Abstract
Background
Aromatase inhibitors (AI) have been introduced to reduce estrogen exposure in women with estrogen-sensitive cancer undergoing ovarian stimulation for oocyte/embryo cryopreservation. There have been questions regarding whether the addition of AI and the presence of BRCA mutations affect cycle outcomes. We sought to determine the impact of letrozole and BRCA mutations on fertility preservation (FP) cycle outcomes of patients undergoing ovarian stimulation with an antagonist protocol.
Methods
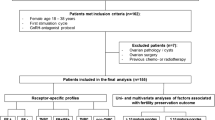
The data were generated by the secondary analysis of a prospective database of all females diagnosed with cancer who underwent embryo or oocyte cryopreservation for FP. The final analysis included 145 patients stimulated with an antagonist protocol either using letrozole combined with recombinant follicle-stimulating hormone (rFSH; LF, n = 118) or rFSH alone (FA, n = 24).
Results
The mean number of total (15.6 [7.9] vs 10.2 [7.8]; P =.004) and mature oocytes (10.4 [5.1] vs 7.8 [3.5]; P =.044) and embryos frozen (7.7 [5.3] vs 5.3 [2.7]; P =.043) were significantly higher after LF stimulation versus FA. In the LF group, women with BRCA mutations produced significantly fewer oocytes (11.0 [8.0] vs 16.4 [7.7], P =.015) and embryos (5.1 [4.4] vs 8.2 [4.7], P =.013), compared to those who were mutation negative. After adjusting for age, body mass index, baseline FSH level, and BRCA status, LF protocol still resulted in higher number of total oocytes (95% confidence interval [CI]: 1.9 to 3.6; P =.002) mature oocyte (95% CI: 0.3 to 1.4; P =.028), and embryo yield (95% CI: 0.7 to 1.4; P =.015).
Conclusion
In women with cancer undergoing FP, letrozole appears to enhance response to ovarian stimulation while the presence of BRCA mutations is associated with lower oocyte and embryo yield.
Similar content being viewed by others
References
American Cancer Society. Cancer Facts & Figures 2016. Atlanta, Georgia: American Cancer Society; 2016.
Siegel R, Naishadham D, Jemal A. Cancer statistics, 2012. Ca Cancer J Clin 2012;62(1):10–29.
Letourneau JM, Ebbel EE, Katz PP, et al. Pretreatment fertility counseling and fertility preservation improve quality of life in reproductive age women with cancer. Cancer. 2012;118(6):1710–1707.
Turan V, Oktay K. Sexual and fertility adverse effects associated with chemotherapy treatment in women. Expert Opin Drug Saf. 2014;13(6):775–783.
Rodriguez-Wallberg KA, Oktay K. Recent advances in oocyte and ovarian tissue cryopreservation and transplantation. Best Pract Res Clin Obstet Gynaecol. 2012;26(3):391–405.
Requena A, Herrero J, Landeras J, et al. Use of letrozole in assisted reproduction: a systematic review and meta-analysis. Hum Reprod Update. 2008;14(6):571–582.
Bedoschi G, Oktay K. Current approach to fertility preservation by embryo cryopreservation. Fertil Steril. 2013;99(6):1496–502.
Loren AW, Mangu PB, Beck LN, et al. Fertility preservation for patients with cancer: American Society of Clinical Oncology clinical practice guideline update. J Clin Oncol. 2013;31(19):2500–2510.
Sonmezer M, Oktay K. Fertility preservation in young women undergoing breast cancer therapy. Oncologist. 2006;11(5):422–434.
Oktay K, Buyuk E, Libertella N, Akar M, Rosenwaks Z. Fertility preservation in breast cancer patients: a prospective controlled comparison of ovarian stimulation with tamoxifen and letrozole for embryo cryopreservation. J Clin Oncol. 2005;23(19):4347–4353.
Azim AA, Costantini-Ferrando M, Oktay K. Safety of fertility preservation by ovarian stimulation with letrozole and gonadotropins in patients with breast cancer: a prospective controlled study. J Clin Oncol. 2008;26(16):2630–2635.
Kim J, Turan V, Oktay K. Long-Term Safety of letrozole and gonadotropin stimulation for fertility preservation in women with breast cancer. J Clin Endocrinol Metab. 2016;101(4):1364–1371.
Turan V, Bedoschi G, Moy F, Oktay K. Safety and feasibility of performing two consecutive ovarian stimulation cycles with the use of letrozole-gonadotropin protocol for fertility preservation in breast cancer patients. Fertil Steril. 2013;100(6):1681–1685.
Oktay K, Turan V, Bedoschi G, Pacheco FS, Moy F. Fertility preservation success subsequent to concurrent aromatase inhibitor treatment and ovarian stimulation in women with breast cancer. J Clin Oncol. 2015;33(22):2424–2429.
Cole P, Robinson C. Mechanism and inhibition of cytochrome P-450 aromatase. J Med Chem. 1990;33(11):2933–2942.
Verpoest WM, Kolibianakis E, Papanikolaou E, Smitz J, Van Steirteghem A, Devroey P. Aromatase inhibitors in ovarian stimulation for IVF/ICSI: a pilot study. Reprod Biomed Online. 2006;13(2):166–172.
Welt CK, Martin KA, Taylor AE, et al. Frequency modulation of follicle-stimulating hormone during the luteal-follicular transition: evidence for FSH control of inhibin B in normal women. J Clin Endocrinol Metab. 1997;82(8):2645–2652.
Hu Y, Cortvrindt R, Smitz J. Effects of aromatase inhibition on in vitro follicle and oocyte development analyzed by early preantral mouse follicle culture. Mol Reprod Dev. 2002;61(4):549–559.
Kar S. Current evidence supporting “letrozole” for ovulation induction. J Hum Reprod Sci. 2013;6(2):93–98.
Oktay K, Hourvitz A, Sahin G, Oktem O, Safro B, Cil A, Bang H. Letrozole reduces estrogen and gonadotropin exposure in women with breast cancer undergoing ovarian stimulation before chemotherapy. J Clin Endocrinol Metab. 2006;91(10):3885–3890.
Yaghjyan L, Colditz GA. Estrogens in the breast tissue: a systematic review. Cancer Causes Control. 2011;22(4):529–540.
Narod SA. Should all women with breast cancer be tested for BRCA mutations at the time of diagnosis? J Clin Oncol. 2012;30(1):2–3.
Reddy J, Turan V, Bedoschi G, Moy F, Oktay K. Triggering final oocyte maturation with gonadotropin-releasing hormone agonist (GnRHa) versus human chorionic gonadotropin (hCG) in breast cancer patients undergoing fertility preservation: an extended experience. J Assist Reprod Genet. 2014;31(7):927–932.
Oktay K, Kim JY, Barad D, Babayev SN. Association of BRCA1 mutations with occult primary ovarian insufficiency: a possible explanation for the link between infertility and breast/ovarian cancer risks. J Clin Oncol. 2010;28(2):240–244.
Titus S, Li F, Stobezki R, et al. Impairment of BRCA1-related DNA double-strand break repair leads to ovarian aging in mice and humans. Sci Transl Med. 2013;5(172):172ra21.
Garcia-Velasco J, Moreno L, et al. The aromatase inhibitor letrozole increases the concentration of intraovarian androgens and improves in vitro fertilization outcome in low responder patients: a pilot study. Fertil Steril. 2005;84(1):82–87.
Weil S, Vendola K, Zhou J, Bondy CA. Androgen and follicle-stimulating hormone interactions in primate ovarian follicle development. J Clin Endocrinol Metab. 1999;84(8):2951–2956.
Murray AA, Gosden RG, Allison V, Spears N. Effect of androgens on the development of mouse follicles growing in vitro. J Reprod Fertil. 1998;113(1):27–33.
Checa Vizcaíno MA, Corchado AR, Cuadri ME, Comadran MG, Brassesco M, Carreras R. The effects of letrozole on ovarian stimulation for fertility preservation in cancer-affected women. Reprod Biomed Online. 2012;24(6):606–610.
Diamond MP, Legro RS, Coutifaris C, et al. NICHD reproductive medicine network. letrozole, gonadotropin, or clomiphene for unexplained infertility. N Engl J Med. 2015;373(13):1230–1240.
Domingo J, Guillén V, Ayllón Y, et al. Ovarian response to controlled ovarian hyperstimulation in cancer patients is diminished even before oncological treatment. Fertil Steril. 2012;97(4):930–934.
Moria A, Das M, Shehata F, Holzer H, Son WY, Tulandi T. Ovarian reserve and oocyte maturity in women with malignancy undergoing in vitro maturation treatment. Fertil Steril. 2011;95(5):1621–1623.
Rzepka-Gorska I, Tarnowski B, Chudecka-Głaz A, Gorski B, Zielinska D, Tołoczko-Grabarek A. Premature menopause in patients with BRCA1 gene mutation. Breast Cancer Res Treat. 2006;100(1):59–63.
Wang ET, Pisarska MD, Bresee C, et al. BRCA1 germline mutations may be associated with reduced ovarian reserve. Fertil Steril. 2014;102(6):1723–1728.
Pavone ME, Hirshfeld-Cytron J, Tingen C, et al. Human ovarian tissue cortex surrounding benign and malignant lesions. Reprod Sci. 2014;21(5):582–589.
Lin WT, Beattie M, Chen LM, et al. Comparison of age at natural menopause in BRCA1/2 mutation carriers with a non-clinic-based sample of women in northern California. Cancer. 2013;119(9):1652–1659.
Phillips KA, Collins IM, Milne RL, et al. Kathleen cuningham consortium for research into familial breast cancer. Anti-Müllerian hormone serum concentrations of women with germline BRCA1 or BRCA2 mutations. Hum Reprod. 2016;31(5):1126–1132.
Oktay K, Turan V, Titus S, Stobezki R, Liu L. BRCA mutations, DNA repair deficiency, and ovarian aging. Biol Reprod. 2015;93(3):67.
Xiong B, Li S, Ai JS, et al. BRCA1 is required for meiotic spindle assembly and spindle assembly checkpoint activation in mouse oocytes. Biol Reprod. 2008;79(4):718–726.
Zhang D, Zhang X, Zeng M, et al. Increased DNA damage and repair deficiency in granulosa cells are associated with ovarian aging in rhesus monkey. J Assist Reprod Genet. 2015;32(7):1069–1078.
Li W, Titus S, Moy F, Ginsburg E, Oktay K. Ovarian aging in women with germline BRCA mutation. The Journal of Clinical Endocrinology & Metabolism, jc.2017–00765, https://doi.org/10.1210/jc.2017-00765. Published 16 August 2017.
Shapira M, Raanani H, Feldman B, et al. BRCA mutation carriers show normal ovarian response in in vitro fertilization cycles. Fertil Steril. 2015;104(5):1162–1167.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Turan, V., Bedoschi, G., Emirdar, V. et al. Ovarian Stimulation in Patients With Cancer: Impact of Letrozole and BRCA Mutations on Fertility Preservation Cycle Outcomes. Reprod. Sci. 25, 26–32 (2018). https://doi.org/10.1177/1933719117728800
Published:
Issue Date:
DOI: https://doi.org/10.1177/1933719117728800