Abstract
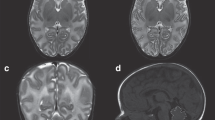
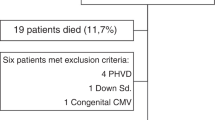
Intrauterine growth restriction (IUGR) is associated with increased risk of perinatal morbidity and mortality, as well as long-term neurological deficits. However, neurostructural correlations with observed developmental disabilities have not yet been established. Magnetic resonance imaging (MRI) could prove useful for assessing brain development in the early neonatal period. We evaluated cerebral lesions and morphological maturation by MRIs in 59 preterm neonates, in order to verify the hypothesis that IUGR interferes on human brain development. A total of 26 pregnancies were complicated by IUGR and 33 pregnancies delivered preterm at a comparable gestational age with appropriate for gestational age (AGA). Magnetic resonance examination was performed at the completion of 41 weeks’ gestation. White matter disease studied with MR included periventricular cavitations and punctuate lesions characterized by increased signal on T1-weighted and decreased signal on T2-weighted images. Cerebral maturation was defined by the total maturation score, on the basis of 4 morphological parameters of cerebral maturation: myelination (M), cortical infolding (C), germinal matrix distribution (GM), and glial cell migration pattern (G). No difference in brain lesions and in the level of cerebral maturation was found between preterm AGA and IUGR neonates. However, myelination was significantly reduced in IUGR neonates with brain sparing compared to IUGR neonates with normal Doppler of middle cerebral artery. Our study could not demonstrate any major significant difference between preterm AGA and IUGR neonates in terms of lesion occurrence and cerebral maturation. We observed, however, a mild delay in myelination in IUGR with brain sparing in utero. The relevance of this finding needs to be investigated with long-term follow-up.
Similar content being viewed by others
References
Sibley CP, Turner MA, Cetin I, et al. Placental phenotypes of intrauterine growth. Pediatr Res. 2005;58(5):827–832. Review.
Pardi G, Marconi AM, Cetin I. Placental-fetal interrelationship in IUGR fetuses-a review. Placenta. 2002;23(suppl A):S136–S141. Review.
Cetin I, Alvino G. Intrauterine growth restriction: implications for placental metabolism and transport. Placenta. 2009;30(suppl A):S77–S82. Review.
Baschat AA, Cosmi E, Bilardo CM, et al. Predictors of neonatal outcome in early-onset placental dysfunction. Obstet Gynecol. 2007 Feb;109(2 Pt 1):253–61.
Garite TJ, Clark R, Thorp JA. Intrauterine growth restriction increases morbidity and mortality among premature neonates. Am J Obstet Gynecol. 2004;191(2):481–487.
Bernstein IM, Horbar JD, Badger GJ, Ohlsson A, Golan A. Morbidity and mortality among very-low-birth-weight neonates with intrauterine growth restriction. The Vermont Oxford Network. Am J Obstet Gynecol. 2000;182(1 pt 1):198–206.
Leitner Y, Fattal-Valevski A, Geva R, et al. Neurodevelopmental outcome of children with intrauterine growth retardation: a longitudinal, 10-year prospective study. J Child Neurol. 2007;22(5):580–587.
Kok JH, den Ouden AL, Verloove-Vanhorick SP, Brand R. Outcome of very preterm small for gestational age infants: the first nine years of life. Br J Obstet Gynaecol. 1998;105(2):162–168.
Walker DM, Marlow N. Neurocognitive outcome following fetal growth restriction. Arch Dis Child Fetal Neonatal Ed 2008;93(4):F322–F325.
Geva R, Eshel R, Leitner Y, Valevski AF, Harel S. Neuropsychological outcome of children with intrauterine growth restriction: a 9-year prospective study. Pediatrics. 2006;118(1):91–100.
Pardi G, Cetin I, Marconi AM, et al. Diagnostic value of blood sampling in fetuses with growth retardation. N Engl J Med. 1993;328(10):692–696.
Figueras F, Eixarch E, Meler E, et al. Small-for-gestational-age fetuses with normal umbilical artery Doppler have suboptimal perinatal and neurodevelopmental outcome. Eur J Obstet Gynecol Reprod Biol. 2008;136(1):34–38.
Arthur R. Magnetic resonance imaging in preterm infants. Pediatr Radiol. 2006 Jul;36(7):593–607. Review.
Tolsa CB, Zimine S, Warfield SK, et al. Early alteration of structural and functional brain development in premature infants born with intrauterine growth restriction. Pediatr Res. 2004;56(1):132–138.
Lodygensky GA, Seghier ML, Warfield SK, et al. Intrauterine growth restriction affects the preterm infant’s hippocampus. Pediatr Res 2008;63(4):438–443.
Childs AM, Ramenghi LA, Cornette L, et al. Cerebral maturation in premature infants: quantitative assessment using MR imaging. AJNR Am J Neuroradiol. 2001;22(8):1577–1582.
Woodward LJ, Anderson PJ, Austin NC, Howard K, Inder TE. Neonatal MRI to predict neurodevelopmental outcomes in preterm infants. N Engl J Med. 2006;355(7):685–694.
Ramenghi LA, Fumagalli M, Righini A, et al. Magnetic resonance imaging assessment of brain maturation in preterm neonates with punctate white matter lesions. Neuroradiology. 2007;49(2):161–167.
Todros T, Ferrazzi E, Groli C, et al. Fitting growth curves to head and abdomen measurements of the fetus: a multicentric study. J Clin Ultrasound. 1987;15(2):95–105.
Parazzini F, Cortinovis I, Bortolus R, Fedele L. Standards of birth weight in Italy. Ann Ostet Ginecol Med Perinat. 1991;112(4):203–246. Italian.
Childs AM, Cornette L, Ramenghi LA, et al. Magnetic resonance and cranial ultrasound characteristics of periventricular white matter abnormalities in newborn infants. Clin Radiol. 2001;56(8):647–655.
Dyet LE, Kennea N, Counsell SJ, et al. Natural history of brain lesions in extremely preterm infants studied with serial magnetic resonance imaging from birth and neurodevelopmental assessment. Pediatrics. 2006;118(2):536–548.
Thompson DK, Warfield SK, Carlin JB, et al. Perinatal risk factors altering regional brain structure in the preterm infant. Brain. 2007;130(pt 3):667–677.
Scherjon S, Briet J, Oosting H, Kok J. The discrepancy between maturation of visual-evoked potentials and cognitive outcome at five years in very preterm infants with and without hemodynamic sign of fetal brain sparing. Pediatrics. 2000;105(2):385–391.
Cruz-Martinez R, Figueras F, Oros D, et al. Cerebral blood perfusion and neurobehavioral performance in full-term small-for-gestational-age fetuses. Am J Obstet Gynecol. 2009;201(5):474.e1–474.e7.
Eixarch E, Meler E, Iraola A, et al. Neurodevelopmental outcome in 2-years-old infants who were small-for-gestational age term fetus with cerebral blood flow redistribution. Ultrasound Obstet Gynecol. 2008;32(7):849–889.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Ramenghi, L.A., Martinelli, A., De Carli, A. et al. Cerebral Maturation in IUGR and Appropriate for Gestational Age Preterm Babies. Reprod. Sci. 18, 469–475 (2011). https://doi.org/10.1177/1933719110388847
Published:
Issue Date:
DOI: https://doi.org/10.1177/1933719110388847