Abstract
Background
Decreased perfusion in the lower extremities is one of the several adverse effects of placing patients in a lithotomy or Trendelenburg position during surgery. This study aimed to evaluate the effects of patient positioning in lower limb perfusion patients undergoing robotic-assisted laparoscopic radical prostatectomy (RARP) using near-infrared spectroscopy (NIRS).
Methods
This observation study comprised 30 consenting males with American Society of Anaesthesiologists physical status classes I and II (age range, ≥20 to < 80 years). Regional saturation of oxygen measurements was obtained using an INVOS™ oximeter (Somanetics, Troy, MI, USA). A NIRS sensor was positioned on the surface of the skin at the mid-diaphyseal region of the calf muscles (the gastrocnemius and soleus), over the posterior compartment, in the right lower leg. Regional saturation of oxygen (rSO2) was sampled during the following time points: before and 5 min after induction of anaesthesia (T0,T1); 5 min after establishment of pneumoperitoneum in a 0° lithotomy position (T2); 5 min after a 25° Trendelenburg position (T3); 30, 60, 90 and 120 min after pneumoperitoneum in a Trendelenburg position (T4, T5, T6 and T7, respectively); after desufflation in a supine position (T8); and after tracheal extubation (T9).
Results
Lower limb perfusion evaluated by NIRS was increased after induction of anaesthesia and maintained during steep Trendelenburg positions in RARP patients with no risk for lower limb compartment syndrome (LLCS) (T0:65 ± 7.2%, T1:69 ± 6.1%, T2:70±:6.1%, T3:68 ± 6.7%, T4:66 ± 7.5%, T5:67 ± 6.9%, T6:68 ± 7.2%, T8:73 ± 7.2%, T9:71 ± 7.9%, respectively).
Conclusions
Lower limb perfusion evaluated by NIRS was maintained during the RARP procedure. Correct patient positioning and careful assessment of risk factors such as vascular morbidity could be important for the prevention of LLCS during RARP.
Similar content being viewed by others
Background
Robotic-assisted laparoscopic radical prostatectomy (RARP) is one of the most commonly performed robotic-assisted surgical procedures worldwide. In RARP, the patient is placed in the lithotomy position and pneumoperitoneum is established, following which the patient is placed in the steep Trendelenburg position. The combination of lithotomy position, pneumoperitoneum, and steep Trendelenburg positioning may cause significant and potentially adverse cardiovascular, respiratory and neuro-physiological changes in the body [1]. The combination of these positions is also thought to decrease perfusion in the lower extremities by reducing blood pressure [2].
Lower limb compartment syndrome (LLCS) is a rare but serious complication of surgery in the lithotomy position, with an estimated incidence of one in 3500 cases [3]. However, in a recent study conducted in the United Kingdom, the incidence of the LLCS during RARP was reported to occur more frequently than previously recognised [4]. Tissue ischaemia with low perfusion is one of the most common causes of LLCS; nonetheless, the effect of the position of the patient on lower limb perfusion during RARP remains unclear. Near-infrared spectroscopy (NIRS) has been recommended as a method to detect perfusion deficits in peripheral tissues [5]. Therefore, the present study aimed to evaluate the effect of patient positioning during RARP by examining the changes in regional saturation of oxygen (rSO2) in the lower limbs using NIRS.
Methods
Thirty adult males (American Society of Anaesthesiologists class I and II physical status) scheduled for RARP at the Ehime University Hospital, Toon, Ehime, Japan, from September 2013 to May 2014 were consecutively selected. Patients with previous episodes of peripheral vascular disease and those who were morbidly obese (body mass index > 35 kg/m2) were excluded from the study. Approval for the study was obtained from the institutional review board (registration number 1308010), and informed consent was obtained from the patients. The study was registered with the UMIN Clinical Trials Registry (000032897).
A standard anaesthetic technique was used, wherein routine monitoring of non-invasive arterial blood pressure, electrocardiogram (ECG) and oxygen saturation (SpO2) was conducted on arrival at the operating room. Anaesthesia was induced with propofol (1.5–2 mg/kg), remifentanil (0.15–0.3 μg/kg/min) and rocuronium bromide (0.8 mg/kg) and maintained using desflurane (4–6%), remifentanil (0.15–0.3 μg/kg/min) and rocuronium bromide (5–7 μg/kg/min). The ventilator settings were as follows: tidal volume, 8–10 mL/kg body weight; inspiratory:expiratory ratio, 1:2 or 1:1.5; inspired O2 fraction, 0.6 with air; and inspiratory fresh gas flow, 2 L/min. The respiratory rate was adjusted to 8–16 /min in order to maintain an end-tidal CO2 (ETCO2) pressure of 30–45 mmHg. After induction of anaesthesia, a 22-G radial artery catheter was inserted for blood sampling and to monitor the continuous arterial pressure and the minimally invasive cardiac output using FloTrac™ (Edwards LifeSciences, Irvine, CA, USA). The mean arterial pressure (MAP) was maintained above 60 mmHg.
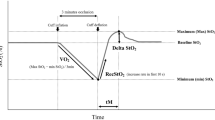
A continuous dual-wavelength near-infrared spectrometer, INVOS™ oximeter (Somanetics, Troy, MI, USA), was used to determine the rSO2 measurements. A NIRS sensor was positioned on the surface of the skin, in the mid-diaphyseal region of the calf muscles (the gastrocnemius and soleus), over the posterior compartment of the right lower leg. For cerebral oximetry, NIRS sensors were placed unilaterally at least 2 cm above the eyebrow on the right side of the forehead according to manufacturer’s instructions. Both sensors were placed before the induction of anaesthesia during pre-oxygenation with 100% O2. A change of more than 8 percentage points in lower limb rSO2 was defined as clinically relevant [6].
For the lithotomy position, devices for vacuum-packed positioning and spreading the legs apart were used to absorb compressive forces, prevent uneven and potentially excessive pressure distribution and prevent excessive stretching or compression. After positioning, the compressive forces were measured using a portable pressure measuring device (PalmQ™, CAPE, Yokosuka, Japan). The positions were then adjusted and maintained in such a manner that the pressure values in the shoulder, hip and calf were below 30 mmHg.
The abdominal cavity was insufflated with CO2 gas at a pressure of 12 mmHg, following which the patients were placed in a 25° Trendelenburg position during surgery. The procedure was performed by a surgeon on a control table located away from the operating table, using the da Vinci robot surgical system (Intuitive Surgical, Sunnyvale, CA, USA).
MAP and rSO2 were recorded before the induction of anaesthesia. ETCO2, cardiac index and stroke volume variations were monitored after ventilation was controlled. The recorded values were sampled at the following time points: before induction of anaesthesia (T0); 5 min after induction of anaesthesia (T1); 5 min after establishing pneumoperitoneum with the patient in a 0° lithotomy position (T2); 5 min after the patient was placed in a 25° Trendelenburg position (T3); 30, 60, 90 and 120 min after establishment of pneumoperitoneum in the Trendelenburg position (T4, T5, T6 and T7, respectively); after desufflation in a supine position (T8); and after tracheal extubation (T9). The levels of haemoglobin, arterial partial pressure of oxygen (PaO2) and arterial partial pressure of carbon dioxide (PaCO2) were measured by arterial blood gas analysis at T1, T2, T3 and T7.
To calculate the sample size, the standard deviation of the baseline rSO2 of the first five patients (7.3) was used. Twenty-six patients with an error of 0.05 and a power of 80% were required to determine the changes in lower limb rSO2 (8 percentage points) in the current study. Assuming a dropout rate of 15%, 30 patients were recruited in this study.
All statistical analyses were performed using IBM SPSS Statistics 23 (SPSS Inc., Chicago, IL, USA). Continuous variables are presented as means and standard deviations. Repeated measured variables were analysed using a linear mixed model, with the patient indicator as random effect and time as fixed effects. Post-hoc analysis was performed with Bonferroni correction to adjust for multiple comparisons when the interactions between times were significant. All of the reported p values are two sided, and a p value < 0.05 was considered significant.
Results
The demographics of the study participants are summarised in Table 1. No cases of LLCS were reported, none of the patients required blood transfusions, and all patients were satisfied with the surgical procedure.
Significant changes in rSO2 values (p < 0.01) were observed in the lower limb (Fig. 1) (T0:65 ± 7.2%, T1:69 ± 6.1%, T2:70±:6.1%, T3:68 ± 6.7%, T4:66 ± 7.5%, T5:67 ± 6.9%, T6:68 ± 7.2%, T8:73 ± 7.2%, T9:71 ± 7.9%, respectively). The values increased after induction of anaesthesia, establishment of pneumoperitoneum in the 0° lithotomy position, placing the patient in the Trendelenburg position (at 5 and 120 min), desufflation in the supine position and tracheal extubation when compared to the baseline values. No significant changes in rSO2 were noted between the time points during the Trendelenburg positions. Furthermore, the lower limb rSO2 values decreased by over 8 percentage points from the baseline after induction of anaesthesia in two patients and at 5 min after steep Trendelenburg positions in four patients. In addition, six patients demonstrated a decrease of more than 8 percentage points in lower limb rSO2 values during the steep Trendelenburg positions.
Changes in cerebral rSO2 were also found to be statistically significant (p < 0.01) in the current study (Fig. 2). A decrease in cerebral rSO2 values was noted after induction of anaesthesia; however, the values returned to baseline during pneumoperitoneum at the Trendelenburg position. One patient presented with a decrease of < 75% from the baseline value 5 min after induction of anaesthesia (probably due to cerebral desaturation) and was treated with ephedrine (intravenous; 8 mg) to increase the cerebral perfusion pressure.
MAP (A) decreased after induction of anaesthesia and continued to show a decreasing trend throughout the operation (Fig. 3). Cardiac index (B) increased at 5 min after a Trendelenburg position and after desufflation in a supine position when compared with the baseline values. Stroke volume variations (C) were temporarily recovered at 5 min after a Trendelenburg position but increased at other time points during the Trendelenburg position when compared with the values obtained at 5 min after induction of anaesthesia. ETCO2 (D) increased 60 min after establishment of pneumoperitoneum in a Trendelenburg position when compared to 5 min after induction of anaesthesia. Serum laboratory data related to the compartment syndrome (e.g. creatine kinase, lactate dehydrogenase) showed no changes when the preoperative values were compared with those on postoperative day one.
Discussion
In the present study, lower limb perfusion evaluated by NIRS was found to be increased after induction of anaesthesia and maintained during the steep Trendelenburg position in RARP patients with no risk of LLCS.
LLCS is a rare but serious complication of RARP [7, 8]. The clinical diagnosis of acute compartment syndrome is difficult as the traditional use of the ‘6 Ps’ to diagnose LLCS has low specificity and is especially difficult to evaluate during the RARP procedure [9]. NIRS allows for the continuous monitoring of the tissue oxygenation of limbs at risk for ischaemia throughout the operative period. Lower limb NIRS was used to confirm the development of compartment syndrome after surgical cut-down for vascular access [10] and in a model of acute LLCS [6, 11]. To the best of our knowledge, this is the first clinical study to demonstrate the use of NIRS to assess lower limb perfusion during the RARP procedure.
There are several mechanisms for intraoperative LLCS. In RARP procedure, the patient’s legs are above the heart level in the lithotomy position and steep Trendelenburg position, and the blood pressure of the lower limb may decrease if these positions are held for prolonged periods. Decreases in blood flow may result in reduced oxygen supply within the compartment and lead to an inflammatory response, release of cytokines, capillary leakage and interstitial oedema. These responses increase the pressure within the compartment, escalating into a self-perpetuating cascade of worsening swelling. Additionally, direct external pressure from the calf support positioning device can also exacerbate the compartmental pressure. When the pressure rises above critical levels, intra-compartmental structures such as nerves, blood vessels and muscles are damaged. Obesity, peripheral vascular disease, prolonged console time and lack of experienced surgeons are increasing the risk of LLCS during RARP [4].
As reported previously, the cardiovascular factors that affect peripheral perfusion pressure, such as cardiac index, heart rate and stroke volume, were shown to decrease significantly after induction of anaesthesia in RARP patients [12]. Additionally, we observed that stroke volume variations, a surrogate marker of cardiac preload, were significantly increased during the Trendelenburg positions, except at 5 min after the Trendelenburg position. These findings suggested that the changes in cardiovascular physiology that occurred during RARP had negative effects on systemic perfusion and may affect cerebral rSO2. However, instead of this negative physiological change, lower limb rSO2 was increased after induction of anaesthesia and maintained during steep Trendelenburg positions in RARP patients. Volatile anaesthetics such as sevoflurane induced marked changes in muscle microcirculation, increase in tissue blood volume, decreased microvascular resistance and compliance, and decreased muscle oxygen consumption [13]. This favourable effect of volatile anaesthetics on microcirculation may be one of the mechanisms by which lower limb rSO2 is maintained during the RARP procedure. High inspiratory fractions of oxygen also help in increasing lower limb oxygenation. Moreover, hypercapnia is known to be beneficial for peripheral microcirculation [14]. Lower limb oxygenation may be compensated by increasing peripheral microcirculation. Therefore, limb positioning to avoid excessive compression force is crucial for the prevention of LLCS during RARP.
One of the limitations of this study is that it is not known whether maintenance of lower limb rSO2 during RARP is genuinely conducive for reducing the incidence of LLCS. Further studies are required to explore the perfusion pressure, microcirculation and clinical threshold of rSO2 values. Furthermore, different mechanisms of muscle microcirculation have been reported using different anaesthetics [15]. Therefore, the effects of various combinations of anaesthetics for lower limb perfusion during RARP must also be explored.
Conclusions
In conclusion, lower limb perfusion evaluated by NIRS was maintained during the RARP procedure, probably by an increase in microcirculation. Hence, correct patient positioning and careful assessment of risk factors, such as vascular morbidity, might be important for the prevention of LLCS during RARP.
Abbreviations
- CI:
-
Cardiac index
- ECG:
-
Electrocardiogram
- ETCO2 :
-
End-tidal CO2
- LLCS:
-
Lower limb compartment syndrome
- MAP:
-
Mean arterial pressure
- NIRS:
-
Near-infrared spectroscopy
- RARP:
-
Robotic-assisted laparoscopic radical prostatectomy
- rSO2 :
-
Regional saturation of oxygen
- SpO2 :
-
Oxygen saturation
- SVV:
-
Stroke volume variations
References
Awad H, Walker CM, Shaikh M, Dimitrova GT, Abaza R, O'Hara J. Anesthetic considerations for robotic prostatectomy: a review of the literature. J Clin Anesth. 2012;24:494–504.
Meyer RS, White KK, Smith JM, Groppo ER, Mubarak SJ, Hargens AR. Intramuscular and blood pressures in legs positioned in the hemilithotomy position: clarification of risk factors for well-leg acute compartment syndrome. J Bone Joint Surg Am. 2002;84:1829–35.
Mumtaz FH, Chew H, Gelister JS. Lower limb compartment syndrome associated with the lithotomy position: concepts and perspectives for the urologist. BJU Int. 2002;90:792–9.
Pridgeon S, Bishop CV, Adshead J. Lower limb compartment syndrome as a complication of robot-assisted radical prostatectomy: the UK experience. BJU Int. 2013;112:485–8.
Murkin JM, Arango M. Near-infrared spectroscopy as an index of brain and tissue oxygenation. Br J Anaesth. 2009;103:i3–13.
Reisman WM, Shuler MS, Kinsey TL, Cole AL, Whitesides TE Jr, Davila MG, Smith EK, Moore TJ. Relationship between near infrared spectroscopy and intra-compartmental pressures. J Emerg Med. 2013;44:292–8.
Raman SR, Jamil Z. Well leg compartment syndrome after robotic prostatectomy: a word of caution. J Robot Surg. 2009;3:105–7.
Yang RH, Chu YK, Huang CW. Compartment syndrome following robotic-assisted prostatectomy: rhabdomyolysis in bone scintigraphy. Clin Nucl Med. 2013;38:365–6.
Ulmer T. The clinical diagnosis of compartment syndrome of the lower leg: are clinical findings predictive of the disorder? J Orthop Trauma. 2002;16:572–7.
Tobias JD, Hoernschemeyer DG. Near-infrared spectroscopy identifies compartment syndrome in an infant. J Pediatr Orthop. 2007;27:311–3.
Gentilello LM, Sanzone A, Wang L, Liu PY, Robinson L. Near-infrared spectroscopy versus compartment pressure for the diagnosis of lower extremity compartmental syndrome using electromyography-determined measurements of neuromuscular function. J Trauma. 2001;51:1–8.
Darlong V, Kunhabdulla NP, Pandey R. Hemodynamic changes during robotic radical prostatectomy. Saudi J Anaesth. 2012;6:213–8.
De Blasi RA, Palmisani S, Boezi M, Arcioni R, Collini S, Troisi F, Pinto G. Effects of remifentanil-based general anaesthesia with propofol or sevoflurane on muscle microcirculation as assessed by near-infrared spectroscopy. Br J Anaesth. 2008;101:171–7.
Hassett P, Laffey JG. Permissive hypercapnia: balancing risks and benefits in the peripheral microcirculation. Crit Care Med. 2007;35:2229–31.
Turek Z, Sykora R, Matejovic M, Cerny V. Anesthesia and the microcirculation. Semin Cardiothorac Vasc Anesth. 2009;13:249–58.
Acknowledgements
The authors thank all staff in the department of anaesthesia and operating rooms of Ehime University Hospital, Toon, Ehime, Japan for their help in the study.
Availability of data and materials
All data generated or analysed during this study are included in this published article and are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
KT: ethics approval, study design, data collection and analysis, drafted the manuscript and reviewed it for important intellectual content; SK: data analysis and reviewed the manuscript for important intellectual content; IS: data analysis and reviewed the manuscript for important intellectual content; TY: data analysis and reviewed the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the local institutional review board of the Ehime University Graduate School of Medicine (registration number 1308010). After a detailed explanation written informed consent was obtained from 30 patients scheduled for RARP.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Takechi, K., Kitamura, S., Shimizu, I. et al. Lower limb perfusion during robotic-assisted laparoscopic radical prostatectomy evaluated by near-infrared spectroscopy: an observational prospective study. BMC Anesthesiol 18, 114 (2018). https://doi.org/10.1186/s12871-018-0567-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12871-018-0567-8