestations or combinations of such (Fig. 1a, Additional file 1: Table S1 and Additional file 4: Table S4). Immunophenotype defects were observed in 194 patients; of those, 133 patients had aberrant blood cell counts, 102 patients showed altered antibody profiles, and 31 patients revealed irregular cytokine production (Fig. 1b, Additional file 1: Table S1 and Additional file 4: Table S4).
Clinical and immunophenotypic overview of the 254 patients included in the diagnostic PID cohort, including percentages of patients with genetic diagnoses per subgroup. a For 219 patients, pathogens and/or autoimmunity was identified. b Immunophenotypic defects were characterized in 194 patients. Quantification of blood cell numbers, antibody levels, and cytokine production aided to determine the genetic diagnosis for these patients. c The diagnostic yield per cohort based on the country from which the patients were referred. Compared to European patients, a higher percentage of patients from Saudi Arabia received a genetic diagnosis
Exome sequencing
Whole exome sequencing resulted in an average coverage of 120.7× (Agilent SureSelect V4) and 130.2× (Agilent SureSelect V5), covering 95.3% of the exome at least 20-fold. For the genes within our gene panel, the average coverage was 132.6× and 93% of the base pairs of these genes were covered at least 20 times (details in Additional file 5: Table S5).
Exome variant interpretation
For each exome, a bioinformatic in silico panel of genes was applied as a first-tier test to select for variants affecting the > 300 known PID genes [19]. This list is regularly updated in silico whenever novel PID genes are discovered. This yielded on average 1542 genetic variants in known PID genes per individual. Additional filtering for coding, non-synonymous variants and population frequency ≤ 1% resulted in 10 to 40 variants per case, which were evaluated on their possible pathogenicity (Fig. 2). Pathogenic (class 4 or class 5) variants were identified in at least one of the known PID genes for 62 patients (24%). Eighty-one percent of genetic-diagnosis-negative patients provided consent for exome-wide analysis. (Re-)analysis for variants in recently published PID genes and genes causing defects in immunological sub-pathways yielded an additional (class 4 or class 5) genetic diagnosis for 10 patients (5% of all exome-wide analyzed samples; 4% of the entire cohort). The combined result of our two-step analysis provided a (class 4 or class 5) genetic diagnosis in 28% of our patients (Figs. 1c and 2, see Table 1 and Additional file 2: Table S2). In total, 84 (33%) of all 254 patients were referred from Saudi Arabia; the diagnostic yield (57%, 48/84 patients) in this sub-cohort was significantly (P value 2.4e−11, two-sided Fisher’s exact test) higher than that in patients of European descent (14%, 24/170). In four of these patients, two independent pathogenic variants in different genes were identified which both contributed to the patient phenotypes (see Additional file 2: Table S2. pt 83.1, 147.1, 153.1, and 222.1).
Schematic flowchart overview of the diagnostic exome procedure. Two hundred fifty-four patients from 249 families were referred for exome sequencing. Gene panel analysis resulted in a genetic diagnosis for 24% of patients. Eighty-one percent of diagnosis-negative patients provided consent for exome-wide analysis of their data. This analysis resulted in a genetic diagnosis for 10 additional patients (6% of exome-wide analyzed patients, 4% of the entire cohort). Data of the remaining 146 patients are re-analyzed for analysis of novel and recently published genes
For an additional 12 patients (5%), exome analysis only identified novel variants in known genes (class 3) with overlapping disease phenotypes (see Additional file 3: Table S3).
Homozygosity calling
We identified in total 1399 large (≥ 5 Mb) homozygous regions in 165 of 254 patient exomes. One thousand sixty-seven of these regions were identified in 81 patients from Saudi Arabia, 318 regions in 68 Dutch patients, and 14 regions in 6 cases from Finland. Thirty-three (82%) of all homozygous pathogenic variants in autosomal recessive genes were present in these homozygous regions. In one Saudi Arabian patient suffering from severe combined immunodeficiency (SCID) (T−, B+, NK−; see Table 1 and Additional file 2: Table S2, 146.1), homozygosity mapping revealed three large homozygous regions on chromosome 19 spanning in total 32.8 Mb (see Additional file 6: Table S6 and Additional file 7: Additional material and references). One of these regions overlapped with the genetic location of JAK3, pathogenic variants which are a known cause of SCID [1]. In-depth analysis of JAK3 resulted in identification of a homozygous deletion of exon 10 (Fig. 3).
Unclear pathogenic effect of known TRAF3 variants
In five phenotypically heterogeneous patients, exome sequencing identified potentially causative TRAF3 variants; four of our patients carried the heterozygous p.R118W variant which was reported earlier in a patient with herpes simplex encephalitis [27], and one patient carried a p.V240I variant in heterozygous state (see Additional file 3: Table S3. pt 42.1, 76.1, 95.1, 132.1, 209.1).
Altered therapy options after genetic diagnosis
For 30 (30/72 = 42%) patients for whom exome sequencing molecularly confirmed the diagnosis of SCID, immunodeficiency, centromere instability, and facial anomalies (ICF) syndrome, chronic granulomatous disease, or chronic mucocutaneous candidiasis, bone marrow transplantation is a published treatment option. For additional 25 patients (34%) (Table 1), the genetic diagnosis defined targeted therapeutic options based on available literature [8, 28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52].
Discussion
The clinical and genetic heterogeneity of PIDs makes exome sequencing a valuable first-tier diagnostic tool for identification of genetic defects underlying PIDs. We present routine diagnostic exome sequencing in a phenotypically heterogeneous group of 254 patients from 249 families. Exome sequencing identified pathogenic genetic variants (interpreted as class 4 or 5) in established disease-causing genes in 72 patients (28%). In four of these patients, a dual genetic diagnosis was made based on two independent genetic pathogenic variants similar to a report for two developmental phenotypes [53].
In addition, for 12 patients (5%), we have identified genetic variants that could possibly contribute to disease, as these patients presented with OMIM-associated clinical features. However, there was insufficient genetic and functional evidence to conclude on the pathogenicity of these variants, which therefore remained variants of unknown significance (class 3 variants; see Additional file 3: Table S3).
The diagnostic yield in our study is in line with other studies describing targeted or exome-wide analyses for heterogeneous groups of PID patients [5, 11, 54, 55]. Phenotypic selection for homogeneous patient cohorts with immunological defects result in increased percentages of diagnoses [56,57,58]. In addition, the PID-associated genes selected for the gene panels, and the stringency of variant prioritization, result in (minor) differences amongst these studies.
We observed a higher percentage of genetic diagnosis for patients referred from Saudi Arabia (57%) compared to patients from Europe (14%) (Fig. 1c). This significant (P value 2.4e−11, two-sided Fisher’s exact test) difference likely arises from two major reasons. Firstly, the Saudi Arabian patients are referred at a very young age (average age of 5.5 years compared to 29.3 years for the European cohort, Fig. 4a), which creates a selection bias towards more severely affected patients. It generally remains challenging to provide molecular diagnoses for older patients from heterogeneous backgrounds. Variants causing late-onset disorders are likely present at higher frequencies in population databases like GnomAD. In addition, the older patients have a higher risk to be exposed to environmental factors (specific pathogens) during their lifetime, highlighting an extra challenge for PID diagnostics.
Differences in percentage diagnostic yield based on age and homozygous regions. a The age distribution of the entire cohort, the European cohort, the Saudi Arabian cohort, and the cases with a genetic diagnosis. b The number of large (> 5 Mb) homozygous regions per cohort. The increased number of homozygous regions in the Saudi Arabian cohort influenced diagnostic yield of the overall cohort
Secondly, increased consanguinity levels in the Saudi Arabian population create a bias towards homozygously inherited defects. Since the vast majority of known PID genes (69%) cause disease in an AR fashion, higher rates of molecular diagnoses can be expected in patients with more homozygous regions. We detected homozygous pathogenic variants in 44/254 patients, of which 36 were referred from Saudi Arabia. The Saudi Arabian patients have a significantly (P value < 0.0001, Welch’s t-test) higher number of genomic homozygous regions compared to the European patients (Fig. 4b, see Additional file 6: Table S6).
Not all homozygous pathogenic variants described in this study are SNVs or indels commonly identified by exome sequencing. Homozygosity mapping on exome data can also reveal regions in which homozygous copy number variants (CNVs) may occur. As an example, we focused on a homozygous region on chromosome 19 and could identify a disease-causing homozygous single exon deletion (patient 146.1, JAK3 exon 10, Fig. 3) in one SCID patient. The contribution of CNVs such as single exon deletions to disease is underestimated in many genetic analyses for PIDs [5], and more systematic assessments from WES data allow up to 6% disease-causing CNVs in heterogeneous disorders [25].
Next to the AR-inherited variants, exome sequencing provided heterozygously rare and private variants that affect known PID (-associated) genes. In case a novel genetic variant did not pass the conservative guideline thresholds [21, 23], the variant was not considered pathogenic in this patient. We acknowledge that these stringent criteria limited the diagnostic outcome of exome sequencing in our cohort at this stage, but we feel this is important in order to prevent misdiagnoses. Systematic trio analysis and functional characterization of each novel missense variant are warranted to gain further insight in the disease mechanism on the individual level [6].
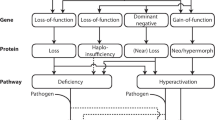
In this study, most pathogenic (class 5) variants were discovered in AR PID genes. There is a bias towards AR disease because all known AR PID genes are caused by genetic loss-of-function (LoF) mutations, and most LoF mutations are considered pathogenic in the ACMG classification [21]. In contrast, the majority of AD-inherited PIDs are the result of gain-of-function (GoF) or dominant-negative mechanisms and are therefore more likely the result of missense variants, or truncating variants affecting the last exon or the last 50 nucleotides of the penultimate exon of the gene [21, 59]. These variants are only considered pathogenic (class 5) in case the exact same genetic variant was described earlier. Generally, these types of variants are less likely pathogenic since the altered RNA is not predicted to undergo nonsense-mediated decay and the altered protein is expressed [60].
Exome sequencing analysis identified more pathogenic variants in specific subgroups of patients compared to others. Similar to earlier reports, severely affected patients were more likely to receive a genetic diagnosis [5]. First, evaluation of clinical characteristics revealed that the patients with a higher burden of infections caused by multiple pathogens and/or autoimmune manifestations were significantly (P value 0.0002, two-sided Fisher’s exact test) more likely to receive a genetic diagnosis (40%; 48/121), compared to patients with infections restricted to a single pathogen or autoimmune manifestation (14%; 14/98) (Fig. 1a). Moreover, patients with defects in important immune cell populations are expected to have more clinical manifestations. In line with this, a significantly (P value 0.0014, two-sided Fisher’s exact test) higher percentage of patients with aberrant blood cell populations received a genetic diagnosis (37%; 49/133), compared to patients with normal blood cell populations (19%; 23/123) (Fig. 1b).
Unclear pathogenic effect of known TRAF3 variants
The exact same pathogenic variants as previously reported in literature were identified in 40 patients from our cohort. In 36 (90%) of these patients, the presented immunophenotypic characteristics were similar to earlier described cases. However, exome sequencing revealed the same TRAF3 variant p.(R118W) as described in one patient with HSV encephalitis in four patients (see Additional file 3: Table S3. 44.1, 76.1, 99.1, and 217.1) within our cohort [27]. Without careful phenotypic assessment and genetic evaluation, this may result in a false diagnosis. Only one of the patients carrying a (paternally inherited) TRAF3 variant (76.1) suffered from HSV infections, which could also be caused by a (maternally inherited) frameshift variant in GATA2 p.(R86fs/wt) [61]. In addition, this variant is relatively common in the population [20] (population frequency of 0.3%) and appeared slightly more frequent in this study (1.5%). Due to the high population frequency and disease heterogeneity, we speculate that the TRAF3 variant p.(R118W) might result in a minor broad immunomodulatory defect, and additional genetic and environmental factors further determine the clinical presentation. We therefore concluded that this specific variant was not solely the cause of disease in these patients but should be rather considered a risk/susceptibility factor. This may be important for future diagnostic interpretation of this variant.
Diagnosis by exome-wide analysis
One hundred fifty-six diagnosis-negative patients provided additional informed consent for exome-wide analysis of their data. For 10 of these patients, we identified disease-causing variants in genes that were described after the latest gene panel update, or genes known to affect specific sub-pathways that have been previously published as a genetic cause of similar phenotypes (Table 1). This is exemplified by one case (70.1) suffering from recurrent respiratory tract infections for which exome sequencing identified a homozygous pathogenic variant in the first amino acid of the protein RSPH9 p.(M1T/M1T) [50]. The genotype-first approach led to identification of the pathogenic variant leading to ciliary dyskinesia in this patient, which retrospectively fits the clinical diagnosis. Re-analysis of exome data for novel disease genes, as well as further functional, co-segregation and overlap analysis will ultimately lead to additional genetic diagnoses for a subset of these patients.
Genetic diagnosis-based treatment options
In total, 24 patients were molecularly diagnosed with severe immunological phenotypes like severe combined immunodeficiency (SCID) or immunodeficiency, centromere instability, and facial anomalies (ICF) syndrome, for which bone marrow transplantation is the main remedy [8]. This treatment option may have been considered already based on the clinical presentation alone for some cases; however, referring clinicians valued the molecular diagnosis of SCID confirming this treatment options.
In addition, six patients were molecularly diagnosed with chronic mucocutaneous candidiasis (CMC) or chronic granulomatous disease (CGD), which can be treated with ruxolitinib (CMC) or IFN-γ (CGD) [46, 62]. However, HSCT has also been published as a therapeutic option for these diseases [35, 47].
For an additional 25 patients, the genetic diagnosis provided novel options for targeted therapeutics based on recent literature (Table 1) [8, 28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52]. The long-term effect of these altered therapeutic strategies is still unknown.
Conclusions
In conclusion, exome sequencing proves to be a valuable first-tier test for routine diagnostics in PIDs providing a genetic diagnosis in 28% of patients. In addition, exome sequencing harbors advantages over gene panels as a truly generic test for all genetic diseases, including in silico extension of existing gene lists and re-analysis of the existing data whenever new knowledge is available.
Importantly, we observed that identifying the molecular diagnosis in PID patients confirmed HSCT in 42% of cases as a possible treatment option and identified therapeutic target options for additional 34% of cases. This high amount of possibly “actionable mutations” is uncommon for genetic disorders due to germline mutations, but highlights the possibilities for PIDs in truly personalized medicine. Future studies combining systematic trio analysis of exome, genome, and/or transcriptome data will provide patients with additional diagnoses and insights in targeted therapeutics.
Availability of data and materials
The datasets supporting the conclusions of this article are included within the article and its additional files. All raw data was retrieved in the realm of patients’ diagnostic procedure; this does not allow sharing of the data publically, because the patient families were not consented for sharing their raw data, which can potentially identify the individuals.
References
Bousfiha A, Jeddane L, Picard C, Ailal F, Bobby Gaspar H, Al-Herz W, et al. The 2017 IUIS phenotypic classification for primary immunodeficiencies. J Clin Immunol. 2018;38:129–43.
Picard C, Bobby Gaspar H, Al-Herz W, Bousfiha A, Casanova JL, Chatila T, et al. International Union of Immunological Societies: 2017 primary immunodeficiency diseases committee report on inborn errors of immunity. J Clin Immunol. 2018;38:96–128.
Keerthikumar S, Raju R, Kandasamy K, Hijikata A, Ramabadran S, Balakrishnan L, Ahmed M, Rani S, Selvan LN, Somanathan DS, Ray S, Bhattacharjee M, Gollapudi S, Ramachandra YL, Bhadra S, Bhattacharyya C, Imai K, Nonoyama S, Kanegane H, Miyawaki T, Pandey A, Ohara O, Mohan S. RAPID: Resource of Asian Primary Immunodeficiency Diseases. Nucleic Acids Res. 2009;37:D863-D867.
ESID registry gene list. https://esid.org/Working-Parties/Registry-Working-Party/ESID-Registry/List-of-diseases-and-genes. Accessed 18 Nov 2016.
Stray-Pedersen A, Sorte HS, Samarakoon P, Gambin T, Chinn IK, Coban Akdemir ZH, et al. Primary immunodeficiency diseases – genomic approaches delineate heterogeneous Mendelian disorders. J Allergy Clin Immunol. 2016;139:232–45.
de Ligt J, Willemsen MH, van Bon BWM, Kleefstra T, Yntema HG, Kroes T, et al. Diagnostic exome sequencing in persons with severe intellectual disability. N Engl J Med. 2012;367:1921–9.
Lelieveld SH, Reijnders MRF, Pfundt R, Yntema HG, Kamsteeg E, de Vries P, et al. Meta-analysis of 2,104 trios provides support for 10 novel candidate genes for intellectual disability. Nat Neurosci. 2016;19:1194–6.
Pai S-Y, Logan BR, Griffith LM, Buckley RH, Parrott RE, Dvorak CC, et al. Transplantation outcomes for severe combined immunodeficiency, 2000-2009. N Engl J Med. 2014;371:434–46.
Genovese P, Schiroli G, Escobar G, Di Tomaso T, Firrito C, Calabria A, et al. Targeted genome editing in human repopulating haematopoietic stem cells. Nature. 2014;510:235–40.
Arts P, van de Veerdonk FL, van der Lee R, Langereis MA, Gilissen C, van Zelst-Stams WAG, et al. Immunologic defects in severe mucocutaneous HSV-2 infections: response to IFN-γ therapy. J Allergy Clin Immunol. 2016;138:895–8.
Nijman IJ, Van Montfrans JM, Hoogstraat M, Boes ML, Van De Corput L, Renner ED, et al. Targeted next-generation sequencing: a novel diagnostic tool for primary immunodeficiencies. J Allergy Clin Immunol. 2014;133:529–34 e1.
Gambin T, Akdemir Z, Yuan B, Gu S, Chiang T, Carvalho C, et al. Homozygous and hemizygous CNV detection from exome sequencing data in a Mendelian disease cohort. Nucl Acids Res. 2017;45(4):1633–48.
Stokowy T, Garbulowski M, Fiskerstrand T, Holdhus R, Labun K, Sztromwasser P, et al. RareVariantVis: new tool for visualization of causative variants in rare monogenic disorders using whole genome sequencing data. Bioinformatics. 2016;32:3018–20.
Krumm N, Sudmant P, Ko A. Copy number variation detection and genotyping from exome sequence data. Genome Res. 2012;22:1525–32.
Neveling K, Feenstra I, Gilissen C, Hoefsloot LH, Kamsteeg EJ, Mensenkamp AR, et al. A post-hoc comparison of the utility of sanger sequencing and exome sequencing for the diagnosis of heterogeneous diseases. Hum Mutat. 2013;34:1721–6.
Parvaneh N, Casanova JL, Notarangelo LD, Conley ME. Primary immunodeficiencies: a rapidly evolving story. J Allergy Clin Immunol. 2013;131:314–23.
Li H, Durbin R. Fast and accurate long-read alignment with Burrows-Wheeler transform. Bioinformatics. 2010;26:589–95.
McKenna A, Hanna M, Banks E, Sivachenko A, Cibulskis K, Kernytsky A, et al. The genome analysis toolkit: a MapReduce framework for analyzing next-generation DNA sequencing data. Proc Int Conf Intellect Capital, Knowl Manag Organ Learn. 2009;20:254–60.
Gene list primary immunodeficiencies. https://www.radboudumc.nl/en/patientenzorg/onderzoeken/exome-sequencing-diagnostics/exomepanelspreviousversions/primary-immunodeficienciesversionDG2.7/DG2.8. Accessed 18 Nov 2016.
Lek M, Karczewski KJ, Minikel EV, Samocha KE, Banks E, Fennell T, et al. Analysis of protein-coding genetic variation in 60,706 humans. Nature. 2016;536:285–91.
Richards S, Aziz N, Bale S, Bick D, Das S, Gastier-Forster J. Standards and guidelines for the interpretation of sequence variants: a joint consensus recommendation of the American College of Medical Genetics and Genomics and the Association for Molecular Pathology. Genet Med. 2015;17:405–24.
Arts P, Plantinga TS, van den Berg JM, Gilissen C, Veltman JA, van Trotsenburg AS, et al. A missense mutation underlies defective SOCS4 function in a family with autoimmunity. J Intern Med. 2015;278:203–10.
Wallis Y, Payne S, Mcanulty C, Bodmer D, Sister-mans E, Robertson K, et al. Practice Guidelines for the Evaluation of Pathogenicity and the Reporting of Sequence Variants in Clinical Molecular Genetics. Birmingham: Association for Clinical Genetic Science; 2013.
McKusick-Nathans Institute of Genetic Medicine, Johns Hopkins University (Baltimore, MD) {January 2017}. Online Mendelian Inheritance in Man, OMIM.
Pfundt R, del Rosario M, Vissers LELM, Kwint MP, Janssen IM, de Leeuw N, et al. Detection of clinically relevant copy-number variants by exome sequencing in a large cohort of genetic disorders. Genet Med. 2017;19(6):667–75.
van de Veerdonk FL, Plantinga TS, Hoischen A, Smeekens SP, Joosten LAB, Gilissen C, et al. STAT1 mutations in autosomal dominant chronic mucocutaneous candidiasis. N Engl J Med. 2011;365:54–61.
Pérez de Diego R, Sancho-Shimizu V, Lorenzo L, Puel A, Plancoulaine S, Picard C, et al. Human TRAF3 adaptor molecule deficiency leads to impaired toll-like receptor 3 response and susceptibility to herpes simplex encephalitis. Immunity. 2010;33:400–11.
Zeeli T, Padalon-Brauch G, Ellenbogen E, Gat A, Sarig O, Sprecher E. Pyoderma gangrenosum, acne and ulcerative colitis in a patient with a novel mutation in the PSTPIP1 gene. Clin Exp Dermatol. 2015;40:367–72.
Ouederni M, Vincent QB, Frange P, Touzot F, Scerra S, Bejaoui M, et al. Major histocompatibility complex class II expression deficiency caused by a RFXANK founder mutation: a survey of 35 patients. Blood. 2011;118:5108–18.
Valencic E, Grasso AG, Conversano E, Lucafò M, Piscianz E, Gregori M, et al. Theophylline as a precision therapy in a young girl with PIK3R1 immunodeficiency. J Allergy Clin Immunol Pract. 2018:1–3. https://doi.org/10.1016/j.jaip.2018.02.029.
Ozsahin H, Cavazzana-Calvo M, Notarangelo LD, Schulz A, Thrasher AJ, Mazzolari E, et al. Long-term outcome following hematopoietic stem-cell transplantation in Wiskott-Aldrich syndrome: collaborative study of the European Society for Immunodeficiencies and European Group for Blood and Marrow Transplantation. Blood. 2008;111:439–45.
Schepp J, Proietti M, Frede N, Buchta M, Hübscher K, Rojas Restrepo J, et al. Screening of 181 patients with antibody deficiency for deficiency of adenosine deaminase 2 sheds new light on the disease in adulthood. Arthritis Rheumatol. 2017;69:1689–700.
Gennery AR, Slatter MA, Bredius RG, Hagleitner MM, Weemaes C, Cant AJ, et al. Hematopoietic stem cell transplantation corrects the immunologic abnormalities associated with immunodeficiency centromeric instability facial dysmorphism syndrome. Pediatrics. 2007;120:e1341–4. https://doi.org/10.1542/peds.2007-0640.
Gössling KL, Schipp C, Fischer U, Babor F, Koch G, Schuster FR, et al. Hematopoietic stem cell transplantation in an infant with immunodeficiency, centromeric instability, and facial anomaly syndrome. Front Immunol. 2017;8:773. https://doi.org/10.3389/fimmu.2017.00773
Morillo-Gutierrez B, Beier R, Rao K, Burroughs L, Schulz A, Ewins AM, et al. Treosulfan-based conditioning for allogeneic HSCT in children with chronic granulomatous disease: a multicenter experience. Blood. 2016;128:440–8.
Rissone A, Weinacht KG, la Marca G, Bishop K, Giocaliere E, Jagadeesh J, et al. Reticular dysgenesis–associated AK2 protects hematopoietic stem and progenitor cell development from oxidative stress. J Exp Med. 2015;212:1185–202. https://doi.org/10.1084/jem.20141286.
Morgan BP, Orren A. Vaccination against meningococcus in complement-deficient individuals. Clin Exp Immunol. 1998;114:327–9.
Stepensky P, Simanovsky N, Averbuch D, Gross M, Yanir A, Mevorach D, et al. VPS 45-associated primary infantile myelofibrosis - successful treatment with hematopoietic stem cell transplantation. Pediatr Transplant. 2013;17:820–5.
Wenham M, Grieve S, Cummins M, Jones ML, Booth S, Kilner R, et al. Two patients with Hermansky Pudlak syndrome type 2 and novel mutations in AP3B1. Haematologica. 2010;95:333–7.
Ghosh S, Carmo M, Calero-Garcia M, Ricciardelli I, Bustamante Ogando JC, Blundell MP, et al. T-cell gene therapy for perforin deficiency corrects cytotoxicity defects and prevents hemophagocytic lymphohistiocytosis manifestations. J Allergy Clin Immunol. 2018. https://doi.org/10.1016/j.jaci.2017.11.050.
Takata K, Kubota S, Fukata S, Kudo T, Nishihara E, Ito M, Amino NMA. Methimazole-induced agranulocytosis in patients with Graves’ disease is more frequent with an initial dose of 30 mg daily than with 15 mg daily. Thyroid. 2009;19:559–63.
Ma CA, Stinson JR, Zhang Y, Abbott JK, Weinreich MA, Hauk PJ, et al. Germline hypomorphic CARD11 mutations in severe atopic disease. Nat Genet. 2017;49:1192–201. https://doi.org/10.1038/ng.3898.
Banka S, Blom HJ, Walter J, Aziz M, Urquhart J, Clouthier CM, et al. Identification and characterization of an inborn error of metabolism caused by dihydrofolate reductase deficiency. Am J Hum Genet. 2011;88:216–25.
Zemer D, Livneh A, Danon YL, Pras M, Sohar E. Long-term colchicine treatment in children with familial mediterranean fever. Arthritis Rheum. 1991;34:973–7.
Luzzatto L, Arese P. Favism and glucose-6-phosphate dehydrogenase deficiency. N Engl J Med. 2018;378:60–71. https://doi.org/10.1056/NEJMra1708111.
Weinacht KG, Charbonnier LM, Alroqi F, Plant A, Qiao Q, Wu H, et al. Ruxolitinib reverses dysregulated T helper cell responses and controls autoimmunity caused by a novel signal transducer and activator of transcription 1 (STAT1) gain-of-function mutation. J Allergy Clin Immunol. 2017;139:1629–40.e2. https://doi.org/10.1016/j.jaci.2016.11.022.
Leiding JW, Okada S, Hagin D, Abinun M, Shcherbina A, Balashov DN, et al. Hematopoietic stem cell transplantation in patients with gain-of-function signal transducer and activator of transcription 1 mutations. J Allergy Clin Immunol. 2017;141:704–17.e5. https://doi.org/10.1016/j.jaci.2017.03.049.
Delsing CE, Gresnigt MS, Leentjens J, Preijers F, Frager FA, Kox M, et al. Interferon-gamma as adjunctive immunotherapy for invasive fungal infections: a case series. BMC Infect Dis. 2014;14:166.
Greil C, Roether F, La Rosée P, Grimbacher B, Duerschmied D, Warnatz K. Rescue of cytokine storm due to HLH by hemoadsorption in a CTLA4-deficient patient. J Clin Immunol. 2017;37:273–6.
Castleman VH, Romio L, Chodhari R, Hirst RA, de Castro SCP, Parker KA, et al. Mutations in radial spoke head protein genes RSPH9 and RSPH4A cause primary ciliary dyskinesia with central-microtubular-pair abnormalities. Am J Hum Genet. 2008;84:197–209.
Parta M, Shah NN, Baird K, Rafei H, Calvo KR, Hughes T, et al. Allogeneic hematopoietic stem cell transplantation for GATA2 deficiency using a busulfan-based regimen. Biol Blood Marrow Transplant. 2018;24:1250–9. https://doi.org/10.1016/j.bbmt.2018.01.030.
Lo B, Zhang K, Lu W, Zheng L, Zhang Q, Kanellopoulou C, et al. Patients with LRBA deficiency show CTLA4 loss and immune dysregulation responsive to abatacept therapy. Science (80- ). 2015;349:436–40.
Posey JE, Harel T, Liu P, Rosenfeld JA, James RA, Coban Akdemir ZH, et al. Resolution of disease phenotypes resulting from multilocus genomic variation. N Engl J Med. 2016;376:21–31.
Stoddard JL, Niemela JE, Fleisher TA, Rosenzweig SD. Targeted NGS: a cost-effective approach to molecular diagnosis of PIDs. Front Immunol. 2014;5:531. https://doi.org/10.3389/fimmu.2014.00531
Al-Mousa H, Abouelhoda M, Monies DM, Al-Tassan N, Al-Ghonaium A, Al-Saud B, et al. Unbiased targeted next-generation sequencing molecular approach for primary immunodeficiency diseases. J Allergy Clin Immunol. 2016;137:1780–7.
Moens LN, Falk-Sörqvist E, Asplund AC, Bernatowska E, Smith CIE, Nilsson M. Diagnostics of primary immunodeficiency diseases: a sequencing capture approach. PLoS One. 2014;9:1–15.
Maffucci P, Filion CA, Boisson B, Itan Y, Shang L, Casanova J, et al. Genetic diagnosis using whole exome sequencing in common variable immunodeficiency. Front Immunol. 2016;7:1–9.
Yu H, Zhang VW, Stray-Pedersen A, Hanson IC, Forbes LR, de la Morena MT, et al. Rapid molecular diagnostics of severe primary immunodeficiency determined by using targeted next-generation sequencing. J Allergy Clin Immunol. 2016;138:1–12.
Boisson B, Quartier P, Casanova J-L. Immunological loss-of-function due to genetic gain-of-function in humans: autosomal dominance of the third kind. Curr Opin Immunol. 2015;32:90–105.
Popp MW-L, Maquat LE. Organizing principles of mammalian nonsense-mediated mRNA decay. Annu Rev Genet. 2013;47:139–65.
Hsu AP, Sampaio EP, Khan J, Calvo KR, Lemieux JE, Patel SY, et al. Mutations in GATA2 are associated with the autosomal dominant and sporadic monocytopenia and mycobacterial infection (MonoMAC) syndrome. Blood. 2011;118:2653–5.
Marciano BE, Wesley R, De Carlo ES, Anderson VL, Barnhart LA, Darnell D, et al. Long-term interferon-g therapy for patients with chronic granulomatous disease. Clin Infect Dis. 2004;39:692–9.
Acknowledgements
We thank the patients and their families for the participation in the study. We thank the Radboud Genomics Technology Center, Radboud University Medical Center Nijmegen, for their technical assistance. We furthermore thank all other members of the immuno-genomics group (Radboud University Medical Center) for their contribution.
Funding
AH was supported by the Solve-RD project. The Solve-RD project has received funding from the European Union’s Horizon 2020 research and innovation programme under grant agreement No 779257. MGN was supported by the Nederlandse Organisatie voor Wetenschappelijk Onderzoek (Spinoza grant) and the European Research Council (grant agreement No 310372). JAV was supported by Nederlandse Organisatie voor Wetenschappelijk Onderzoek (918-15-667).
Author information
Authors and Affiliations
Contributions
PA and AH designed the study. AS1, JAV, FLvdV, and MGN helped with the study design. PA performed the formal analysis and investigation under the supervision of AH, JAV, FLvdV, and MGN. EY performed the variant validation and additional exome analysis. AS1, ARM, and PA performed the primary diagnostic exome analysis and generated the original clinical molecular analyses and interpretation of individual patients. CG, JYH-K, SHL, MN, TS, MvdV, and DZ contributed to the exome sequencing analysis. MSAZ, EAI, KJvA, NA, HAAG, HAAJ, AAA-H, FAM, ABA, BA-S, AAA, AA, WB, CPB-R, MvD, MvdF, EHG, MKH, SSH, EPH, SH, CHK, RK-F, KL, MAMK, JM, JtO, JP, PvP, JHMS-H, AS2, MV, AW, GTJvW, EZ-H, WAGvZ-S, EAF, FLvdV, and MGN recruited participants, collected the clinical data, and contributed to the characterization of individual patient phenotypes/genotypes. MSAZ, WAGvZS, JHMS-H, VLvdV, JtO, MvD, and EAF coordinated patient recruitment and cohort assembly. PA and AH wrote the manuscript with contributions by all other authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Patients/families were counseled and provided informed consent in the realm of the diagnostic procedure, written informed consent was obtained from all patients, and our research project was approved by the local ethics committee (Commissie Mensgebonden Onderzoek Regio Arnhem- Nijmegen). All participants provided written informed consent to participate in the study. Families were counseled and provided consent for “PID gene panel only” or “gene panel and exome-wide analysis” as presented here. The research conforms to the principles of the Declaration of Helsinki.
Consent for publication
All individuals involved in this study provided consent for publication. We also obtained consent to publish the clinical information of all individuals presented in this study.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Table S1. Overview of all clinical characteristics of the patients included in our diagnostic PID cohort, including all immunophenotype characteristics. (XLSX 63 kb)
Additional file 2:
Table S2. Shows all causative mutations identified in 72 patients from 68 families suffering from primary immunodeficiencies. (XLSX 17 kb)
Additional file 3:
Table S3. Variants of unknown significance (class 3) and variants in TRAF3 identified in 17 patients suffering from primary immunodeficiencies. (XLSX 11 kb)
Additional file 4:
Table S4. (A) The number of patients with isolated or combined infections, and (B) the number of patients with isolated or combined immunophenotypes, and the percentage for which we have reported a genetic diagnosis. (XLSX 11 kb)
Additional file 5:
Table S5. Quality information of the WES technology, with the mean target coverage, and the % of bases with > 20× coverage. (XLSX 22 kb)
Additional file 6:
Table S6. Information on all large > 5-Mb homozygous regions per patient, detected in the exome. Of each region, the genomic location, size, % homozygous variants, and the detected mutation are provided. (XLSX 158 kb)
Additional file 7:
Additional material and references. (DOCX 31 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Arts, P., Simons, A., AlZahrani, M.S. et al. Exome sequencing in routine diagnostics: a generic test for 254 patients with primary immunodeficiencies. Genome Med 11, 38 (2019). https://doi.org/10.1186/s13073-019-0649-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13073-019-0649-3