Abstract
Background
Elderly patients with coronary artery disease (CAD) frequently complicated with more cardiovascular risk factors, but received fewer evidence-based medications (EBMs). This study explored the association of EBMs compliance in different age groups and the risk of long-term death.
Methods
A retrospective analysis was conducted from a single registered database. 2830 consecutive patients with CAD were enrolled and grouped into 3 categories by age. The primary end point was all-cause mortality and secondary endpoint is cardiovascular mortality.
Results
The mean follow-up time was 30.25 ± 11.89 months and death occurred in 270 cases,including 150 cases of cardiac death. Cumulative survival curves indicated that the incidence rates of all-cause death and cardiovascular death increased with age (older than 75 years old vs. 60 to 75 years old vs. younger than 60 years old, mortality: 18.7% vs. 9.6% vs. 4.1%, p < 0.001; cardiovascular mortality: 10.3% vs. 5.1% vs. 2.7%, p < 0.001). The percentage of elderly patients using no EBMs was significantly higher than the percentages in the other age group (7.7% vs. 4.6% vs. 2.2%,p < 0.05). Cox regression analysis revealed the benefit of combination EBMs (all-cause mortality: hazard ratio [HR] 0.15, 95% CI 0.08–0.27; cardiac mortality: HR 0.08, 95% CI 0.04–0.19) for older CAD patients. Similar trends were found about different kinds of EBMs in elderly patients.
Conclusions
Elderly patients with CAD had higher risk of death but a lower degree of compliance with EBMs usage. Elderly CAD patients could receive more clinical benefits by using EBMs.
Similar content being viewed by others
Background
After 30 years of rapid economic growth, China is facing the dual pressures of chronic non-communicable diseases and an ageing population [1, 2]. Elderly patients frequently have complications from various cardiovascular disease risk factors, such as hypertension, hyperlipidaemia, and diabetes, which are independently associated with cardiovascular events and deaths in patients with coronary artery disease (CAD) [3,4,5]. Studies have shown that CAD is the most common disease in people over 65 years of age and that 83% of patients who die of ischaemic heart disease are older than 65 years [3]. Current treatment for CAD have entered the era of evidence-based medications (EBMs), and the clinical diagnosis and treatment are implemented following the standard of care listed in the guidelines [6,7,8,9]. However, the current guidelines were established based on studies that did not take age factors into full account; in addition, many studies completely excluded elderly patients due to safety considerations [10,11,12]. Furthermore, when treating elderly patients, clinicians have more concerns for the therapeutic window and the possibility of side effects due to elderly patients’ unique physiological characteristics [13]. Therefore, current guidelines might have significant limitations regarding clinical compliance among elderly CAD patients. These limitations have not been adequately studied among CAD patients in China.
By analysing a single-centre cohort of 2830 CAD patients, this study explored the association of EBM compliance in CAD patients in different age groups and the risk of long-term death.
Methods
Study population
We investigated patients undergoing angiography from July 2008 to December 2010 included the West China Hospital CAD database. Patients met the inclusion criteria when they were restricted to participants with angiographic evidence of ≥50% stenosis in ≥1 coronary vessels. The exclusion criteria included pregnancy, malignancies, end stage renal disease (ESRD) with haemodialysis or renal transplant and severe liver or haematological diseases. Severe liver diseases were defined as liver insufficiency that lead to haemostatic disturbances, aminotransferases and bilirubin concentrations 3 times greater than the normal upper limits and other factors that may preclude angiography and subsequent EBM therapy [14]. Haematological diseases were defined as severe anaemia, myeloproliferative disorders, coagulopathies and haematological malignancies that may preclude angiography and subsequent EBM therapy. Patients with moderate and severe iron deficiency anaemia were excluded from our study. These inclusion and exclusion criteria were met by 3178 continuously enrolled CAD patients. A total of 302 patients were lost to follow-up and another 46 had incomplete follow-up data. There were 2830 patients included in the data analysis. The study protocol was approved by the local institutional review boards in accordance with the Declaration of Helsinki. Informed consent was obtained from all individual participants included in the study.
Baseline characteristics
Demographic data, medical history, cardiovascular risk factors, vital signs at admission, medication at discharge, and final diagnosis were obtained from the patients’ electronic medical records and reviewed by a trained study coordinator. Blood sample were collected before angiography, and plasma biomarkers including markers of liver and kidney function (including the admission serum creatinine levels), blood glucose, serum lipids, and others, were analysed in the department of laboratory medicine, West China hospital, accredited by the College of American Pathologists. Hypertensive individuals were defined as those with systolic blood pressure (SBP) greater than 140 mmHg and/or diastolic blood pressure (DBP) greater than 90 mmHg and/or those receiving antihypertensive medications for 2 weeks. Diabetes was diagnosed when patients had previously undergone dietary treatment and/or had received additional oral antidiabetic or insulin medication or had a current fasting blood glucose level of ≥7.0 mmol/L or random blood glucose level ≥ 11.1 mmol/L. Dyslipidemia was defined as fasting serum total cholesterol (TC) level ≥ 5.18 mmol/L, and/or fasting serum low-density lipoprotein cholesterol (LDL-C) level ≥ 3.37 mmol/L, and/or fasting serum high-density lipoprotein-cholesterol (HDL-C) level of 1.04 mmol/L, and/or fasting serum triglycerides (TG) level ≥ 1.70 mmol/L, and/or those receiving treatment with drugs or therapeutic life-style change for dyslipidaemia. Acute myocardial infarction (AMI) was diagnosed by cardiologists, based on the triad of chest pain, electrocardiogram changes, and elevated cardiac troponin I levels (≥0.03 μg/L) or elevated cardiac troponin T levels (≥42 ng/L). Patients received care according to the usual practice; treatment was not affected by participation in this study.
Follow-up and end points
The follow-up period ended in January 2013. Follow-up information was collected by contacting with patients, their family or physicians, follow-up information was collected. All data were corroborated with the hospital records. The primary end points in this study was all-cause mortality and the secondary endpoints is cardiovascular (CV) death. Death was considered cardiac-related when it was caused by AMI, significant arrhythmias, or refractory heart failure. Sudden unexpected death occurring without another explanation was also included.
Statistical analyses
We conducted the post-hoc analysis on a retrospective basis. Baseline demographics and clinical characteristics were compared among patients categorized by age in 3 group corresponding to strata used to define elderly: Group 1: younger than 60 years old; Group 2: ranging from 60 to 75 years old and Group 3: older than 75 years old. The clinical characteristics of each of the three groups were presented as frequencies and percentages for categorical variables and as means ± standard deviation (SD) for continuous variables, respectively. Means were compared with analysis of variance (ANOVA) and nominal variables were compared with the chi-square test. The Kaplan-Meier and the log-rank test were used for survival analysis in relation to all-cause mortality and cardiovascular in CAD patients. The effects of discharged EBMs effects on all-cause mortality and mortality were considered in a Cox proportional hazards regression model in both unadjusted and adjusted fashion, and hazard ratios (HRs) were estimated with 95% confidence intervals (CIs). EBMs included aspirin, beta-receptor blockers, statins and angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin-receptor blockers (ARBs) [8, 9]. Adjustments were made for the possible confounding effects of sex, history of hypertension, history of diabetes mellitus, history of heart failure, history of dyslipidaemia, smoking status, eGFR and hepatic enzymes. Because of the significant imbalances in baseline covariates between patients with and without EBMs, we used a 1:1 propensity score-matched pair method combined with covariate adjustment including sex, history of hypertension, history of diabetes mellitus, history of heart failure, history of dyslipidaemia, smoking status, eGFR and hepatic enzymes to analyse patients with and without the prescription of different kind of EBMs (for detail See Additional file 1). Then we constructed a Cox proportional hazards regression model in unadjusted fashion to compare outcomes among matched pairs of patients with and without the prescription of different kind. Increasingly adjusted models for composite effect of discharged medication on mortality were built for all-cause mortality and cardiovascular mortality to assess the three EBMs: beta-receptor blockers, statins and ACEIs or ARBs. Therefore, models were built as described below to classify the number of prescription regardless of the type of drugs: model 0: no medications; model 1: prescribed 1 type of EBM; model 2, prescribed 2 types of EBMs; and model 3, prescribed all 3 types of EBMs. Two-sided p values of less than 0.05 indicated statistical significance. All analyses were performed with SPSS software (version 19.0).
Results
A total of 2830 patients with CAD were included in the study. The the average age and its SD were 64.62 ± 10.54 years, and 20.3% of the patients were male. A total of 850 (30.0%) patients are younger than 60 years old, 1490 (52.6%) were in the range of 60 to 75 years old and 491(17.3%) were over 75 years old. The distribution of baseline data is shown in Table 1. The clinical features of the patients showed certain differences between groups. Older patients have a lower proportion of dyslipidaemia, and higher proportion of hypertension, diabetes mellitus and heart failure (p < 0.001). The percentage of patients diagnosed with non-ST segment elevation myocardial infarction (NSTEMI) had a higher trending proportion (Fig. 1).
Discharge prescription of EBMs for CAD patients stratified by age (P < 0.05 for trend in EBMs, including aspirin, clopidogrel, dual antiplatelet, statins, beta-blockers, and ACEIs or ARBs, according to age). Abbreviations: EBMs, evidence-based medicines; CAD, coronary artery disease; ACEI, angiotensin-converting enzyme inhibitor; ARBs, angiotensin receptor blockers
The average follow up was 30.25 ± 11.89 months. A total of 270 cases of all-cause death occurred (mortality, 9.5%, 95% CI: 8.5%–10.7%), including 150 cases of cardiovascular death (cardiovascular mortality, 5.3%, 95% CI, 4.5%–6.2%). The survival curve of patients older than 75 years old had a significantly higher risk of all-cause death (panel A) and cardiovascular death (panel B) than the group ranging from 60 to 75 years old and the group younger than 60 years old (mortality, Group 3 vs. Group 1: 18.7% vs. 4.1%, p < 0.001; Group 2 vs. Group 1: 9.6% vs. 4.1%, p < 0.001; cardiovascular mortality, Group 3 vs. Group 1: 10.3% vs. 2.7%, p < 0.001; Group 2 vs. Group 1: 5.1% vs. 2.7%, p < 0.001) (Fig. 2).
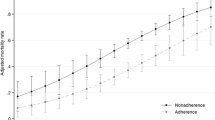
Approximately 92.2% of CAD patients were discharged with aspirin, 86.4% with aspirin and clopidogrel, 66.22% with beta-blockers, 56.6% with ACE inhibitors, 89.1% with statins, and 36% with the combination of aspirin, clopidogrel, beta-blockers, ACE inhibitors, and statins. The medicine proportion of ere different in all groups. In the group 2 and 3, the proportion of EBMs prescribed at discharge is significantly lower than the younger but ACEIs or ARBs is opposite. (asprin, dual-antiplatelet, and beta-blockers: all p for tends < 0.001; and statins: p = 0.023) (Fig. 3). Meanwhile, we analysed the combined use of beta-blockers, statins, and ACEIs or ARBs among the EBMs (Fig. 4). The percentage of patients over 75 years old using no EBMs was significantly higher than the percentages in the other 2 groups (7.7% vs. 4.6% vs. 2.2%,p for trend < 0.05) (Fig. 4).
In multivariate Cox’s proportional hazards regression model analyses each kind of EBMs (beta-blockers, statins, and ACEIs or ARBs) alone was considered an important modifiable protective factor of both all-cause death and CV death in patients ranged from 60 to 75 years old or over 75 years old (Table 2). For ACEI or ARB use, Group 3 and 2 benefit more than Group 1 regarding to all-cause death and CV death (all-cause death: Group 1: HR = 0.89, 95% CI, 0.44–1.80; Group 2: HR =0.48, 95% CI, 0.34–0.68; Group 3: HR =0.54, 95% CI, 0.35–0.84; CV death: Group 1: HR = 0.54, 95% CI, 0.22–1.34; Group 2: HR =0.42, 95% CI, 0.26–0.68; Group 3: HR =0.45, 95% CI, 0.25–0.83). In the unadjusted Cox’s proportional hazards regression model analysis of the patients after propensity score matching, we obtained constant results with the adjusted analysis of patients before propensity score matching (Table 2). The combination of EBM use resulted in a greater reduction in the risk of all-cause death even in patients older than 75 years. Meanwhile, similar results were observed in the analysis of CV death (Table 3).
Discussion
This study found that elderly patients had complications with more cardiovascular disease risk factors and had higher all-cause death and cardiovascular events. However, the proportion of elderly patients receiving EBMs was lower than that of younger patients. Patients who had higher compliance with EBMs exhibited a lower risk of death.
Age is an important risk factor for poor prognosis in patients with CAD [15]. On one hand, with increases in age and organ ageing, the capacity to survive cardiovascular events declines; on the other hand, due to concerns regarding drug tolerance and side effects, elderly patients often receive insufficiently effective drugs, resulting in poor prognosis [16,17,18,19]. Previous studies have shown that complications or dysfunctions of liver and kidney limit the use of statins and ACEI/ ARB drugs [17, 18]. Concerns regarding the risk of bleeding and gastrointestinal discomfort limit the use of aspirin in elderly patients [20, 21]. Similar with previous foreign reports [3, 22, 23], our study suggests that EBM compliance among Chinese patients with CAD is notably inadequate.
The reasons for inadequate compliance with EBMs for elderly patients are not clearly elucidated. Based on previous studies, we speculate that the inadequate compliance might be caused by the following reasons. (1) Due to organ dysfunction, elderly patients had concerns about drug side effects. For example, due to high risk of cerebral haemorrhage and gastrointestinal bleeding, elderly patients had more concerns about the risk of bleeding associated with anti-platelet drugs, especially double antiplatelet therapy [21, 24]; due to liver and renal dysfunction, elderly patients had major concerns about statin-induced liver injury and ACEI/ARB-induced renal damage [25,26,27]; and due to conduction dysfunction and high incidence of chronic obstructive pulmonary disease (COPD), elderly patients had concerns that a beta-blocker would aggravate slow arrhythmia and wheezing [28, 29]. (2) Elderly patients had poor tolerance for drugs. Elderly patients had a narrow therapeutic window, with the minimum effective concentration being very close to the minimum toxic concentration [30]. (3) The physical conditions of elderly patients is frequently changing. CAD is a chronic disease, and the long-term compliance with EBMs requires complicated medication dose adjustment and maintenance [13]. (4) Elderly patients often suffered from multiple diseases and therefore bear high medication costs [31]. (5) Elderly patients had decreased memory and limited social support, negatively affecting long-term medication compliance [32]. The above factors not only led to low EBM compliance among the elderly patients but also discouraged physicians from prescribing EBMs to elderly CAD patients. However, the available evidence does not show that elderly CAD patients should reduce the use of EBMs [33,34,35]. Two meta-analyses showed that statin use in elderly patients over 65 years of age was able to reduce the risk of all-cause mortality by 22%, coronary-related deaths by 30%, myocardial infarction by 26% and revascularization by 30% [36, 37]. Another meta-analysis showed that the use of an ACEI or ARB in elderly patients with cardiovascular disease may increase the risk of vascular oedema, hypotension, and renal impairment, but cautious use could still reduce the risk of all-cause death, cardiac death, myocardial infarction, heart failure, and other clinical events [38]. Soumerai et al. found that the risk of death was 14% lower in elderly patients with acute myocardial infarction who were treated with beta-blockers at discharge, which was consistent with the results of randomized controlled trials of young and low-risk populations [39]. The results of the present study also showed that a higher degree of EBM compliance corresponded to better prognosis, suggesting that elderly CAD patients should also adhere to the guidelines and EBMs.
Several limitations of this study should be addressed. First, the registry made it difficult to completely avoid selection bias and confounding factors including information of activity of daily livings. In current study, the prescription rate of ACEI/ARBs was higher in those aged 60–75 and > 75 than those aged < 60, which was a converse trend to other EBMs. The possible explain was that ACEI/ARBs was not only an EBMs for ACS, but also used as an antihypertensive agents. Elderly CAD patients were complicated more hypertension than younger patients, and had more chance to take ACEI/ARBs. After excluding the patients with hypertension, the prescription rate of ACEI/ARBs were equal in three groups of different ages. (see Additional files 2) Second, the samples in this single-centre study were subject to geographical restrictions, which affected their representativeness and generalization. Third, patients older than 80 years old are thought to be more insufficient in EBM use than younger patients [40, 41]. We conducted analysis on patients older than 80 but the group sizes (n = 155) was too small to obtain an adequate statistical power. (see Additional files 3 and 4) Finally, this study focused on four types of medications, antiplatelet drugs, statin, beta-blocker and ACEI/ARB. The effects of other medications were not studied. In conclusion, caution must be taken when analysing the results of this study. However, attention should be paid to the insufficient use of EBMs and its potential impact on prognosis in elderly patients with CAD. High-quality research reports are needed to provide more clinical evidence and experience in the use of EBMs in elderly patients with CAD.
Conclusions
Elderly patients with CAD had higher risk of cardiovascular disease but had a lower degree of compliance with EBMs usage to prevent cardiovascular events. Elderly CAD patients, similar to younger CAD patients, could also receive more clinical benefits by strictly adhering to the use of EBMs. Therefore, EBMs should also be actively promoted for elderly CAD patients.
Abbreviations
- ACEI:
-
Angiotensin-converting enzyme inhibitors
- AMI:
-
Acute myocardial infarction
- ANOVA:
-
Analysis of variance
- ARB:
-
Angiotensin-receptor blocker
- CAD:
-
Coronary artery disease
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- CV death:
-
Cardiovascular death
- DBP:
-
Diastolic blood pressure
- EBMs:
-
Evidence-based medications
- ESRD:
-
End stage renal disease
- HDL-C:
-
High-density lipoprotein-cholesterol
- HR:
-
Hazard ratio
- LDL-C:
-
Low-density lipoprotein cholesterol
- NSTEMI:
-
Non-ST segment elevation myocardial infarction
- SBP:
-
Systolic blood pressure
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
References
Celermajer DS, Chow CK, Marijon E, Anstey NM, Woo KS. Cardiovascular disease in the developing world: prevalences, patterns, and the potential of early disease detection. J Am Coll Cardiol. 2012;60(14):1207–16.
Yang G, Wang Y, Zeng Y, Gao GF, Liang X, Zhou M, Wan X, Yu S, Jiang Y, Naghavi M, et al. Rapid health transition in China, 1990-2010: findings from the global burden of disease study 2010. Lancet. 2013;381(9882):1987–2015.
Alexander KP, Newby LK, Cannon CP, Armstrong PW, Gibler WB, Rich MW, Van de Werf F, White HD, Weaver WD, Naylor MD, et al. Acute coronary care in the elderly, part I: non-ST-segment-elevation acute coronary syndromes: a scientific statement for healthcare professionals from the American Heart Association Council on clinical cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation. 2007;115(19):2549–69.
Alexander KP, Newby LK, Armstrong PW, Cannon CP, Gibler WB, Rich MW, Van de Werf F, White HD, Weaver WD, Naylor MD, et al. Acute coronary care in the elderly, part II: ST-segment-elevation myocardial infarction: a scientific statement for healthcare professionals from the American Heart Association Council on clinical cardiology: in collaboration with the Society of Geriatric Cardiology. Circulation. 2007;115(19):2570–89.
Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined--a consensus document of the joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36(3):959–69.
Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, Das SR, de Ferranti S, Despres JP, Fullerton HJ, et al. Heart disease and stroke Statistics-2016 update: a report from the American Heart Association. Circulation. 2016, 133(4):e38–60.
Gao Y, Masoudi FA, Hu S, Li J, Zhang H, Li X, Desai NR, Krumholz HM, Jiang L. Trends in early aspirin use among patients with acute myocardial infarction in China, 2001-2011: the China PEACE-retrospective AMI study. J Am Heart Assoc. 2014;3(5):e001250.
Anderson JL, Adams CD, Antman EM, Bridges CR, Califf RM, Casey DE, Chavey WE, Fesmire FM, Hochman JS, Levin TN et al: ACC/AHA 2007 Guidelines for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction. <span class="subtitle">A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Revise the 2002 Guidelines for the Management of Patients With Unstable Angina/Non–ST-Elevation Myocardial Infarction): <em>Developed in Collaboration with the American College of Emergency Physicians, the Society for Cardiovascular Angiography and Interventions, and the Society of Thoracic Surgeons</em>: <em>Endorsed by the American Association of Cardiovascular and Pulmonary Rehabilitation and the Society for Academic Emergency Medicine</em></span> 2007, 116(7):e148-e304.
Antman EM, Armstrong PW, Green LA, Halasyamani LK, Hochman JS, Krumholz HM, Lamas GA, Smith SC, Hand MM, Bates ER. 2007 focused update of the ACC/AHA 2004 guidelines for the Management of Patients with ST-elevation myocardial infarction. J Am Coll Cardiol. 2008;51(2):210–47.
Kabir SEJ, Chowdhury AW, Amin MG, Alam MS, Sabah KMN, Abdullah AS, Hossain M, Zahid A, Faruk CO, Khan TA: In-Hospital Outcome of Older and Younger Patients with Acute Coronary Syndrome. 2015 2015, 8(1):4.
Public health and aging: Trends in aging—united states and worldwide. Jama. 2003;289(11):1371–3.
Vitale C, Fini M, Spoletini I, Lainscak M, Seferovic P, Rosano GMC. Under-representation of elderly and women in clinical trials. Int J Cardiology. 232:216–21.
Gurwitz JH. Polypharmacy: a new paradigm for quality drug therapy in the elderly? Arch Intern Med. 2004;164(18):1957–9.
Pratt DS, Kaplan MM. Evaluation of abnormal liver-enzyme results in asymptomatic patients. N Engl J Med. 2000;342(17):1266–71.
Wang TY, Gutierrez A, Peterson ED. Percutaneous coronary intervention in the elderly. Nature reviews. Cardiology. 2011;8(2):79–90.
Toth PP. Treatment of dyslipidemia in elderly patients with coronary heart disease. There Are Miles to Go Before We Sleep J Am Coll Cardiol. 2015;66(17):1873–5.
Cholesterol Treatment Trialists C, Baigent C, Blackwell L, Emberson J, Holland LE, Reith C, Bhala N, Peto R, Barnes EH, Keech A, et al. Efficacy and safety of more intensive lowering of LDL cholesterol: a meta-analysis of data from 170,000 participants in 26 randomised trials. Lancet. 2010;376(9753):1670–81.
Setoguchi S, Levin R, Winkelmayer WC. Long-term trends of angiotensin-converting enzyme inhibitor and angiotensin-receptor blocker use after heart failure hospitalization in community-dwelling seniors. Int J Cardiol. 2008;125(2):172–7.
Al-Khadra S, Meisinger C, Amann U, Holle R, Kuch B, Seidl H, Kirchberger I. Secondary prevention medication after myocardial infarction: persistence in elderly people over the course of 1 year. Drugs Aging. 2014;31(7):513–25.
Krumholz HM, Radford MJ, Ellerbeck EF, Hennen J, Meehan TP, Petrillo M, Wang Y, Kresowik TF, Jencks SF. Aspirin in the treatment of acute myocardial infarction in elderly Medicare beneficiaries. Patterns of use and outcomes. Circulation. 1995;92(10):2841–7.
Becker RC, Burns M, Gore JM, Lambrew CT, French WJ, Rogers WJ. Early and pre-discharge aspirin administration among patients with acute myocardial infarction : current clinical practice and trends in the United States. J Thromb Thrombolysis. 2000;9(3):207–15.
Niu S, Zhao D, Zhu J, Liu J, Liu Q, Liu J, Wang W, Smith SC. The association between socioeconomic status of high-risk patients with coronary heart disease and the treatment rates of evidence-based medicine for coronary heart disease secondary prevention in China: results from the bridging the gap on CHD secondary prevention in China (BRIG) project. Am Heart J. 2009;157(4):709–15.
Bi Y, Gao R, Patel A, Su S, Gao W, Hu D, Huang D, Kong L, Qi W, Wu Y. Evidence-based medication use among Chinese patients with acute coronary syndromes at the time of hospital discharge and 1 year after hospitalization: results from the clinical pathways for acute coronary syndromes in China (CPACS) study. Am Heart J. 2009;157(3):509–16.
Krumholz HM, Radford MJ, Ellerbeck EF, Hennen J, Meehan TP, Petrillo MK, Wang Y, Kresowik TF, Jencks SF: Aspirin in the Treatment of Acute Myocardial Infarction in Elderly Medicare Beneficiaries. Circulation 1995, 92(10):2841–2847.
Ma C, Cao J, Lu X, Guo X, Gao Y, Liu XF, Fan L: Cardiovascular and cerebrovascular outcomes in elderly hypertensive patients treated with either ARB or ACEI; 2012.
Gray SL, Lacroix AZ, Aragaki AK, Mcdermott M, Cochrane BB, Kooperberg C, Murray A, Rodriguez BL, Black HR, Woods NF. Angiotensin-converting enzyme inhibitor use and incident frailty in women aged 65 and older: prospective findings from the Women's Health Initiative observational study. J Am Geriatr Soc. 2009;57(2):297.
Gianni M, Bosch J, Pogue J, Probstfield JL, Dagenais GR, Yusuf S, Lonn E. Effect of long-term ACE-inhibitor therapy in elderly vascular disease patients. Eur Heart J. 2007;28(11):1382–8.
Hoes AW. Beta blockers for heart failure. BMJ. 2016;353:i2074.
Boulet LP. Asthma in the elderly patient. Asthma research and practice. 2016;2:3.
Yanagisawa S, Suzuki N, Tanaka T. Poor tolerance of beta-blockers by elderly patients with heart failure. Clin Interv Aging. 2010;5:365–8.
Eichhorn EJ, Young JB. Optimizing the use of beta-blockers in the effective treatment and management of heart failure: a case study approach. Am J Med. 2001;110(Suppl 5A):11S–20S.
Marcum ZA, Hanlon JT, Murray MD. Improving medication adherence and health outcomes in older adults: an evidence-based review of randomized controlled trials. Drugs Aging. 2017;34(3):191–201.
Piepoli MF, Hoes AW, Agewall S, Albus C, Brotons C, Catapano AL, Cooney M, Corra U, Cosyns B, Deaton C. 2016 European guidelines on cardiovascular disease prevention in clinical practice. Eur Heart J. 2016;37(29):2315–81.
Gazzola KM, Vigna GB. Hypolipidemic drugs in elderly subjects: indications and limits. Nutrition Metabolism and Cardiovascular Diseases. 2016;0(0):1064–70.
Rasmussen JN, Chong A, Alter DA: Relationship between adherence to evidence-based pharmacotherapy and long-term mortality after acute myocardial infarction. JAMA 2007, 297(2):177–186.
Gotto AM: Statin Therapy and the Elderly. SAGE Advice? 2007, 115(6):681–683.
Afilalo J, Duque G, Steele R, Jukema JW, de Craen AJ, Eisenberg MJ. Statins for secondary prevention in elderly patients. A hierarchical bayesian meta-analysis J Am Coll Cardiol. 2008;51(1):37–45.
Elgendy IY, Huo T, Chik V, Pepine CJ, Bavry AA. Efficacy and safety of angiotensin receptor blockers in older patients: a meta-analysis of randomized trials. Am J Hypertens. 2015;28(5):576–85.
Soumerai SB, Mclaughlin TJ, Spiegelman D, Hertzmark E, Thibault GE, Goldman L. Adverse outcomes of underuse of beta-blockers in elderly survivors of acute myocardial infarction. JAMA. 1997;277(2):115–21.
Tegn N, Abdelnoor M, Aaberge L, Endresen K, Smith P, Aakhus S, Gjertsen E, Dahl-Hofseth O, Ranhoff AH, Gullestad L, et al. Invasive versus conservative strategy in patients aged 80 years or older with non-ST-elevation myocardial infarction or unstable angina pectoris (after eighty study): an open-label randomised controlled trial. Lancet. 2016;387(10023):1057–65.
Chen B, Zhang D, Zhu T, Wang L, Li C, Wang H, Zhang F, Cao K, Ma W, Yang Z. Immediate and long-term results of coronary angioplasty in patients aged 80 years and older. Cardiol Res Pract. 2010;2010(263685)
Acknowledgements
Not applicable
Funding
This study was funded by the National Natural Science Foundation of China (grant number: 81400267 and 81370219, Beijing, China) and the National High-tech Research and Development Program of China [2012AA02A510, Beijing, China].
Availability of data and materials
The data that support the findings of this study are available from the corresponding author upon reasonable request.
Author information
Authors and Affiliations
Contributions
TLX, MC, DJH and YP participated in study conception and design. FYH, HC, BTH, YWXO and QL performed the acquisition of data and participated in analysis and interpretation of data. XBP, YML, ZLZ and YP drafted the manuscript and YP, MC, YML, and DJH helped in critical review of the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
This study was conducted after the acquisition of written informed consent from the participating patients and upon the approval by the ethics committee of West China Hospital, Sichuan University.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Number of matched pairs, before-matched and c-statistic. (DOCX 16 kb)
Additional file 2:
Discharge prescription of ACEI/ARBs for CAD patients (panel A) and CAD patients without hypertension (panel B) stratified by age. Abbreviations: CAD, coronary artery disease; ACEI, angiotensin-converting enzyme inhibitor; ARBs, angiotensin receptor blockers. (DOCX 95 kb)
Additional file 3:
Multivariate Cox’s proportional hazards regression model each evidence-based medications. Abbreviations: CAD: coronary artery disease, CI: confidence interval, CV death: cardiovascular death, HR: hazard ratio, LDL-C: low-density lipoprotein-cholesterol, STEMI: ST-segment elevated myocardial infarction. Adjusted factor: sex, history of hypertension, history of diabetes mellitus, and history of heart failure, history of dyslipidemia, smoking status, eGFR and hepatic enzymes. (DOCX 13 kb)
Additional file 4:
Multivariate Cox’s proportional hazards regression model on combination therapy of EBMs. Adjusted factor: sex, history of hypertension, history of diabetes mellitus, and history of heart failure, history of dyslipidemia, smoking status, eGFR and hepatic enzymes. Model 0: no medication; model 1: prescribed 1 type of EBMs; model 2, prescribed 2 types of EBMs; model 3, prescribed all 3 types of EBMs. Three types of EBMs included: statin, beta-blockers, and RAAS inhibitors (ACEIs or ARBs). Abbreviations: EBMs: evidence-based medications, CAD: coronary artery disease, CI: confidence interval, CV death: cardiovascular death, HR: hazard ratio. (DOCX 13 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Xia, Tl., Huang, Fy., Li, Ym. et al. The impact of age on the implementation of evidence-based medications in patients with coronary artery disease and its prognostic significance: a retrospective cohort study. BMC Public Health 18, 150 (2018). https://doi.org/10.1186/s12889-018-5049-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12889-018-5049-x