Abstract
Polychlorinated biphenyls (PCBs) are one of the most common endocrine-disrupting chemicals and have obvious toxicity on human reproductive development. The aim of our study was to investigate the toxicity of chronic 2,3’,4,4’,5-pentachlorobiphenyl (PCB 118) exposure on embryo implantation and endometrial receptivity, with the possible mechanism of DNA methylation involved. Virgin CD-I female mice (3 weeks old) were housed and orally treated with PCB 118 (0, 1, 10, 100 Hg/kg) for a month. After mating with fertile males, the pregnant mice were killed on gestation day 4.5. Compared with the control group, implantation failures were observed in 1 p.g/kg PCB 118- and 100 p.g/kg PCB 118-treated groups. Abnormal endometrial morphology with open uterine lumens and densely compact stromal cells and poorly developed pinopodes were substantially in response to PCB 118 doses above, as well as the significant downregulation of implantation-associated genes (estrogen receptor I, homeobox A10 [HOXA10], integrin subunit beta 3) and hypermethylation in the promoter region of HOXA10 further. It was confirmed that chronic exposure to PCB 118 produced an increased number of implantation failures in association with a defective uterine morphology during the implantation period. Alterations in methylation of HOXA10 could explain, at least in part, the mechanism of effects of PCB 118 exposure on the implantation process.
Similar content being viewed by others
References
Bergman A, Ryden A, Law RJ, et al. A novel abbreviation standard for organobromine, organochlorine and organophosphorous flame retardants and some characteristics of the chemicals. Environ Int. 2012;49:57–82.
Hsu PC, Huang W, Yao WJ, Wu MH, Guo YL, Lambert GH. Sperm changes in men exposed to polychlorinated biphenyls and dibenzofurans. JAMA. 2003;289(22):2943–2944.
Gerhard I, Monga B, Krahe J, Runnebaum B. Chlorinated hydrocarbons in infertile women. Environ Res. 1999;80(4):299–310.
Toft G, Axmon A, Lindh CH, Giwercman A, Bonde JP. Menstrual cycle characteristics in European and Inuit women exposed to persistent organochlorine pollutants. Hum Reprod. 2008;23(1):193–200.
Tsukimori K, Tokunaga S, Shibata S, et al. Long-term effects of polychlorinated biphenyls and dioxins on pregnancy outcomes in women affected by the Yusho incident. Environ Health Perspect. 2008;116(5):626–630.
Negri E, Bosetti C, Fattore E, La Vecchia C. Environmental exposure to polychlorinated biphenyls (PCBs) and breast cancer: a systematic review of the epidemiological evidence. Eur J Cancer Prev. 2003;12(6):509–516.
Ritter R, Scheringer M, MacLeod M, Moeckel C, Jones KC, Hungerbuhler K. Intrinsic human elimination half-lives of poly-chlorinated biphenyls derived from the temporal evolution of cross-sectional biomonitoring data from the United Kingdom. Environ Health Perspect. 2011;119(2):225–231.
Covaci A, Jorens P, Jacquemyn Y, Schepens P. Distribution of PCBs and organochlorine pesticides in umbilical cord and maternal serum. Sci Total Environ. 2002;298(1-3):45–53.
De Felip E, di Domenico A, Miniero R, Silvestroni L. Polychlor-obiphenyls and other organochlorine compounds in human follicular fluid. Chemosphere. 2004;54(10):1445–1449.
Cok I, Donmez MK, Satiroglu MH, et al. Concentrations of poly-chlorinated dibenzo-p-dioxins (PCDDs), polychlorinated diben-zofurans (PCDFs), and dioxin-like PCBs in adipose tissue of infertile men. Arch Environ Contam Toxicol. 2008;55(1):143–152.
Alivernini S, Battistelli CL. Turrio-Baldassarri L. Human milk as a vector and an indicator of exposure to PCBs and PBDEs: temporal trend of samples collected in Rome. Bull Environ Contam Toxicol. 2011;87(1):21–25.
Meeker JD, Maity A, Missmer SA, et al. Serum concentrations of polychlorinated biphenyls in relation to in vitro fertilization outcomes. Environ Health Perspect. 2011;119(7):1010–1016.
Barrett Jr. PCBs may impede IVF success: failed embryo implantation linked to exposure. Environ Health Perspect. 2011;119(7): A307.
Johnson PI, Altshul L, Cramer DW, Missmer SA, Hauser R, Meeker JD. Serum and follicular fluid concentrations of polybro-minated diphenyl ethers and in-vitro fertilization outcome. Environ Int. 2012;45:9–14.
Kuriyama SN, Chahoud I. In utero exposure to low-dose 2,3′,4,4′,5-pentachlorobiphenyl (PCB 118) impairs male fertility and alters neurobehavior in rat offspring. Toxicology. 2004;202(3):185–197.
Fritz M, Speroff L. Clinical Gynecologic Endocrinology and Infertility. Philadelphia, PA: Lippincott Williams & Wilkins; 2011:121–156.
Achache H, Revel A. Endometrial receptivity markers, the journey to successful embryo implantation. Hum Reprod Update. 2006;12(6):731–746.
Stavreus-Evers A, Nikas G, Sahlin L, Eriksson H, Landgren BM. Formation of pinopodes in human endometrium is associated with the concentrations of progesterone and progesterone receptors. Fertil Steril. 2001;76(4):782–791.
Nikas G, Psychoyos A. Uterine pinopodes in peri-implantation human endometrium. Clinical relevance. Ann N Y Acad Sci. 1997;816:129–142.
Xu B, Sun X, Li L, Wu L, Zhang A, Feng Y. Pinopodes, leukemia inhibitory factor, integrin-beta3, and mucin-1 expression in the peri-implantation endometrium of women with unexplained recurrent pregnancy loss. Fertil Steril. 2012;98(2):389–395.
Nikas G, Develioglu OH, Toner JP, Jones HJ. Endometrial pinopodes indicate a shift in the window of receptivity in IVF cycles. Hum Reprod. 1999;14(3):787–792.
Bagot CN, Kliman HJ, Taylor HS. Maternal Hoxa10 is required for pinopod formation in the development of mouse uterine receptivity to embryo implantation. Dev Dyn. 2001;222(3):538–544.
Nikas G, Makrigiannakis A. Endometrial pinopodes and uterine receptivity. Ann N Y Acad Sci. 2003;997:120–123.
Kim JJ, Fazleabas AT. Uterine receptivity and implantation: the regulation and action of insulin-like growth factor binding protein-1 (IGFBP-1), HOXA10 and forkhead transcription factor-1 (FOXO-1) in the baboon endometrium. Reprod Biol Endocrinol. 2004;2:34.
Kaneko Y, Day ML, Murphy CR. Integrin beta3 in rat blastocysts and epithelial cells is essential for implantation in vitro: studies with Ishikawa cells and small interfering RNA transfection. Hum Reprod. 2011;26(7):1665–1674.
Coughlan C, Sinagra M, Ledger W, Li TC, Laird S. Endometrial integrin expression in women with recurrent implantation failure after in vitro fertilization and its relationship to pregnancy outcome. Fertil Steril. 2013;100(3):825–830.
Corbo RM, Ulizzi L, Piombo L, Martinez-Labarga C, De Stefano GF, Scacchi R. Estrogen receptor alpha polymorphisms and fertility in populations with different reproductive patterns. Mol Hum Reprod. 2007;13(8):537–540.
Kaya OH, Das A, Taylor RN, Bagchi IC, Bagchi MK. Roles of estrogen receptor-alpha and the coactivator MED1 during human endometrial decidualization. Mol Endocrinol. 2016;30(3):302–313.
Lubahn DB, Moyer JS, Golding TS, Couse JF, Korach KS, Smithies O. Alteration of reproductive function but not prenatal sexual development after insertional disruption of the mouse estrogen receptor gene. Proc Natl Acad Sci U S A. 1993;90(23):11162–11166.
Curtis HS, Goulding EH, Eddy EM, Korach KS. Studies using the estrogen receptor alpha knockout uterus demonstrate that implantation but not decidualization-associated signaling is estrogen dependent. Biol Reprod. 2002;67(4):1268–1277.
Lydon JP, DeMayo FJ, Funk CR, et al. Mice lacking progesterone receptor exhibit pleiotropic reproductive abnormalities. Genes Dev. 1995;9(18):2266–2278.
Franco HL, Jeong JW, Tsai SY, Lydon JP, DeMayo FJ. In vivo analysis of progesterone receptor action in the uterus during embryo implantation. Semin Cell Dev Biol. 2008;19(2):178–186.
Lim H, Ma L, Ma WG, Maas RL, Dey SK. Hoxa-10 regulates uterine stromal cell responsiveness to progesterone during implantation and decidualization in the mouse. Mol Endocrinol. 1999;13(6):1005–1017.
Benson GV, Lim H, Paria BC, Satokata I, Dey SK, Maas RL. Mechanisms of reduced fertility in Hoxa-10 mutant mice: uterine homeosis and loss of maternal Hoxa-10 expression. Development. 1996;122(9):2687–2696.
Lessey BA, Castelbaum AJ, Wolf L, et al. Use of integrins to date the endometrium. Fertil Steril. 2000;73(4):779–787.
Tei C, Maruyama T, Kuji N, Miyazaki T, Mikami M, Yoshimura Y. Reduced expression of alphavbeta3 integrin in the endometrium of unexplained infertility patients with recurrent IVF-ET failures: improvement by danazol treatment. J Assist Reprod Genet. 2003;20(1):13–20.
Chen D, Jin Z, Xing F. The expression of integrin beta 3 in cycling and early pregnant endometrium and its relationship with primary unexplained infertility [in Chinese]. Zhonghua Fu Chan Ke Za Zhi. 1998;33(8):487–489.
Boroujerdnia MG, Nikbakht R. Beta3 integrin expression within uterine endometrium and its relationship with unexplained infertility. Pak J Biol Sci. 2008;11(21):2495–2499.
McCabe MT, Brandes JC, Vertino PM. Cancer DNA methylation: molecular mechanisms and clinical implications. Clin Cancer Res. 2009;15(12):3927–3937.
Michaelson-Cohen R, Keshet I, Straussman R, Hecht M, Cedar H, Beller U. Genome-wide de novo methylation in epithelial ovarian cancer. Int J Gynecol Cancer. 2011;21(2):269–279.
Vlaykova T, Mitkova A, Stancheva G, et al. Microsatellite instability and promoter hypermethylation of MLH1 and MSH2 in patients with sporadic colorectal cancer. J BUON. 2011;16(2):265–273.
Shi J, Zhang G, Yao D, et al. Prognostic significance of aberrant gene methylation in gastric cancer. Am J Cancer Res. 2012;2(1):116–129.
Walters RJ, Williamson EJ, English DR, et al. Association between hypermethylation of DNA repetitive elements in white blood cell DNA and early-onset colorectal cancer. Epigenetics. 2013;8(7):748–755.
Kim JJ, Taylor HS, Lu Z, et al. Altered expression of HOXA10 in endometriosis: potential role in decidualization. Mol Hum Reprod. 2007;13(5):323–332.
Shin JE, Park SH, Jang YK. Epigenetic up-regulation of leukemia inhibitory factor (LIF) gene during the progression to breast cancer. Mol Cells. 2011;31(2):181–189.
Gao R, Ding Y, Liu X, et al. Effect of folate deficiency on promoter methylation and gene expression of Esrl, Cdhl and Pgr, and its influence on endometrial receptivity and embryo implantation. Hum Reprod. 2012;27(9):2756–2765.
Novak P, Jensen T, Oshiro MM, et al. Epigenetic inactivation of the HOXA gene cluster in breast cancer. Cancer Res. 2006;66(22):10664–10670.
Cheng W, Jiang Y, Liu C, Shen O, Tang W, Wang X. Identification of aberrant promoter hypomethylation of HOXA 10 in ovarian cancer. J Cancer Res Clin Oncol. 2010;136(8):1221–1227.
Rusiecki JA, Baccarelli A, Bollati V, Tarantini L, Moore LE. Bonefeld-Jorgensen EC. Global DNA hypomethylation is associated with high serum-persistent organic pollutants in Greenlandic Inuit. Environ Health Perspect. 2008;116(11):1547–1552.
Desaulniers D, Xiao GH, Lian H, et al. Effects of mixtures of polychlorinated biphenyls, methylmercury, and organochlorine pesticides on hepatic DNA methylation in prepubertal female Sprague-Dawley rats. Int J Toxicol. 2009;28(4):294–307.
Aluru N, Karchner SI, Hahn ME. Role of DNA methylation of AHR1 and AHR2 promoters in differential sensitivity to PCBs in Atlantic Killifish, Fundulus heteroclitus. Aquat Toxicol. 2011;101(1):288–294.
Lind L, Penell J, Luttropp K, et al. Global DNA hypermethylation is associated with high serum levels of persistent organic pollutants in an elderly population. Environ Int. 2013;59:456–461.
Colles A, Koppen G, Hanot V, et al. Fourth WHO-coordinated survey of human milk for persistent organic pollutants (POPs): Belgian results. Chemosphere. 2008;73(6):907–914.
Bloom MS, Fujimoto VY, Storm R, et al. Persistent organic pollutants (POPs) in human follicular fluid and in vitro fertilization outcomes, a pilot study. Reprod Toxicol. 2017;67:165–173.
Younglai EV, Foster WG, Hughes EG, Trim K, Jarrell JF. Levels of environmental contaminants in human follicular fluid, serum, and seminal plasma of couples undergoing in vitro fertilization. Arch Environ Contam Toxicol. 2002;43(1):121–126.
Lim HJ, Dey SK. HB-EGF: a unique mediator of embryo-uterine interactions during implantation. Exp Cell Res. 2009;315(4):619–626.
Zhang S, Lin H, Kong S, et al. Physiological and molecular determinants of embryo implantation. Mol Aspects Med. 2013;34(5):939–980.
Dey SK, Lim H, Das SK, et al. Molecular cues to implantation. Endocr Rev. 2004;25(3):341–373.
Wang H, Dey SK. Roadmap to embryo implantation: clues from mouse models. Nat Rev Genet. 2006;7(3):185–199.
Berger RG, Foster WG, DeCatanzaro D. Bisphenol-A exposure during the period of blastocyst implantation alters uterine morphology and perturbs measures of estrogen and progesterone receptor expression in mice. Reprod Toxicol. 2010;30(3):393–400.
Li R, Yu C, Gao R, et al. Effects of DEHP on endometrial receptivity and embryo implantation in pregnant mice. J Hazard Mater. 2012;241-242:231–240.
Lopata A, Bentin-Ley U, Enders A. “Pinopodes” and implantation. Rev Endocr Metab Disord. 2002;3(2):77–86.
Usadi RS, Murray MJ, Bagnell RC, et al. Temporal and morphologic characteristics of pinopod expression across the secretory phase of the endometrial cycle in normally cycling women with proven fertility. Fertil Steril. 2003;79(4):970–974.
Nikas G, Makrigiannakis A, Hovatta O, Jones HW Jr. Surface morphology of the human endometrium. Basic and clinical aspects. Ann N Y Acad Sci. 2000;900:316–324.
Kodaman PH, Taylor HS. Hormonal regulation of implantation. Obstet Gynecol Clin North Am. 2004;31(4):745–766.
Makrigiannakis A, Karamouti M, Petsas G, Makris N, Nikas G, Antsaklis A. The expression of receptivity markers in the fallopian tube epithelium. Histochem Cell Biol. 2009;132(2):159–167.
Jorgensen EM, Alderman MR, Taylor HS. Preferential epigenetic programming of estrogen response after in utero xenoestrogen (bisphenol-A) exposure. FASEB J. 2016;30(9):3194–3201.
Rashid NA, Lalitkumar S, Lalitkumar PG. Gemzell-Danielsson K. Endometrial receptivity and human embryo implantation. Am J Reprod Immunol. 2011;66(suppl 1):23–30.
Singh M, Chaudhry P, Asselin E. Bridging endometrial receptivity and implantation: network of hormones, cytokines, and growth factors. J Endocrinol. 2011;210(1):5–14.
Jobling S, Casey D, Rogers-Gray T, et al. Comparative responses of molluscs and fish to environmental estrogens and an estrogenic effluent. Aquat Toxicol. 2004;66(2):207–222.
Daston GP, Cook JC, Kavlock RJ. Uncertainties for endocrine disrupters: our view on progress. Toxicol Sci. 2003;74(2):245–252.
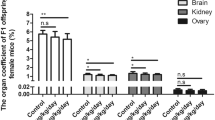
Pocar P, Fiandanese N, Secchi C, et al. Effects of polychlorinated biphenyls in CD-1 mice: reproductive toxicity and intergenera-tional transmission. Toxicol Sci. 2012;126(1):213–226.
Kulp JL, Mamillapalli R, Taylor HS. Aberrant HOXA10 methy-lation in patients with common gynecologic disorders: implications for reproductive outcomes. Reprod Sci. 2016;23(4):455–463.
Smith CC, Taylor HS. Xenoestrogen exposure imprints expression of genes (HoxalO) required for normal uterine development. FASEB J. 2007;21(1):239–246.
Du H, Taylor HS. The role of Hox genes in female reproductive tract development, adult function, and fertility. Cold Spring Harb Perspect Med. 2015;6(1):a023002.
Bromer JG, Wu J, Zhou Y, Taylor HS. Hypermethylation of homeobox A10 by in utero diethylstilbestrol exposure: an epige-netic mechanism for altered developmental programming. Endocrinology. 2009;150(7):3376–3382.
Bromer JG, Zhou Y, Taylor MB, Doherty L, Taylor HS. Bisphenol-A exposure in utero leads to epigenetic alterations in the developmental programming of uterine estrogen response. FASEB J. 2010;24(7):2273–2280.
Chen Y, Zhang J, Wang H, et al. miRNA-135a promotes breast cancer cell migration and invasion by targeting HOXA10. BMC Cancer. 2012;12:111.
Jackson JP, Lindroth AM, Cao X, Jacobsen SE. Control of CpNpG DNA methylation by the KRYPTONITE histone H3 methyltransferase. Nature. 2002;416(6880):556–560.
Zhu B, Zheng Y, Pham AD, et al. Monoubiquitination of human histone H2B: the factors involved and their roles in HOX gene regulation. Mol Cell. 2005;20(4):601–611.
von Grothusen C, Lalitkumar S, Rao BN. Gemzell-Danielsson K, Lalitkumar PG. Recent advances in understanding endometrial receptivity: molecular basis and clinical applications. Am J Reprod Immunol. 2014;72(2):148–157.
Petracco R, Grechukhina O, Popkhadze S, Massasa E, Zhou Y, Taylor HS. MicroRNA 135 regulates HOXA10 expression in endometriosis. J Clin Endocrinol Metab. 2011;96(12):E1925–E1933.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Qu, XL., Ming-Zhang, Yuan-Fang et al. Effect of 2,3′,4,4′,5-Pentachlorobiphenyl Exposure on Endometrial Receptivity and the Methylation of HOXA10. Reprod. Sci. 25, 256–268 (2018). https://doi.org/10.1177/1933719117711258
Published:
Issue Date:
DOI: https://doi.org/10.1177/1933719117711258