Abstract
Objective
To compare pregnancy outcome and placental pathology in pregnancies complicated by fetal growth restriction (FGR) with and without preeclampsia.
Methods
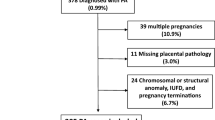
Labor, fetal/neonatal outcome, and placental pathology parameters from neonates with a birth weight below the10th percentile (FGR), born between 24 and 42 weeks of gestation, were reviewed. Results were compared between pregnancies complicated with preeclampsia (hypertensive FGR [H-FGR]) to those without preeclampsia (normotensive FGR [N-FGR]). Composite neonatal outcome, defined as 1 or more of early complication (respiratory distress, necrotizing enterocolitis, sepsis, transfusion, ventilation, seizure, hypoxic–ischemic encephalopathy, phototherapy, or death), Apgar score ≤7 at 5 minutes, and days of hospitalization, were compared between the groups. Placental lesions, classified as lesions related to maternal vascular supply, lesions consistent with fetal thrombo-occlusive disease and inflammatory lesions, maternal inflammatory response, and fetal inflammatory response, were also compared.
Results
Women in the H-FGR group (n = 72) were older, with higher body mass index (BMI) and higher rate of preterm labor (<34 weeks) than in the N-FGR group (n = 270), P < .001 for all. Composite neonatal outcome was worse in the H-FGR than in the N-FGR group, 50% versus 15.5%, P < .001. Higher rate of maternal placental vascular lesions was detected in H-FGR compared with N-FGR, 82% versus 57.7%, P < .001. Using a stepwise logistic regression model, maternal BMI (1.13 odds ratio [OR], confidence interval [CI] 1.035-1.227, P = .006) and neonatal birth weight (0.996 OR, CI 0.995-0.998, P < .001) were independently associated with worse neonatal outcome.
Conclusion
Worse neonatal outcome and more maternal placental vascular lesions in pregnancy complicated by FGR with preeclampsia versus FGR without preeclampsia suggest different pathophysiology in these entities.
Similar content being viewed by others
References
Baschat AA, Hecher K. Fetal growth restriction due to placental disease. Semin Perinatol. 2004;28(1):67–80.
Baschat AA. Pathophysiology of fetal growth restriction: implications for diagnosis and surveillance. Obstet Gynecol Surv. 2004; 59(8):617–627.
Breeze AC, Lees CC. Prediction and perinatal outcomes of fetal growth restriction. Semin Fetal Neonatal Med. 2007;12(5): 383–397.
Srinivas SK, Edlow AG, Neff PM, Sammel MD, Andrela CM, Elovitz MA. Rethinking IUGR in preeclampsia: dependent or independent of maternal hypertension? J Perinatol. 2009;29(10):680–684.
Witlin AG, Saade GR, Mattar F, Sibai BM. Predictors of neonatal outcome in women with severe preeclampsia or eclampsia between 24 and 33 weeks’ gestation. Am J Obstet Gynecol. 2000;182(3):607–611.
Chammas MF, Nguyen TM, Li MA, Nuwayhid BS, Castro LC. Expectant management of severe preterm preeclampsia: is intrauterine growth restriction an indication for immediate delivery? Am J Obstet Gynecol. 2000;183(4):853–858.
Shear RM, Rinfret D, Leduc L. Should we offer expectant management in cases of severe preterm preeclampsia with fetal growth restriction? Am J Obstet Gynecol. 2005;192(4):1119–125.
Haddad B, Kayem G, Deis S, Sibai BM. Are perinatal and maternal outcomes different during expectant management of severe preeclampsia in the presence of intrauterine growth restriction? Am J Obstet Gynecol. 2007;196(3):237.e1–e5.
Mitani M, Matsuda Y, Makino Y, Akizawa Y, Ohta H. Clinical features of fetal growth restriction complicated later by preeclampsia. J Obstet Gynaecol Res. 2009;35(5):882–887.
Zhou Q, Ren Y, Yan Y, Chu C, Gui Y, Li X. Fetal tissue Doppler imaging in pregnancies complicated with preeclampsia with or without intrauterine growth restriction. Prenat Diagn. 2012; 32(11):1021–1028.
Piper JM, Langer O, Xenakis EM, McFarland M, Elliott BD, Berkus MD. Perinatal outcome in growth-restricted fetuses: do hypertensive and normotensive pregnancies differ? Obstet Gynecol. 1996;88(2):194–199.
Parlakgumus HA, Iskender C, Aytac PC, Tarim E. Do intrauterine growth restricted fetuses of the hypertensive and normotensive mothers differ from each other?. Arch Gynecol Obstet. 2012;286(5):1147–1151.
McCowan LM, Roberts CT, Dekker GA, et al. Risk factors for small-for-gestational-age infants by customised birthweight centiles: data from an international prospective cohort study. BJOG. 2010; 117(13):1599–607.
Norwitz ER. Defective implantation and placentation: laying the blueprint for pregnancy complications. Reprod Biomed Online. 2007;14(spec no 1):101–109.
Sibai B, Dekker G, Kupferminc M. Pre-eclampsia. Lancet. 2005; 365(9461):785–799.
Redline RW. Placental pathology: a systematic approach with clinical correlations. Placenta. 2008;29(suppl A):S86–S91.
Vinnars MT, Nasiell J, Holmstrom G, Norman M, Westgren M, Papadogiannakis N. Association between placental pathology and neonatal outcome in preeclampsia: a large cohort study. Hypertens Pregnancy. 2013;33(2):145–158.
Vinnars MT, Wijnaendts LC, Westgren M, Bolte AC, Papadogiannakis N, Nasiell J. Severe preeclampsia with and without HELLP differ with regard to placental pathology. Hypertension. 2008;51(5):1295–1299.
Sebire NJ, Goldin RD, Regan L. Term preeclampsia is associated with minimal histopathological placental features regardless of clinical severity. J Obstet Gynaecol. 2005;25(2):117–118.
Kovo M, Schreiber L, Ben-Haroush A, Wand S, Golan A, Bar J. Placental vascular lesion differences in pregnancy-induced hypertension and normotensive fetal growth restriction. Am J Obstet Gynecol. 2010;202(6):561.e1–e5.
Ogge G, Chaiworapongsa T, Romero R, et al. Placental lesions associated with maternal underperfusion are more frequent in early-onset than in late-onset preeclampsia. J Perinat Med. 2011;39(6):641–652.
Salafia CM, Ernst LM, Pezzullo JC, Wolf EJ, Rosenkrantz TS, Vintzileos AM. The very low birthweight infant: maternal complications leading to preterm birth, placental lesions, and intrauterine growth. Am J Perinatol. 1995;12(2):106–110.
Salafia CM, Charles AK, Maas EM. Placenta and fetal growth restriction. Clin Obstet Gynecol. 2006;49(2):236–256.
Vedmedovska N, Rezeberga D, Teibe U, Melderis I, Donders GG. Placental pathology in fetal growth restriction. Eur J Obstet Gynecol Reprod Biol. 2011;155(1):36–40.
Dicke JM, Huettner P, Yan S, Odibo A, Kraus FT. Umbilical artery Doppler indices in small for gestational age fetuses: correlation with adverse outcomes and placental abnormalities. J Ultrasound Med. 2009;28(12):1603–1610.
Fok RY, Pavlova Z, Benirschke K, Paul RH, Platt LD. The correlation of arterial lesions with umbilical artery Doppler velocimetry in the placentas of small-for-dates pregnancies. Obstet Gynecol. 1990;75(4):578–583.
Villar J, Carroli G, Wojdyla D, et al. Preeclampsia, gestational hypertension and intrauterine growth restriction, related or independent conditions? Am J Obstet Gynecol. 2006;194(4):921–931.
Dollberg S, Haklai Z, Mimouni FB, Gorfein I, Gordon ES. Birth weight standards in the live-born population in Israel. Isr Med Assoc J. 2005;7(5):311–314.
ACOG practice bulletin. Diagnosis and management of preeclampsia and eclamps. Number 33, January 2002. American college of obstetricians and gynecologists. Int J Gynaecol Obstet. 2002;77(1):67–75.
Kovo M, Schreiber L, Ben-Haroush A, Gold E, Golan A, Bar J. The placental component in early-onset and late-onset preeclampsia in relation to fetal growth restriction. Prenat Diagn. 2012; 32(7):632–637.
Kovo M, Schreiber L, Ben-Haroush A, et al. The placental factor in early- and late-onset normotensive fetal growth restriction. Placenta. 2013;34(4):320–324.
Redline RW, Heller D, Keating S, Kingdom J. Placental diagnostic criteria and clinical correlation—a workshop report. Placenta. 2005;26(suppl A):S114–S117.
Morsing E, Marsal K. Pre-eclampsia—an additional risk factor for cognitive impairment at school age after intrauterine growth restriction and very preterm birth. Early Hum Dev. 2014;90(2):99–101.
Salafia CM, Pezzullo JC, Lopez-Zeno JA, Simmens S, Minior VK, Vintzileos AM. Placental pathologic features of preterm preeclampsia. Am J Obstet Gynecol. 1995;173(4):1097–1105.
Roberts JM, Escudero C. The placenta in preeclampsia. Pregnancy Hypertens. 2012;2(2):72–83.
Huppertz B. Placental origins of preeclampsia: challenging the current hypothesis. Hypertension. 2008;51(4):970–975.
Spinillo A, Gardella B, Bariselli S, Alfei A, Silini E, Dal Bello B. Placental histopathological correlates of umbilical artery Doppler velocimetry in pregnancies complicated by fetal growth restriction. Prenat Diagn. 2012;32(13):1263–1272.
Redline RW, Ariel I, Baergen RN, et al. Fetal vascular obstructive lesions: nosology and reproducibility of placental reaction patterns. Pediatr Dev Pathol. 2004;7(5):443–452.
Sander CH, Kinnane L, Stevens NG. Hemorrhagic endovasculitis of the placenta: a clinicopathologic entity associated with adverse pregnancy outcome. Compr Ther. 1985;11(5):66–74.
Redline RW. Severe fetal placental vascular lesions in term infants with neurologic impairment. Am J Obstet Gynecol. 2005;192(2):452–457.
Parra-Saavedra M, Crovetto F, Triunfo S, et al. Neurodevelopmental outcomes of near-term small-for-gestational-age infants with and without signs of placental underperfusion. Placenta. 2014;35(4):269–274.
Illa M, Coloma JL, Eixarch E, et al. Growth deficit in term small-for-gestational fetuses with normal umbilical artery Doppler is associated with adverse outcome. J Perinat Med. 2009;37(1): 48–52.
Parra-Saavedra M, Crovetto F, Triunfo S, et al. Placental findings in late-onset SGA births without Doppler signs of placental insufficiency. Placenta. 2013;34(12):1136–1141.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kovo, M., Schreiber, L., Elyashiv, O. et al. Pregnancy Outcome and Placental Findings in Pregnancies Complicated by Fetal Growth Restriction With and Without Preeclampsia. Reprod. Sci. 22, 316–321 (2015). https://doi.org/10.1177/1933719114542024
Published:
Issue Date:
DOI: https://doi.org/10.1177/1933719114542024