Abstract
Background
The low cost of thiazolidinediones makes them a potentially valuable therapeutic option for the > 300 million economically disadvantaged persons worldwide with type 2 diabetes mellitus. Differential selectivity of thiazolidinediones for peroxisome proliferator-activated receptors in the myocardium may lead to disparate arrhythmogenic effects. We examined real-world effects of thiazolidinediones on outpatient-originating sudden cardiac arrest (SCA) and ventricular arrhythmia (VA).
Methods
We conducted population-based high-dimensional propensity score-matched cohort studies in five Medicaid programs (California, Florida, New York, Ohio, Pennsylvania | 1999–2012) and a commercial health insurance plan (Optum Clinformatics | 2000–2016). We defined exposure based on incident rosiglitazone or pioglitazone dispensings; the latter served as an active comparator. We controlled for confounding by matching exposure groups on propensity score, informed by baseline covariates identified via a data adaptive approach. We ascertained SCA/VA outcomes precipitating hospital presentation using a validated, diagnosis-based algorithm. We generated marginal hazard ratios (HRs) via Cox proportional hazards regression that accounted for clustering within matched pairs. We prespecified Medicaid and Optum findings as primary and secondary, respectively; the latter served as a conceptual replication dataset.
Results
The adjusted HR for SCA/VA among rosiglitazone (vs. pioglitazone) users was 0.91 (0.75–1.10) in Medicaid and 0.88 (0.61–1.28) in Optum. Among Medicaid but not Optum enrollees, we found treatment effect heterogeneity by sex (adjusted HRs = 0.71 [0.54–0.93] and 1.16 [0.89–1.52] in men and women respectively, interaction term p-value = 0.01).
Conclusions
Rosiglitazone and pioglitazone appear to be associated with similar risks of SCA/VA.
Similar content being viewed by others
Background
Type 2 diabetes mellitus (DM) disproportionally affects persons of moderate to limited economic means [1]. Among the ~ 60% of the United States (US) population with a personal annual income < $48,000 [2], DM prevalence is 13–19%—2- to 3-fold greater than in persons with higher incomes [3]. From a global perspective, DM affects > 335 million residents of middle- to low-income countries [4] and its prevalence is increasing most rapidly in these nations [5]. Therefore, it is unsurprising that the World Health Organization deems cost a critical factor in type 2 DM treatment personalization [6]. In alignment with this, the American Diabetes Association and European Association for the Study of Diabetes has tailored guidelines [7] for cost-sensitive type 2 DM patients. Thiazolidinediones—generically available, low-cost insulin-sensitizing agents—are among the preferred add-ons to metformin for such patients without atherosclerotic cardiovascular or chronic kidney diseases. This highlights the continued role of thiazolidinediones in a practitioner’s toolkit of pharmacologic type 2 DM treatments.
Differential selectivity of thiazolidinediones for peroxisome proliferator-activated receptors in the myocardium may account for potential disparate effects on major cardiovascular events [8]. Numerous trials and meta-analyses have investigated relationships between thiazolidinediones and acute myocardial infarction (AMI) [9], stroke [9], dyslipidemia [10], left ventricular mass [11], heart failure [12], cardiovascular death [12], and all-cause death [13], as examples. To our knowledge, there have been no prior population-based studies of sudden cardiac arrest (SCA) and ventricular arrhythmia (VA). Such an investigation is warranted since high dose rosiglitazone may inhibit human ether-a-go-go-related gene (hERG) potassium channels (a surrogate for delayed cardiac repolarization [14]) in a human cell line [15]. Filling this knowledge gap is important because thiazolidinediones remain commonly used [16], may have synergistic effects with newer antidiabetic drugs [17], and may be repurposed for cancer [18, 19], neurodegenerative disorders [19], pulmonary arterial hypertension [20], fatty liver disease [19, 21], nephrotic syndrome [22], and secondary prevention of stroke [23]. Forthcoming trials examining thiazolidinediones and clinical sequelae of arrhythmogenicity are extremely unlikely given the futility of the TOSCA.IT trial [24] and the pharmacologic class’ lack of market exclusivity [16].
We therefore set forth to examine the relationship between individual thiazolidinediones and outpatient-originating SCA and VA.
Methods
Overview and study populations
We conducted high-dimensional propensity score (hdPS)-matched observational cohort studies to examine the risk of SCA/VA among new users of thiazolidinediones. The study included adults aged 30–75 years. Younger persons were excluded because SCA/VA is extremely rare in such individuals and unlikely to be due to prescription drugs [25]. Older persons were excluded to minimize concern for significant competing comorbidities that may mimic SCA/VA. The cohort consisted exclusively of person-time exposed to rosiglitazone or pioglitazone. Data included demographic, enrollment, and healthcare claims from the US Medicaid programs of California, Florida, New York, Ohio, and Pennsylvania from 1999 to 2012. These states comprise ~ 40% of the national Medicaid population, with the 14-year dataset recording the experience of nearly 70 million cumulative enrollees. Because many Medicaid beneficiaries are co-enrolled in the US Medicare program, we also obtained Medicare claims to ascertain a more complete picture of enrollees’ healthcare [26, 27]. We linked these datasets to the US Social Security Administration Death Master File to supplement dates of death with those provided by the US Centers for Medicare and Medicaid Services (CMS). For purposes of conceptual replication and robustness [28,29,30], and consistency with good practice for generating real-world evidence [31], we secondarily addressed this study question and examined the same estimands in an independent, 17-year US commercial health insurance dataset (Optum Clinformatics Data Mart, 2000–2016).
Defining the cohort
Persons under study were apparent new users of a thiazolidinedione, i.e., had a 12-month baseline period devoid of a thiazolidinedione dispensing (including troglitazone [32] for 1999–2000). Cohort entry occurred upon an incident rosiglitazone or pioglitazone dispensing. The following 12-month baseline events served to exclude observations from study: (a) interruption in insurance benefit enrollment; and/or (b) SCA or VA diagnosis in an emergency department, inpatient, or ambulatory setting. We used the latter exclusion criterion to maximize the identification of incident outcomes described below. Persons with excluded observations could later be eligible for inclusion if subsequently meeting the above criteria; yet, once included, a person could not contribute second or later observations.
Follow-up began at cohort entry and continued until the first occurrence of a/an: (a) SCA or VA diagnosis, regardless of whether or not it met the outcome definition described below; (b) death (CMS only, since not recorded in Optum); (c) > 15-day gap in therapy for the cohort-defining thiazolidinedione; (d) dispensing of a thiazolidinedione different than that upon cohort entry (i.e., indicative of switching within pharmacologic class); (e) dispensing of a drug with a known risk of torsade de pointes; [33] (f) insurance benefit disenrollment; or (g) end date of the dataset. Although hospitalization was not a censoring event, we excluded follow-up time during a hospitalization to minimize immeasurable time bias [34].
Exposure and covariate ascertainment
The thiazolidinedione dispensed on the day of cohort entry defined exposure. We did not study troglitazone given its US market withdrawal in 2000 [32]. To minimize the potential for selection bias and confounding by indication and other unmeasured subject characteristics [35], we did not study thiazolidinedione-unexposed persons. We selected pioglitazone as the active comparator referent since it: (a) is unlikely to prolong (although may shorten [36]) the electrocardiographic QT interval; [33] (b) is a predicted non-inhibitor of the human ether-a-go-go-related gene; [37] and (c) was utilized more frequently in these datasets, an important consideration for pairwise propensity score matching [38].
Potential confounders included prespecified and empirically identified baseline variables, both of which informed the propensity score. Prespecified variables included demographics, measures of intensity of healthcare utilization (e.g., numbers of prescription drugs used, healthcare provider visits, hospitalizations) [39], measures of socioeconomic status (Optum only), drug exposures, and comorbidities (Additional file 1: Table S1). Empiric variables were identified by a high-dimensional approach [40, 41] which ranks and selects potential confounders or proxies thereof based on their observed associations with exposure and outcome (see specifications in Additional file 1: Table S2).
Outcome ascertainment
The outcome of primary interest was an incident outpatient-originating SCA/VA event precipitating hospital presentation—consistent with our aim to study the serious arrhythmogenic effects of thiazolidinediones in an ambulatory population. The rationale for a composite outcome is that SCA events are generally considered undocumented arrhythmias (i.e., sudden and presumed arrhythmic) [42]. We identified outcomes in emergency department or hospital claims having at least one discharge diagnosis code of interest (Additional file 1: Table S3) in the principal or first-listed position (indicative of the reason for presentation/admission) without regard to discharge disposition. The International Classification of Diseases, 9th Revision, Clinical Modification (ICD-9-CM) component of this algorithm was validated against primary medical records in a Medicaid population. These diagnoses had a positive predictive value (PPV) ~ 85% for identifying outpatient-originating SCA/VA [43]. The rationale for not using death certificate causes of death is that they have a poor PPV for identifying sudden death [44]. The rationale for not studying inpatient-originating SCA/VA is that: (a) oral antidiabetic drugs are rarely utilized in the inpatient setting; [45] (b) arrhythmogenic events occurring during hospitalizations are often attributable to causes other than ambulatory drug exposures; and c) CMS and Optum data, like most claims datasets, do not record inpatient drug exposures [46].
The outcome of secondary interest was the subset of primary events that were fatal, i.e., sudden cardiac death (SCD) or fatal VA. Operationally, this was defined as having died the day of or the day after the healthcare encounter defining the event.
Statistical analysis
We calculated descriptive statistics for baseline variables, crude incidence rates, and unadjusted association measures, the latter via Cox proportional hazards models. We utilized a semi-automated, data-adaptive hdPS approach—an algorithm for identifying and selecting proxies for important confounder constructs [47]—to reduce the impact of measured and unmeasured potential confounders that are correlated with measured factors [48]. First, we used the hdPS algorithm [41, 47] to identify empiric candidate covariates; we identified the 200 most prevalent baseline diagnoses, procedures, and dispensed drugs for each of nine prespecified data dimensions. Second, within each dimension, we ranked candidates based on their potential for bias by assessing each variable’s prevalence and univariate association with exposure and outcome according to the Bross formula [49, 50]. Third, we used these associations to select 500 empiric covariates for inclusion in the propensity score. We also included in the propensity score: demographics; measures of intensity of healthcare utilization; [51] and investigator-prespecified covariates meeting the disjunctive cause criterion (Additional file 1: Table S1) [52]. We assessed covariate balance between thiazolidinedione groups using standardized differences [53]. Fourth, we used logistic regression to calculate propensity scores, defined as a subject’s predicted probability of receiving rosiglitazone vs. pioglitazone. Fifth, we paired rosiglitazone to pioglitazone users (1:1) on propensity score using nearest-neighbor caliper (width = 0.2 standard deviations of the logit of the propensity score) matching without replacement; matching began with study subjects in a random order [54]. Sixth, we generated Kaplan–Meier curves and compared their equality using a stratified log-rank test [38]. Finally, we generated marginal hazard ratios (HRs) via Cox proportional hazards regression that adjusted for calendar time and used a robust variance estimator to account for clustering within matched pairs [38, 55]. We assessed proportional hazards assumptions via inclusion of an interaction term of exposure by time.
We conducted numerous secondary analyses (e.g., dose–response) to assess the robustness of our primary findings (Additional file 1: Table S4). Primary and secondary analyses were conducted using SAS v9.4 (SAS Institute Inc.: Cary, NC). The University of Pennsylvania institutional review board approved this research.
Role of the funding sources
Neither the American Diabetes Association nor the US National Institutes of Health had a role in the study’s conduct or interpretation.
Results
Cohort characteristics and outcome frequencies|Medicaid
In the Medicaid dataset, we identified 294,324 and 205,767 new users of pioglitazone and rosiglitazone, respectively. Additional file 1: Table S5 and Figure S1 display their baseline characteristics. Overall, users were predominantly female (62.2%) and non-Hispanic white (34.9%), with a median age of 58.7 years. Large proportions of users had pre-existing hypertension (65.2%), dyslipidemia (50.2%), depression (26.1%), and ischemic heart disease (23.4%). Small proportions of users had pre-existing cardiomegaly (5.7%), a cardiac conduction disorder (1.9%), and a congenital cardiac anomaly (1.6%). Few users experienced a prior serious hypoglycemic episode (2.8%).
Users contributed 184,664 person-years (p-y) of follow-up, during which we identified 528 SCA/VA outcomes (crude incidence rate = 2.86 [95% confidence interval: 2.62–3.11] per 1000 p-y), 273 (51.7%) of which were fatal. See Additional file 1: Figure S2 for the Kaplan–Meier curve. In the secondary analysis limited to the first 30 days of follow-up, we identified 215 SCA/VA outcomes during 35,592 p-y of follow-up (crude incidence rate = 6.04 [5.26–6.90] per 1000 p-y). Crude incidence rates for SCD/fatal VA were 1.48 (1.31–1.66) and 3.26 (2.69–3.91) per 1000 p-y in all follow-up time and limited to the first 30 days of follow-up, respectively. These incidence rates are similar to prior findings in persons with DM [56,57,58].
Effect estimates: primary analysis|Medicaid
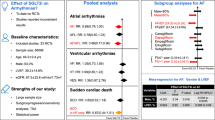
The propensity score model included 560 covariates—60 prespecified and 500 empirically identified by the hdPS algorithm (Additional file 1: Table S6). Using logits of propensity scores, we matched 189,799 rosiglitazone users (92.2% of available population) to an equal number of pioglitazone users (NTotal = 379,598). Additional file 1: Figure S3 depicts near-perfect overlap in propensity score distributions post-matching. Figure 1 presents the Kaplan–Meier curve in the matched sample. Table 1 presents unadjusted HRs. Table 1 and Fig. 2 present adjusted marginal HRs. Notably, the hazard of SCA/VA for rosiglitazone (vs. pioglitazone) was consistent with the null (adjusted marginal HR = 0.91 [0.75–1.10]).
Kaplan–Meier curve depicting the probability of sudden cardiac arrest/ventricular arrhythmia upon new use of rosiglitazone vs. pioglitazone, limited to the propensity score-matched sample in Medicaid (N = 379,598). Solid line is pioglitazone. Dashed line is rosiglitazone. p-value for stratified log-rank test = 0.75
Confounder-adjusted marginal hazard ratios for rosiglitazone (vs. pioglitazone) exposure and primary and secondary outcomes, by dataset | Medicaid and Optum. HR hazard ratio. Squares depict hazard ratios for the primary outcome of sudden cardiac arrest and ventricular arrhythmia. The circle depicts a hazard ratio for the secondary outcome of sudden cardiac death and fatal ventricular arrhythmia. * Optum was the prespecified conceptual replication dataset. Its analyses were limited to the primary outcome since the dataset does not document deaths
Effect estimates: secondary analyses|Medicaid
Effect estimates from secondary analyses of the Medicaid dataset (Table 2) were consistent with the primary finding. We found treatment effect heterogeneity by sex (adjusted marginal HR among men = 0.71 [0.54–0.93], among women = 1.16 [0.89–1.52], interaction term p-value = 0.01). Other secondary analyses examining high-risk subgroups did not meet the prespecified threshold for statistical significance. Further, we did not identify dose–response relationships (Additional file 1: Figure S4).
Conceptual replication [28,29,30]|Optum
In the Optum dataset, we identified 190,226 and 103,834 new users of pioglitazone and rosiglitazone, respectively. In contrast to Medicaid, users in Optum were predominantly male (56.5%), had a higher burden of dyslipidemia (60.6%), and had lower burdens of depression (13.8%), ischemic heart disease (13.3%), and prior serious hypoglycemia (0.6%). The crude incidence rate of SCA/VA was 1.41 (1.21–1.64) per 1000 p-y, approximately half the rate estimated among Medicaid enrollees. Consistent with our Medicaid finding, the hazard of SCA/VA for rosiglitazone (vs. pioglitazone) was consistent with the null (adjusted marginal HR = 0.88 [0.61–1.28]). Unlike in Medicaid, we did not find treatment effect heterogeneity by sex (interaction term p-value = 0.96). Further, we did not identify dose–response relationships (Additional file 1: Figure S5).
Discussion
This post-market comparative safety study using real-world healthcare data is the first to estimate effects of thiazolidinediones on SCA/VA as a stand-alone endpoint. The crude incidence rate of SCA/VA among thiazolidinedione users (2.86 per 1000 p-y) reported herein is less than we previously found among sulfonylurea users (3.57 per 1000 p-y); [58] this may be partly driven by different rates of serious hypoglycemia between these pharmacologic classes [59, 60]. Our overall finding of no difference in SCA/VA between new users of rosiglitazone vs. pioglitazone (adjusted marginal HR = 0.91) was robust across numerous secondary analyses and conceptually replicated in an independent dataset (adjusted marginal HR = 0.88). This null finding aligns with a human cell biology study demonstrating that rosiglitazone’s inhibition of hERG (a putative SCA surrogate [14]) is limited to supratherapeutic doses (half maximal inhibitory concentration ~ 9- to 19-fold therapeutic human plasma concentration) [15]. Interestingly, our examination of potential effect modifiers found potential SCA differences by sex among Medicaid, but not Optum, enrollees. The Medicaid finding is consistent with prior reports of sex-based heterogeneity in thiazolidinedione effects, including on hemoglobin A1c, weight gain, edema, and AMI [61, 62].
SCA is a common and growing problem in type 2 DM given the interrelatedness of abnormalities in glucose/insulin homeostasis, dyslipidemia, coronary atherosclerosis, myocardial fibrosis, and QT interval prolongation [57]. In this population, 70% of deaths are attributed to cardiovascular disease, half of which are SCAs [63]. Saxagliptin assessment of vascular outcomes recorded in patients with diabetes mellitus–thrombolysis in myocardial infarction 53 (SAVOR–TIMI 53) data suggest that hemoglobin A1c is a unique predictor of sudden cardiac, but not other, deaths [64]. Therefore, insulin-sensitizing, glucose-lowering, and/or pleiotropic effects of antidiabetic medications may reduce risks of cardiovascular morbidity and mortality. Despite early reports of beneficial effects on atherosclerotic processes, cardiovascular sequelae of thiazolidinediones remain incompletely understood [11, 24, 65, 66]. Despite rosiglitazone’s fall from favor [67], our examination remains clinically relevant given (a) reassuring findings on cardiovascular death, AMI, and stroke endpoints from a re-analysis of RECORD; [68] and (b) its lack of an association with bladder cancer [69].
Among all potential cardiovascular effects, we investigated SCA/VA given the paucity of data on the topic. The recently terminated TOSCA.IT pragmatic trial attempted to compare sudden death in concomitant users of metformin and pioglitazone, but was underpowered [24]. A cohort study using i3 (now Optum) data examined sudden death as part of a composite secondary endpoint with rosiglitazone vs. pioglitazone, but did not report sudden death specific findings [70]. The following biologic underpinnings supported our decision to elucidate within-pharmacologic class SCA/VA risks and thereby created clinical equipoise. First, a molecular biology study found that high-dose rosiglitazone but not pioglitazone [36] inhibited hERG [15]. Second, rosiglitazone lacks pioglitazone’s favorable actions on lipids, serum measures of which are evident within the first 4 weeks of therapy [71]. Despite these apparent distinctions, we found no overall difference in SCA/VA risk between new users of rosiglitazone and pioglitazone.
Motivated by prior findings that sex may alter risk–benefit considerations among thiazolidinedione users [62], we prespecified, examined, then observed effect modification by sex in Medicaid enrollees. Among men, SCA/VA risk was 29% lower among new users of rosiglitazone vs. pioglitazone; the finding among women was consistent with a null association. The potential differential risk by sex, if real, may be at least partly explained by differential responses to thiazolidinediones (e.g., via hormonal mechanisms, peroxisome proliferator-activated receptor expression) [72], hypoglycemia rates [73], and cardiovascular effects [74], as examples. The apparent protective association for rosiglitazone in men may be explained by its less potent effect on plasma glucose [75], subsequent titration to higher doses, and lower rates of serious hypoglycemia at these doses [59], all vs. pioglitazone, for example. Further investigation of this result is prudent, especially since our sex finding did not replicate in Optum enrollees.
Our study has notable strengths. It is the first population-based study to examine the relationship between thiazolidinediones and SCA/VA. Such results are not forthcoming from ongoing trials and, given the futility of TOSCA.IT, are unlikely to be examined in future trials. Our algorithm to identify the clinical outcome of interest was developed and validated in a population used herein and has a good PPV [43]. Our implementation of an incident user design, active comparator reference exposure, data adaptive approach to identify then adjust for confounders and their proxies, and secondary analyses served to mitigate confounding. Finally, we estimated marginal treatment effects, the same type of measure that arises from a clinical trial.
Our study also has limitations. First, despite rigor in our design and analysis, residual differences between pioglitazone and rosiglitazone users may remain. Second, our lack of access to biosamples precluded an examination of genetic determinants of SCA/VA risk. Third, our adjustment for family history of diseases relied on diagnostic coding and therefore was likely underascertained. Fourth, we lacked data on direct adherence to thiazolidinedione therapy. To address this, we conducted secondary analyses in which we modified the allowable grace period between contiguous prescriptions. Fifth, we did not assess competing events that may have precluded our observation of the outcome [76]. If competing risks were present, our reliance on the Kaplan–Meier estimate of the survival function to estimate the incidence function would generally result in an upward bias in the estimation of the incidence function [77]. Relatedly, we did not model cause-specific hazard functions. Finally, we may have underascertained outcomes, likely biasing towards the null. Because SCA/VA was defined using emergency department and inpatient diagnosis codes, we likely missed fatal events not resulting in hospital presentation. However, prior work suggests that 69–80% of persons experiencing an out-of-hospital cardiac arrest [78, 79] and up to 88% of persons experiencing a witnessed ventricular tachycardia survive to hospital admission [80], although recent registry data from CARES suggests poorer survival-to-admission rates (18–49%, depending on presenting characteristics) [81]. We considered using death certificates to identify supplemental events, but decided against it given the approach’s poor PPV for identifying SCA/VA [44, 82, 83].
Conclusions
Thiazolidinediones are a low-cost, effective treatment for type 2 DM, a highly prevalent condition in persons with limited economic means. Although substantial attention has been paid to thiazolidinediones and risk of AMI and heart failure, there is a major knowledge gap in their arrhythmogenic safety. In response, we generated real-world evidence that rosiglitazone and pioglitazone have similar risks of SCA/VA.
Availability of data and materials
The data that support the findings of this study are available from the United States (US) Centers for Medicare and Medicaid Services (CMS) and Optum Inc., but restrictions apply to the availability of these data, which were used under license for the current study and so are not publicly available. Data may be available from the authors upon reasonable request and with explicit permission from CMS and Optum Inc.
Abbreviations
- AMI:
-
Acute myocardial infarction
- CARES:
-
Cardiac arrest registry to enhance survival
- CMS:
-
Centers for Medicare and Medicaid Services
- DM:
-
Diabetes mellitus
- hdPS:
-
High-dimensional propensity score
- hERG:
-
Human ether-a-go-go-related gene
- HR:
-
Hazard ratio
- ICD-9-CM:
-
International classification of diseases, 9th revision, clinical modification
- PPV:
-
Positive predictive value
- P-Y:
-
Person-years
- RECORD:
-
Rosiglitazone evaluated for cardiovascular outcomes in oral agent combination therapy for type 2 diabetes
- SAVOR–TIMI 53:
-
Saxagliptin assessment of vascular outcomes recorded in patients with diabetes mellitus–thrombolysis in myocardial infarction 53
- SCA:
-
Sudden cardiac arrest
- SCD:
-
Sudden cardiac death
- TOSCA.IT:
-
Thiazolidinediones or sulfonylureas and cardiovascular accidents intervention trial
- US:
-
Unites States
- VA:
-
Ventricular arrhythmia
References
Beckles GL, Chou CF. Disparities in the prevalence of diagnosed diabetes—United States, 1999–2002 and 2011–2014. MMWR Morb Mortal Wkly Rep. 2016;65(45):1265–9.
United States Census Bureau: PINC-01. Selected characteristics of people 15 years and over, by total money income, work experience, race, Hispanic origin, and sex. 2017. https://www.census.gov/data/tables/time-series/demo/income-poverty/cps-pinc/pinc-01.2017.html. Accessed 6 Feb 2020.
Statista GmbH: State of health: percentage of adults in the US with diabetes as of 2016, by income. 2017. https://www.statista.com/statistics/790678/diabetes-prevalence-us-by-income/. Accessed 6 Feb 2020.
International Diabetes Federation. IDF diabetes atlas. 8th ed. Brussels: International Diabetes Federation; 2017.
World Health Organization. Global report on diabetes. Geneva: World Health Organization; 2016.
World Health Organization. Guidelines on second- and third-line medicines and type of insulin for the control of blood glucose levels in non-pregnant adults with diabetes mellitus. Geneva: World Health Organization; 2018.
American Diabetes Association. 9. Pharmacologic approaches to glycemic treatment: standards of medical care in diabetes-2019. Diabetes Care. 2019;42(Suppl 1):S90–102.
Friedland SN, Leong A, Filion KB, Genest J, Lega IC, Mottillo S, Poirier P, Reoch J, Eisenberg MJ. The cardiovascular effects of peroxisome proliferator-activated receptor agonists. Am J Med. 2012;125(2):126–33.
Pladevall M, Riera-Guardia N, Margulis AV, Varas-Lorenzo C, Calingaert B, Perez-Gutthann S. Cardiovascular risk associated with the use of glitazones, metformin and sufonylureas: meta-analysis of published observational studies. BMC Cardiovasc Disord. 2016;16:14.
Chiquette E, Ramirez G, Defronzo R. A meta-analysis comparing the effect of thiazolidinediones on cardiovascular risk factors. Arch Intern Med. 2004;164(19):2097–104.
Ida S, Kaneko R, Murata K. Effects of oral antidiabetic drugs on left ventricular mass in patients with type 2 diabetes mellitus: a network meta-analysis. Cardiovasc Diabetol. 2018;17(1):129.
Lago RM, Singh PP, Nesto RW. Congestive heart failure and cardiovascular death in patients with prediabetes and type 2 diabetes given thiazolidinediones: a meta-analysis of randomised clinical trials. Lancet. 2007;370(9593):1129–36.
Strongman H, Korhonen P, Williams R, Bahmanyar S, Hoti F, Christopher S, Majak M, Kool-Houweling L, Linder M, Dolin P, Heintjes EM. Pioglitazone and risk of mortality in patients with type 2 diabetes: results from a European multidatabase cohort study. BMJ Open Diabetes Res Care. 2017;5(1):e000364.
Gintant GA, Su Z, Martin RL, Cox BF. Utility of hERG assays as surrogate markers of delayed cardiac repolarization and QT safety. Toxicol Pathol. 2006;34(1):81–90.
Lee SH, Sung MJ, Hahn SJ, Kim J, Min G, Jo SH, Choe H, Choi BH. Blockade of human HERG K(+) channels by rosiglitazone, an antidiabetic drug. Arch Pharm Res. 2012;35(9):1655–64.
Arnold SV, Inzucchi SE, Echouffo-Tcheugui JB, Tang F, Lam CSP, Sperling LS, Kosiborod M. Understanding contemporary use of thiazolidinediones. Circ Heart Fail. 2019;12(6):e005855.
DeFronzo RA, Chilton R, Norton L, Clarke G, Ryder RE, Abdul-Ghani M. Revitalization of pioglitazone: the optimum agent to be combined with a sodium-glucose co-transporter-2 inhibitor. Diabetes Obes Metab. 2016;18(5):454–62.
Prost S, Relouzat F, Spentchian M, Ouzegdouh Y, Saliba J, Massonnet G, Beressi JP, Verhoeyen E, Raggueneau V, Maneglier B, Castaigne S, Chomienne C, Chretien S, Rousselot P, Leboulch P. Erosion of the chronic myeloid leukaemia stem cell pool by PPARgamma agonists. Nature. 2015;525(7569):380–3.
Davidson MA, Mattison DR, Azoulay L, Krewski D. Thiazolidinedione drugs in the treatment of type 2 diabetes mellitus: past, present and future. Crit Rev Toxicol. 2018;48(1):52–108.
Prins KW, Thenappan T, Weir EK, Kalra R, Pritzker M, Archer SL. Repurposing medications for treatment of pulmonary arterial hypertension: what’s old is new again. J Am Heart Assoc. 2019;8(1):e011343.
US National Library of Medicine. Comparison of the effects of thiazolidinediones (TZD), sodium-glucose cotransporter 2 inhibitors (SGLT2i) alone and TZD/SGLT2i combination therapy on non-alcoholic fatty liver disease in type 2 diabetic patients with fatty liver. ClinicalTrials.gov. 2019. https://clinicaltrials.gov/ct2/show/NCT03646292. Accessed 6 Feb 2020.
Agrawal S, Chanley MA, Westbrook D, Nie X, Kitao T, Guess AJ, Benndorf R, Hidalgo G, Smoyer WE. Pioglitazone enhances the beneficial effects of glucocorticoids in experimental nephrotic syndrome. Sci Rep. 2016;6:24392.
Spence JD, Viscoli CM, Inzucchi SE, Dearborn-Tomazos J, Ford GA, Gorman M, Furie KL, Lovejoy AM, Young LH, Kernan WN. IRIS Investigators: pioglitazone therapy in patients with stroke and prediabetes: a post hoc analysis of the iris randomized clinical trial. JAMA Neurol. 2019;76(5):526–35.
Vaccaro O, Masulli M, Nicolucci A, Bonora E, Del Prato S, Maggioni AP, Rivellese AA, Squatrito S, Giorda CB, Sesti G, Mocarelli P, Lucisano G, Sacco M, Signorini S, Cappellini F, Perriello G, Babini AC, Lapolla A, Gregori G, Giordano C, Corsi L, Buzzetti R, Clemente G, Di Cianni G, Iannarelli R, Cordera R, La Macchia O, Zamboni C, Scaranna C, Boemi M, Iovine C, Lauro D, Leotta S, Dall’Aglio E, Cannarsa E, Tonutti L, Pugliese G, Bossi AC, Anichini R, Dotta F, Di Benedetto A, Citro G, Antenucci D, Ricci L, Giorgino F, Santini C, Gnasso A, De Cosmo S, Zavaroni D, Vedovato M, Consoli A, Calabrese M, di Bartolo P, Fornengo P, Riccardi G, Thiazolidinediones Or Sulfonylureas Cardiovascular Accidents Intervention Trial (TOSCA.IT) study group, Italian Diabetes Society. Effects on the incidence of cardiovascular events of the addition of pioglitazone versus sulfonylureas in patients with type 2 diabetes inadequately controlled with metformin (TOSCA.IT): a randomised, multicentre trial. Lancet Diabetes Endocrinol. 2017;5(11):887–97.
Liberthson RR. Sudden death from cardiac causes in children and young adults. N Engl J Med. 1996;334(16):1039–44.
Hennessy S, Leonard CE, Palumbo CM, Newcomb C, Bilker WB. Quality of Medicaid and Medicare data obtained through Centers for Medicare and Medicaid Services (CMS). Med Care. 2007;45(12):1216–20.
Leonard CE, Brensinger CM, Nam YH, Bilker WB, Barosso GM, Mangaali MJ, Hennessy S. The quality of Medicaid and Medicare data obtained from CMS and its contractors: implications for pharmacoepidemiology. BMC Health Serv Res. 2017;17(1):304.
Wang SV, Schneeweiss S, Berger ML, Brown J, de Vries F, Douglas I, Gagne JJ, Gini R, Klungel O, Mullins CD, Nguyen MD, Rassen JA, Smeeth L, Sturkenboom M, Joint ISPE-ISPOR Special Task Force on Real World Evidence in Health Care Decision Making. Reporting to improve reproducibility and facilitate validity assessment for healthcare database studies v1.0. Pharmacoepidemiol Drug Saf. 2017;26(9):1018–32.
Wang SV, Schneeweiss S, Berger ML, Brown J, de Vries F, Douglas I, Gagne JJ, Gini R, Klungel O, Mullins CD, Nguyen MD, Rassen JA, Smeeth L, Sturkenboom M, Joint ISPE-ISPOR Special Task Force on Real World Evidence in Health Care Decision Making. Reporting to improve reproducibility and facilitate validity assessment for healthcare database studies v1.0. Value Health. 2017;20(8):1009–22.
Wang SV, Verpillat P, Rassen JA, Patrick A, Garry EM, Bartels DB. Transparency and reproducibility of observational cohort studies using large healthcare databases. Clin Pharmacol Ther. 2016;99(3):325–32.
Berger ML, Sox H, Willke RJ, Brixner DL, Eichler HG, Goettsch W, Madigan D, Makady A, Schneeweiss S, Tarricone R, Wang SV, Watkins J, Mullins CD. Good practices for real-world data studies of treatment and/or comparative effectiveness: recommendations from the joint ISPOR-ISPE special task force on real-world evidence in health care decision making. Value Health. 2017;20(8):1003–8.
Henney JE. Withdrawal of troglitazone and cisapride. JAMA. 2000;283(17):2228.
AZCERT: Risk categories for drugs that prolong QT & induce torsades de pointes (TdP). CredibleMeds. 2019. https://crediblemeds.org/new-drug-list/. Accessed 6 Feb 2020.
Suissa S. Immeasurable time bias in observational studies of drug effects on mortality. Am J Epidemiol. 2008;168(3):329–35.
Lund JL, Richardson DB, Sturmer T. The active comparator, new user study design in pharmacoepidemiology: historical foundations and contemporary application. Curr Epidemiol Rep. 2015;2(4):221–8.
Raschi E, Poluzzi E, Koci A, Boriani G, De Ponti F. QT interval shortening in spontaneous reports submitted to the FDA: the need for consensus. Br J Clin Pharmacol. 2011;72(5):839–41.
DrugBank: Pioglitazone. https://www.drugbank.ca/drugs/DB01132. Accessed 6 Feb 2020.
Austin PC. The use of propensity score methods with survival or time-to-event outcomes: reporting measures of effect similar to those used in randomized experiments. Stat Med. 2014;33(7):1242–58.
Toh S, Garcia Rodriguez LA, Hernan MA. Confounding adjustment via a semi-automated high-dimensional propensity score algorithm: an application to electronic medical records. Pharmacoepidemiol Drug Saf. 2011;20(8):849–57.
Schneeweiss S, Rassen JA, Glynn RJ, Avorn J, Mogun H, Brookhart MA. High-dimensional propensity score adjustment in studies of treatment effects using health care claims data. Epidemiology. 2009;20(4):512–22.
Brigham and Women’s Hospital: Pharmacoepidemiology toolbox. http://www.drugepi.org/dope-downloads/. Accessed 6 Feb 2020.
McMurray J. Prophylactic class III antiarrhythmic drug therapy after myocardial infarction: ALIVE or dead? Cardiology Scientific Update 2002. Boston: SNELL Medical Communication, Inc. Report no. 402-010.
Hennessy S, Leonard CE, Freeman CP, Deo R, Newcomb C, Kimmel SE, Strom BL, Bilker WB. Validation of diagnostic codes for outpatient-originating sudden cardiac death and ventricular arrhythmia in Medicaid and Medicare claims data. Pharmacoepidemiol Drug Saf. 2010;19(6):555–62.
Chugh SS, Jui J, Gunson K, Stecker EC, John BT, Thompson B, Ilias N, Vickers C, Dogra V, Daya M, Kron J, Zheng ZJ, Mensah G, McAnulty J. Current burden of sudden cardiac death: Multiple source surveillance versus retrospective death certificate-based review in a large U.S. community. J Am Coll Cardiol. 2004;44(6):1268–75.
Moghissi ES, Korytkowski MT, DiNardo M, Einhorn D, Hellman R, Hirsch IB, Inzucchi SE, Ismail-Beigi F, Kirkman MS, Umpierrez GE. American Association of Clinical Endocrinologists, American Diabetes Association: American Association of Clinical Endocrinologists and American Diabetes Association consensus statement on inpatient glycemic control. Endocr Pract. 2009;15(4):353–69.
ISPOR. ISPOR international digest of databases. 2019. Available at: https://tools.ispor.org/Intl_Databases/index.asp. Accessed 6 Feb 2020.
Rassen JA, Glynn RJ, Brookhart MA, Schneeweiss S. Covariate selection in high-dimensional propensity score analyses of treatment effects in small samples. Am J Epidemiol. 2011;173(12):1404–13.
Guertin JR, Rahme E, LeLorier J. Performance of the high-dimensional propensity score in adjusting for unmeasured confounders. Eur J Clin Pharmacol. 2016;72(12):1497–505.
Bross ID. Spurious effects from an extraneous variable. J Chronic Dis. 1966;19(6):637–47.
Wyss R, Fireman B, Rassen JA, Schneeweiss S. Erratum: high-dimensional propensity score adjustment in studies of treatment effects using health care claims data. Epidemiology. 2018;29(6):e63–4.
Schneeweiss S, Seeger JD, Maclure M, Wang PS, Avorn J, Glynn RJ. Performance of comorbidity scores to control for confounding in epidemiologic studies using claims data. Am J Epidemiol. 2001;154(9):854–64.
VanderWeele TJ. Principles of confounder selection. Eur J Epidemiol. 2019;34(3):211–9.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28(25):3083–107.
Austin PC. A comparison of 12 algorithms for matching on the propensity score. Stat Med. 2014;33(6):1057–69.
Lin DY, Wei LJ. The robust inference for the Cox proportional hazards model. JASA. 1989;84(408):1074–8.
Rea TD, Pearce RM, Raghunathan TE, Lemaitre RN, Sotoodehnia N, Jouven X, Siscovick DS. Incidence of out-of-hospital cardiac arrest. Am J Cardiol. 2004;93(12):1455–60.
Siscovick DS, Sotoodehnia N, Rea TD, Raghunathan TE, Jouven X, Lemaitre RN. Type 2 diabetes mellitus and the risk of sudden cardiac arrest in the community. Rev Endocr Metab Disord. 2010;11(1):53–9.
Leonard CE, Brensinger CM, Aquilante CL, Bilker WB, Boudreau DM, Deo R, Flory JH, Gagne JJ, Mangaali MJ, Hennessy S. Comparative safety of sulfonylureas and the risk of sudden cardiac arrest and ventricular arrhythmia. Diabetes Care. 2018;41(4):713–22.
Leonard CE, Han X, Brensinger CM, Bilker WB, Cardillo S, Flory JH, Hennessy S. Comparative risk of serious hypoglycemia with oral antidiabetic monotherapy: a retrospective cohort study. Pharmacoepidemiol Drug Saf. 2018;27(1):9–18.
Leonard CE, Hennessy S, Han X, Siscovick DS, Flory JH, Deo R. Pro- and anti-arrhythmic actions of sulfonylureas: mechanistic and clinical evidence. Trends Endocrinol Metab. 2017;28(8):561–86.
Wang SH, Chen WJ, Hsu LY, Chien KL, Wu CS. Use of spontaneous reporting systems to detect host-medication interactions: sex differences in oral anti-diabetic drug-associated myocardial infarction. J Am Heart Assoc. 2018;7(22):e008959.
Dennis JM, Henley WE, Weedon MN, Lonergan M, Rodgers LR, Jones AG, Hamilton WT, Sattar N, Janmohamed S, Holman RR, Pearson ER, Shields BM, Hattersley AT. MASTERMIND Consortium: sex and BMI alter the benefits and risks of sulfonylureas and thiazolidinediones in type 2 diabetes: a framework for evaluating stratification using routine clinical and individual trial data. Diabetes Care. 2018;41(9):1844–53.
Authors/Task Force Members, Ryden L, Grant PJ, Anker SD, Berne C, Cosentino F, Danchin N, Deaton C, Escaned J, Hammes HP, Huikuri H, Marre M, Marx N, Mellbin L, Ostergren J, Patrono C, Seferovic P, Uva MS, Taskinen MR, Tendera M, Tuomilehto J, Valensi P, Zamorano JL, ESC Committee for Practice Guidelines (CPG), Zamorano JL, Achenbach S, Baumgartner H, Bax JJ, Bueno H, Dean V, Deaton C, Erol C, Fagard R, Ferrari R, Hasdai D, Hoes AW, Kirchhof P, Knuuti J, Kolh P, Lancellotti P, Linhart A, Nihoyannopoulos P, Piepoli MF, Ponikowski P, Sirnes PA, Tamargo JL, Tendera M, Torbicki A, Wijns W, Windecker S, Document Reviewers, De Backer G, Sirnes PA, Ezquerra EA, Avogaro A, Badimon L, Baranova E, Baumgartner H, Betteridge J, Ceriello A, Fagard R, Funck-Brentano C, Gulba DC, Hasdai D, Hoes AW, Kjekshus JK, Knuuti J, Kolh P, Lev E, Mueller C, Neyses L, Nilsson PM, Perk J, Ponikowski P, Reiner Z, Sattar N, Schachinger V, Scheen A, Schirmer H, Stromberg A, Sudzhaeva S, Tamargo JL, Viigimaa M, Vlachopoulos C, Xuereb RG. ESC Guidelines on diabetes, pre-diabetes, and cardiovascular diseases developed in collaboration with the EASD: the Task Force on diabetes, pre-diabetes, and cardiovascular diseases of the European Society of Cardiology (ESC) and developed in collaboration with the European Association for the Study of Diabetes (EASD). Eur Heart J 2013, 34(39):3035–87.
Cavallari L, Patel R, Bhatt D, Steg P, Leiter L, McGuire D, Mosenzon O, Kanevsky E, Im K, Raz I, Braunwald E, Scirica B. Clinical factors associated with sudden cardiac death in type 2 diabetes: insights from the SAVOR-TIMI 53 trial. JACC. 2016;67(13 Suppl):2083. https://doi.org/10.1016/s0735-1097(16)32084-8.
Kaul S, Bolger AF, Herrington D, Giugliano RP, Eckel RH, American Heart Association, American College Of Cardiology Foundation: Thiazolidinedione drugs and cardiovascular risks: a science advisory from the American Heart Association and American College of Cardiology Foundation. J Am Coll Cardiol. 2010;55(17):1885–94.
Zinn A, Felson S, Fisher E, Schwartzbard A. Reassessing the cardiovascular risks and benefits of thiazolidinediones. Clin Cardiol. 2008;31(9):397–403.
Margolis DJ, Leonard CE, Razzaghi H, Hoffstad OJ, Freeman CP, de Nava KL, Molina T, Tan Y, Bartman BA. Utilization of antidiabetic drugs among Medicare beneficiaries with diabetes, 2006–2009: data points #9. In: Data points publication series. Rockville: AHRQ; 2011.
Mahaffey KW, Hafley G, Dickerson S, Burns S, Tourt-Uhlig S, White J, Newby LK, Komajda M, McMurray J, Bigelow R, Home PD, Lopes RD. Results of a reevaluation of cardiovascular outcomes in the RECORD trial. Am Heart J. 2013;166(2):240–249.e1.
Tuccori M, Filion KB, Yin H, Yu OH, Platt RW, Azoulay L. Pioglitazone use and risk of bladder cancer: population based cohort study. BMJ. 2016;352:i1541.
Ziyadeh N, McAfee AT, Koro C, Landon J, Arnold Chan K. The thiazolidinediones rosiglitazone and pioglitazone and the risk of coronary heart disease: a retrospective cohort study using a US health insurance database. Clin Ther. 2009;31(11):2665–77.
Goldberg RB, Kendall DM, Deeg MA, Buse JB, Zagar AJ, Pinaire JA, Tan MH, Khan MA, Perez AT, Jacober SJ, GLAI Study Investigators. A comparison of lipid and glycemic effects of pioglitazone and rosiglitazone in patients with type 2 diabetes and dyslipidemia. Diabetes Care. 2005;28(7):1547–54.
Arnetz L, Dorkhan M, Alvarsson M, Brismar K, Ekberg NR. Gender differences in non-glycemic responses to improved insulin sensitivity by pioglitazone treatment in patients with type 2 diabetes. Acta Diabetol. 2014;51(2):185–92.
Miller ME, Bonds DE, Gerstein HC, Seaquist ER, Bergenstal RM, Calles-Escandon J, Childress RD, Craven TE, Cuddihy RM, Dailey G, Feinglos MN, Ismail-Beigi F, Largay JF, O’Connor PJ, Paul T, Savage PJ, Schubart UK, Sood A, Genuth S, ACCORD Investigators. The effects of baseline characteristics, glycaemia treatment approach, and glycated haemoglobin concentration on the risk of severe hypoglycaemia: post hoc epidemiological analysis of the ACCORD study. BMJ. 2010;340:b5444.
Ben V, Klintscher U, Foryst-Ludwig A. Sex-specific differences in type 2 diabetes mellitus and dyslipidemia therapy: PPAR agonists. In: Regitz-Zagrosek V, editor. Sex and gender differences in pharmacology. Berlin: Springer-Verlag; 2012. p. 387–410.
Sharma SK, Verma SH. A study of effects of pioglitazone and rosiglitazone on various parameters in patients of type-2 diabetes mellitus with special reference to lipid profile. J Assoc Physicians India. 2016;64(9):24–8.
Edwards JK, Hester LL, Gokhale M, Lesko CR. Methodologic issues when estimating risks in pharmacoepidemiology. Curr Epidemiol Rep. 2016;3(4):285–96.
Austin PC, Lee DS, Fine JP. Introduction to the analysis of survival data in the presence of competing risks. Circulation. 2016;133(6):601–9.
Bunch TJ, White RD, Bruce GK, Hammill SC, Gersh BJ, Shen WK, Carter MA, Packer DL. Prediction of short- and long-term outcomes by electrocardiography in survivors of out-of-hospital cardiac arrest. Resuscitation. 2004;63(2):137–43.
Manfredini R, Portaluppi F, Grandi E, Fersini C, Gallerani M. Out-of-hospital sudden death referring to an emergency department. J Clin Epidemiol. 1996;49(8):865–8.
Myerburg RJ, Kessler KM, Zaman L, Conde CA, Castellanos A. Survivors of prehospital cardiac arrest. JAMA. 1982;247(10):1485–90.
Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, Delling FN, Djousse L, Elkind MSV, Ferguson JF, Fornage M, Jordan LC, Khan SS, Kissela BM, Knutson KL, Kwan TW, Lackland DT, Lewis TT, Lichtman JH, Longenecker CT, Loop MS, Lutsey PL, Martin SS, Matsushita K, Moran AE, Mussolino ME, O’Flaherty M, Pandey A, Perak AM, Rosamond WD, Roth GA, Sampson UKA, Satou GM, Schroeder EB, Shah SH, Spartano NL, Stokes A, Tirschwell DL, Tsao CW, Turakhia MP, VanWagner LB, Wilkins JT, Wong SS, Virani SS, American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee. Heart disease and stroke statistics-2019 update: A report from the American Heart Association. Circulation. 2019;139(10):e56–528.
Fox CS, Evans JC, Larson MG, Lloyd-Jones DM, O’Donnell CJ, Sorlie PD, Manolio TA, Kannel WB, Levy D. A comparison of death certificate out-of-hospital coronary heart disease death with physician-adjudicated sudden cardiac death. Am J Cardiol. 2005;95(7):856–9.
Iribarren C, Crow RS, Hannan PJ, Jacobs DR Jr, Luepker RV. Validation of death certificate diagnosis of out-of-hospital sudden cardiac death. Am J Cardiol. 1998;82(1):50–3.
Acknowledgements
The authors thank Ms. Qing Liu and Ms. Min Du from the Perelman School of Medicine at the University of Pennsylvania for their computer programming support.
Funding
This work was supported by grants from the American Diabetes Association (1-18-ICTS-097, PI: Dr. Charles E. Leonard), the US National Institute on Aging (R01AG060975, PI: Dr. Charles E. Leonard; R01AG025152, PI: Dr. Sean Hennessy; and R01AG064589, PI: Dr. Sean Hennessy), and the US National Institute of General Medical Sciences (T32GM075766, PI: Dr. Sean Hennessy). Neither the American Diabetes Association nor the US National Institutes of Health had a role in the study’s conduct or interpretation.
Author information
Authors and Affiliations
Contributions
CEL, WBB, and SH conceived and designed the analysis. CMB, WBB, JJG contributed analysis tools. CMB and WBB performed the analyses. CEL wrote the initial draft of the manuscript. CMB, GKD, RD, WBB, SES, ND, JHF, ZTB, CLA, SEK, and SH revised the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The University of Pennsylvania institutional review board approved this research (protocol #823865).
Consent for publication
Not applicable.
Competing interests
CEL serves on the Executive Committee of and SH directs the University of Pennsylvania’s Center for Pharmacoepidemiology Research and Training. The Center receives unrestricted support for education from Pfizer. JHF has consulted for Boehringer Ingelheim, Eli Lilly and Company, and Genentech. JJG has received salary support from grants from Eli Lilly and Company and Novartis to the Brigham and Women’s Hospital, and was a consultant to Aetion Inc. and Optum Inc., all for unrelated work. SEK has consulted for pharmaceutical companies, unrelated to this work. SH has consulted for GlaxoSmithKline on matters unrelated to this work. All other authors report no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Additional file 1.
Additional tables and figures.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Leonard, C.E., Brensinger, C.M., Dawwas, G.K. et al. The risk of sudden cardiac arrest and ventricular arrhythmia with rosiglitazone versus pioglitazone: real-world evidence on thiazolidinedione safety. Cardiovasc Diabetol 19, 25 (2020). https://doi.org/10.1186/s12933-020-00999-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12933-020-00999-5