Abstract
Background
Juvenile Idiopathic Arthritis (JIA) may cause significant impairment in health-related quality of life (HrQoL), despite effective therapies. The aim of this study was to assess HrQoL during first-year treatment in patients with new-onset polyarticular JIA, and to compare treatment strategies.
Methods
In ACUTE-JIA Study, 60 patients with new-onset JIA were randomized to receive either infliximab with methotrexate (IFX+MTX); a triple therapy of methotrexate, hydroxychloroquine, and sulfasalazine (Triple); or methotrexate monotherapy (MTX). Efficacy was measured with American College of Rheumatology pediatric (ACRp) score, and juvenile arthritis disease activity score (JADAS). HrQoL was evaluated with Child Health Questionnaire (CHQ), which includes physical and psychosocial summary scores (PhS and PsS). Linear mixed models were utilized to compare groups over time.
Results
In the whole group of 60 patients, mean physical summary score (PhS) improved from 26.2 (SD 8.7) at week 0 to 49.7 (SD 13.2) at week 54 (p=0.046). Mean improvement of PhS was 20.3 (95% CI -15.5 to 56.2); 22.6 (-19.5 to 64.7); and 26.6 (-12.1 to 65.3) in IFX+MTX, Triple, and MTX, respectively. Changes in psychosocial summary score (PsS) were smaller: from 51.0 (SD 8.5) to 54.7 (6.3) (p=0.019) in all patients. No differences between the three treatment groups were detected in either of the measures. In multivariate analyses, Child Health Assessment Questionnaire (CHAQ), pain VAS, and time spent in inactive disease contributed to improvement in PhS; gender and CHAQ to PsS.
Conclusions
HrQol improved during the first year on therapy for JIA irrespective of the treatment strategy. The timing of change in the different dimensions of HrQoL varied; improvement occurred earlier in physical than psychosocial domains of HrQol.
Trial registration
This study was registered within the Hospital District of Helsinki and Uusimaa (http://www.hus.fi) clinical trials, number 211864 in October 2002, and later on with ClinicalTrials.gov, number NCT01015547.
Similar content being viewed by others
Background
Juvenile idiopathic arthritis (JIA) is a chronic condition, which may cause disability and functional impairment. JIA is treated with non-steroidal anti-inflammatory drugs, synthetic disease-modifying anti-rheumatic drugs (DMARDs), glucocorticoid injections, and in refractory disease, with biologic drugs.
Health-related Quality of Life (HrQoL) is a multi-dimensional health outcome concept, which takes into account perspectives of well-being, physical health, and psychological state, as well as the surrounding culture and environment [1]. In health technology assessments of new treatment approaches, HrQoL is an important component in the measurement of efficacy. In JIA, baseline HrQoL seems to have an independent role in predicting disease activity and functional disability [2].
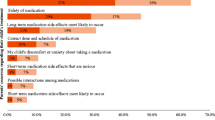
Patients with JIA often have impaired HrQoL [3]. On the other hand, effective therapies targeting disease activity have improved HrQoL [4]. Besides disease activity, other factors such as pain, disability, and burden of medication can affect HrQoL [5].
In patients with new-onset JIA, only a few studies have evaluated the effects of treatment on HrQoL. In a recent german inception cohort, psychosocial health reached the level of normal population at 18 months from onset, whereas a significant difference in physical health remained [4]. Disease activity, functional disability [4, 6], parent or patient global assessment of wellbeing, and pain [4] seem to play a major role in HrQoL. Yet it is not known how safety and efficacy of different medications affect HrQoL.
In this study, we aimed to assess HrQoL during the first-year of early aggressive treatment in patients with polyarticular JIA, and the impact of different treatments on HrQoL.
Methods
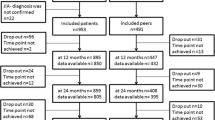
This study was part of the ACUTE-JIA Study, in which sixty patients with new-onset polyarticular JIA were randomized into three treatment arms: infliximab with methotrexate (IFX+MTX); a combination of methotrexate, hydroxychloroquine, and sulphasalazine (Triple), or methotrexate monotherapy (MTX). Study protocol has been described in detail previously [7]. In brief, patients entered the trial very early in the disease course, less than 6 months from disease onset. During the first year, patients underwent altogether eight study visits. During the first year, patients underwent altogether eight study visits. At these visits, disease activity was measured with American College of Rheumatology pediatric (ACRp) scores, and juvenile arthritis activity score (JADAS). Medication was adjusted according to the study protocol, aiming to a minimum of ACRp 30 improvement. At seven visits (weeks 0, 6, 12, 24, 36, 48, and 54) HrQoL was measured with parents’ proxy reports on Child Health Questionnaire (CHQ)-PF50. Pain was measured on a visual analog scale (0-100 mm). The preliminary Wallace criteria [8] were used to define clinically inactive disease (CID). Intra articular corticosteroids (GCs) were allowed as symptomatic treatment, whereas systemic GCs were not allowed.
CHQ is an international, validated, and generic HrQoL survey. CHQ-PF50 has 50 questions that together produce 15 health concepts (Global Health, Physical Functioning, Role/Social Limitations - Emotional/Behavioral or Physical, Bodily Pain/Discomfort, Behavior, Global Behavior Item, Mental Health, Self Esteem, General Health Perceptions, Change in Health, Parental Impact -Emotional or Time, Family Activities and Cohesion), each producing values between 0-100. It also constitutes two summary scores Physical Summary Score (PhS), and Psychosocial Summary Score (PsS), which have been standardized with a linear T-score transformation (mean 50; one standard deviation of age and sex matched healthy children is 10, changes of 5 or 8 are considered moderate or large). In a normal U.S. population sample, mean PhS is 53.0 (SD 8.8), and PsS 51.2 (SD 9.1) Higher scores indicate for better health [9].
The CHQ values were calculated as advised by the publisher [9]. For missing items, scores were imputed if at least half of the items in the scale were completed, as advised. For patients who discontinued medication, the last observation on intended treatment was carried forward.
Statistical analyses
Differences between groups at baseline were tested with one-way analysis of variance, Kruskal-Wallis test, or Chi square, as appropriate. Paired samples t-test was used to test differences in summary scores between time points. A linear mixed model was developed to investigate changes in summary scores over time, and contributing factors. First, demographic and variables related to treatment and disease activity were selected to perform separate univariate analyses. Second, significant variables were used in the final linear mixed model.
IBM SPSS Statistics Version 24 (IBM Corp., Armonk, NY, USA) was used for all statistical analyses.
Results
Parents of all 60 patients filled the CHQ in the beginning of the study. Of these, 20 patients remained on intended treatment on IFX+MTX, 16 on Triple, and 11 on MTX. Patients in IFX+MTX achieved and remained in inactive disease more often than in other groups. Differences between Triple and MTX were not statistically significant (7). Patients in MTX had more infections and transient elevations of liver enzymes than in other groups. Nausea was more common in Triple. 3 patients in Triple and 8 in MTX discontinued due to inefficacy, one patient in Triple and one in MTX due to an adverse event. At baseline, compared with other treatment groups, patients on IFX+MTX had lower CHAQ, JADAS, and pain. PhS and PsS levels were similar in all treatment groups. (Table 1)
Mean (SD) PhS at week 54 was 49.9 (15.5) on IFX+MTX; 49.9 (12.0) on Triple; and 49.3 (12.9) on MTX, (p=0.98). Changes in PhS in the total cohort were significant between weeks 0 to 6 (p= 0.023); 6 to 12 (p=0.020); and 12 and 24 (p=0.004) (Figure 1). Mean PsS at week 54 was 54.9 (6.0) on IFX+MTX; 55.0 (6.8) on Triple; and 54.1 (6.3) on MTX, (p=0.89). There were no significant changes between consecutive weeks, but scores at weeks 24, 36, 48, and 54 were significantly higher than at week 0. (Fig. 1a and b)
In the mixed model, Child Health Assessment Questionnaire (CHAQ), pain, and cumulative time spent in CID prior to each study visit contributed significantly to PhS values (Table 2). For PsS, gender and CHAQ remained significant contributors in the mixed model (Table 3).
Of the single domains of HrQoL; bodily pain (BP), role or social limitations due to physical reasons (RP), physical functioning (PF), global health perception (GH), and parental emotional impact (PE) differed from normal population at week 0. Other domains did not differ from normal population. At week 54, patients reached normal population in other domains, except GH (Fig. 1c)
Discussion
In the present intention-to-treat analysis of new-onset polyarticular JIA, HrQoL improved irrespective of the treatment strategy, although the timing of change in the dimensions of HrQoL varied. This suggests that early aggressive treatment of JIA either with biologics or synthetic DMARDs makes it possible to control imminent impairment of HrQoL.
Physical condition improved soon after the onset of aggressive therapy, simultaneously with the decrease in disease activity. In a recent study from Canada, improvement in HrQoL occurred later than in other disease outcome measures, several years after improvement of disease activity [5]. However, in that study only 10% of patients received biologics. In the current study, each of CHAQ, pain VAS, and time spent in CID were associated with improvement in physical condition. This underlines the significance of controlling disease activity to ensure good quality of life.
The changes of psychosocial condition in this study were minor, and significant improvement over time compared to the situation at onset of therapy could not be seen until week 24. Usually, psycho-social components of QoL have been affected to lesser extent than physical components [3, 4]. In line with the present study, previous studies utilizing CHQ or SF-36 have found only small changes in PsS [10]. In a recent study on abatacept, measured with CHQ, patients with JIA reported better PsS values than healthy normal population, already in the beginning of treatment [11].
In this study, the subdomain parental emotional impact remained below normal population at the end of the first year. Measurements in this study were parent proxy-reports, which however have shown similarities [12] with the juvenile patients’ self-reporting. In a previous study on patients with new-onset polyarticular JIA, parental emotional scores have been a significant predictor of proxy-reported HrQoL [4]. These findings indicate that it is important to pay attention to parents’ emotions to enable holistic approach for patient care in JIA.
In this study, pain contributed to physical aspects of QoL. This was also demonstrated previously [3, 4, 13]. This suggests that instead of HrQoL questionnaires with multiple items, pain VAS could possibly be used in clinical work as a rapid tool to assess patient’s well-being.
In long-term follow-up studies, patients with JIA have shown poorer HrQoL than their peers, even despite their low disease activity [6, 10]. One reason for this might be the less effective treatment available at the time of disease onset of these studies. The current study demonstrated that despite the differences in the safety and efficacy profiles of biologics and DMARDs [14, 15], these treatments are equal in improving HrQoL, when used in a treat-to-target manner.
A limitation of this study was the small sample size, which decreased the power to detect differences between treatment groups. Despite the fact that there were differences in the efficacy (IFX +MTX was more effective than other treatments), no differences were detected in the evolution of HrQoL. This might be due to the small sample size, and the differences at baseline. HrQoL was measured during the first year from disease onset. Longer follow-up time may be needed to reveal the effects of early aggressive therapy and other contributing factors on HrQoL. The effects of non-medical conditions, such as social support and school absence, were not measured.
To the best of our knowledge, this is the first study comparing HrQoL between biologic and synthetic DMARD therapy. In the future, a long-term follow-up study on HrQoL, assessing the effects of early aggressive treatment and factors associated with HrQoL might direct treatment decisions towards better patient-reported outcomes.
Conclusions
In conclusion, quality of life improved in all treatment groups during the first year from onset of polyarticular JIA. Despite their different efficacy and safety profiles, infliximab and synthetic DMARDs, when used early and aggressively, were effective in improving health-related quality of life.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ACRp:
-
American College of Rheumatology pediatric (score)
- BP:
-
Bodily pain
- CHAQ:
-
Child health assessment questionnaire
- CHQ:
-
Child health questionnaire
- CID:
-
Clinically inactive disease
- DMARDs:
-
Disease-modifying anti-rheumatic drugs
- GH:
-
General health perceptions
- HrQoL:
-
Health-related quality of life
- JADAS:
-
Juvenile arthritis disease activity score
- JIA:
-
Juvenile Idiopathic Arthritis
- PE:
-
Parental emotional impact
- PF:
-
Physical functioning
- PF-50:
-
Patient form 50
- PhS:
-
Physical summary score
- PsS:
-
Psychosocial summary score
- RP:
-
Role or social limitations due to physical reasons
- SF-36:
-
Short form health survey
- VAS:
-
Visual analogue scale
References
Wilson IB, Cleary PD. Linking clinical variables with health-related quality of life. A conceptual model of patient outcomes. JAMA. 1995;4(273):59–65.
Oen K, Tucker L, Huber AM, Miettunen P, Scuccimarri R, Campillo S, et al. Predictors of early inactive disease in a juvenile idiopathic arthritis cohort: results of a Canadian multicenter, prospective inception cohort study. Arthritis Rheum. 2009;61(8):1077–86.
Wipff J, Sparsa L, Lohse A, Quartier P, Kahan A, Deslandre CJ. Impact of juvenile idiopathic arthritis on quality of life during transition period at the era of biotherapies. Joint Bone Spine. 2016;83(1):69–74.
Listing M, Monkemoller K, Liedmann J, Niewerth M, Sengler C, Listing J. et al. The majority of patients with newly diagnosed juvenile idiopathic arthritis achieve a health-related quality of life that is similar to that of healthy peers: results of the German multicenter inception cohort (ICON). Arthritis Res Ther 2018; 20(1):106,018-1588-x.
Oen K, Guzman J, Dufault B, Guzman J, Lim H, Lee C, et al. Health-Related Quality of Life in an Inception Cohort of Children With Juvenile Idiopathic Arthritis: A Longitudinal Analysis. Arthritis Care Res (Hoboken). 2018;70(1):134–44.
Seid M, Opipari L, Huang B, Brunner HI, Lovell DJ. Disease control and health-related quality of life in juvenile idiopathic arthritis. Arthritis Rheum. 2009;61(3):393–9.
Tynjala P, Vahasalo P, Tarkiainen M, Kroger L, Aalto K, Malin M, et al. Aggressive combination drug therapy in very early polyarticular juvenile idiopathic arthritis (ACUTE-JIA): a multicentre randomised open-label clinical trial. Ann Rheum Dis. 2011;70(9):1605–12.
Wallace CA, Ruperto N, Giannini E. Preliminary criteria for clinical remission for select categories of juvenile idiopathic arthritis. J Rheumatol. 2004;31(11):2290–4.
Child Health Questionnaire (CHQ). Scoring and Interpretation Manual. Cambridge, MA 02141: HealthActCHQ, Inc., 2008.
Tollisen A, Selvaag AM, Aulie HA, Lilleby V, Aasland A, Lerdal A, et al. Physical Functioning, Pain, and Health-Related Quality of Life in Adults With Juvenile Idiopathic Arthritis: A Longitudinal 30-Year Followup Study. Arthritis Care Res (Hoboken). 2018;70(5):741–9.
Lovell DJ, Ruperto N, Mouy R, Paz E, Rubio-Perez N, Silva CA, et al. Long-term safety, efficacy, and quality of life in patients with juvenile idiopathic arthritis treated with intravenous abatacept for up to seven years. Arthritis Rheumatol. 2015;67(10):2759–70.
Brunner HI, Klein-Gitelman MS, Miller MJ, Trombley M, Baldwin N, Kresset A, et al. Health of children with chronic arthritis: relationship of different measures and the quality of parent proxy reporting. Arthritis Rheum. 2004;51(5):763–73.
Shiff NJ, Tupper S, Oen K, Guzman J, Lim H, Lee CH, et al. Trajectories of pain severity in juvenile idiopathic arthritis: results from the Research in Arthritis in Canadian Children Emphasizing Outcomes cohort. Pain. 2018;159(1):57–66.
Klotsche J, Minden K, Niewerth M, Horneff G. Time spent in inactive disease before MTX withdrawal is relevant with regard to the flare risk in patients with JIA. Ann Rheum Dis. 2018;77(7):996–1002.
Tarkiainen M, Tynjala P, Vahasalo P, Lahdenne P. Occurrence of adverse events in patients with JIA receiving biologic agents: long-term follow-up in a real-life setting. Rheumatology (Oxford). 2015;54(7):1170–6.
Acknowledgements
The authors wish to thank the other members in Acute-JIA study group: Merja Malin, Tampere; Anne Putto-Laurila, Turku; Visa Honkanen, Helsinki; Katarina Rebane, Helsinki; and Eija Piippo-Savolainen, Kuopio.
Funding
For this work, MT has received grants from The Finnish Cultural Foundation, The Finnish Medicine Foundation, and The Finnish Foundation for Research in Rheumatic Diseases.
Author information
Authors and Affiliations
Contributions
PT, PV, KA, LK, and PL contributed to study conception and design; MT, PT, PV, KA and LK contributed to acquisition of data; MT, PT and PL contributed to analysis and interpretation of data. MT was major contributor in writing manuscript. All authors contributed in revising and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethical approval was obtained from the coordinating ethical committee of Helsinki University Central Hospital. The study was registered within the Hospital District of Helsinki and Uusimaa (http://www.hus.fi) clinical trials, number 211864, and later on to ClinicalTrials.gov, number NCT01015547. A written consent to participate was obtained from parents and patients.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tarkiainen, M., Tynjälä, P., Vähäsalo, P. et al. Health-related quality of life during early aggressive treatment in patients with polyarticular juvenile idiopathic arthritis: results from randomized controlled trial. Pediatr Rheumatol 17, 80 (2019). https://doi.org/10.1186/s12969-019-0370-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12969-019-0370-1