Abstract
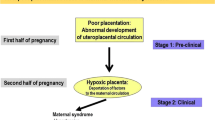
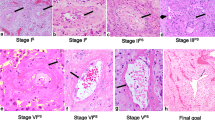
During pregnancy, trophoblasts invade and transform the maternal spiral arteries that supply blood to the placenta. Recent work has revealed that this process occurs in several stages, and details of the molecular and cellular mechanisms are beginning to emerge, including changes that precede or accompany trophoblastic colonization of the vascular media. Disruption and eventual loss of smooth muscle cells and their associated extracellular matrix are central to physiological transformation. Advances in understanding will lead to the identification of the causative factors involved in failure of remodeling in pathological pregnancies and suggest novel diagnostic and therapeutic avenues.
Similar content being viewed by others
References
Craven CM, Morgan T., Ward K. Decidual spiral artery remodelling begins before cellular interaction with cytotrophoblasts. Placenta. 1998;19(4):241–252.
Aplin JD Implantation, trophoblast differentiation and haemochorial placentation: mechanistic evidence in vivo and in vitro. J Cell Sci. 1991;99(pt 4):681–692.
Pijnenborg R., Vercruysse L., Hanssens M. The uterine spiral arteries in human pregnancy: facts and controversies. Placenta. 2006;27(9–10):939–958.
Ball E., Bulmer JN, Ayis S, et al. Late sporadic miscarriage is associated with abnormalities in spiral artery transformation and trophoblast invasion. J Pathol. 2006;208(4):535–542.
Kim YM, Bujold E., Chaiworapongsa T, et al. Failure of physiologic transformation of the spiral arteries in patients with preterm labor and intact membranes. Am J Obstet Gynecol. 2003;189(4):1063–1069.
Allt G., Lawrenson JG Pericytes: cell biology and pathology. Cells Tissues Organs. 2001;169(1):1–11.
Alimohamad H., Habijanac T., Larjava H, et al. Colocalization of the collagen-binding proteoglycans decorin, biglycan, fibromodulin and lumican with different cells in human gingiva. J Periodontal Res. 2005;40(1):73–86.
Canfield AE, Allen TD, Grant ME, et al. Modulation of extracellular matrix biosynthesis by bovine retinal pericytes in vitro: effects of the substratum and cell density. J Cell Sci. 1990;96(pt 1):159–169.
Schor AM, Canfield AE, Sutton AB, et al. Pericyte differentiation. Clin Orthop Relat Res. 1995;(313):81–91.
Myllyharju J., Kivirikko KI Collagens, modifying enzymes and their mutations in humans, flies and worms. Trends Genet. 2004;20(1):33–43.
Shekhonin BV, Domogatsky SP, Muzykantov VR, et al. Distribution of type I, III, IV and V collagen in normal and atherosclerotic human arterial wall: immunomorphological characteristics. Coll Relat Res. 1985;5(4):355–368.
Jacob MP Extracellular matrix remodeling and matrix metalloproteinases in the vascular wall during aging and in pathological conditions. Biomed Pharmacother. 2003;57(5–6): 195–202.
Zanetti M., Braghetta P., Sabatelli P, et al. EMILIN-1 deficiency induces elastogenesis and vascular cell defects. Mol Cell Biol. 2004;24(2):638–650.
Spessotto P., Bulla R., Danussi C, et al. EMILIN1 represents a major stromal element determining human trophoblast invasion of the uterine wall. J Cell Sci. 2006;119(pt 21): 4574–4584.
Heissig B., Hattori K., Friedrich M, et al. Angiogenesis: vascular remodeling of the extracellular matrix involves metalloproteinases. Curr Opin Hematol. 2003;10(2):136–141.
Pepper MS Role of the matrix metalloproteinase and plasminogen activator-plasmin systems in angiogenesis. Arterioscler Thromb Vasc Biol. 2001;21(7):1104–1117.
Mott JD, Werb Z. Regulation of matrix biology by matrix metalloproteinases. Curr Opin Cell Biol. 2004;16(5):558–564.
Davis GE, Bayless KJ, Mavila A. Molecular basis of endothelial cell morphogenesis in three-dimensional extracellular matrices. Anat Rec. 2002;268(3):252–275.
McGuire JK, Li Q., Parks WC Matrilysin (matrix metalloproteinase-7) mediates E-cadherin ectodomain shedding in injured lung epithelium. Am J Pathol. 2003; 162(6):1831–1843.
Covington MD, Bayless KJ, Burghardt RC, et al. Ischemia-induced cleavage of cadherins in NRK cells: evidence for a role of metalloproteinases. Am J Physiol Renal Physiol. 2005; 289(2):F280–F288.
Ham C., Levkau B., Raines EW, et al. ADAM15 is an adherens junction molecule whose surface expression can be driven by VE-cadherin. Exp Cell Res. 2002;279(2):239–247.
Horiuchi K., Weskamp G., Lum L, et al. Potential role for ADAM15 in pathological neovascularization in mice. Mol Cell Biol. 2003;23(16):5614–5624.
Bazzoni G., Dejana E. Endothelial cell-to-cell junctions: molecular organization and role in vascular homeostasis. Physiol Rev. 2004;84(3):869–901.
Dejana E. Endothelial cell-cell junctions: happy together. Nat Rev Mol Cell Biol. 2004;5(4):261–270.
Nawrocki B., Polette M., Marchand V, et al. Membrane-type matrix metalloproteinase-1 expression at the site of human placentation. Placenta. 1996;17(8):565–572.
Vegh GL, Selcuk Tuncer Z, Fulop V, et al. Matrix metalloproteinases and their inhibitors in gestational trophoblastic diseases and normal placenta. Gynecol Oncol. 1999;75(2):248–253.
Lash GE, Otun HA, Innes BA, et al. Interferon-gamma inhibits extravillous trophoblast cell invasion by a mechanism that involves both changes in apoptosis and protease levels. FASEB J. 2006;20(14):2512–2518.
Librach CL, Feigenbaum SL, Bass KE, et al. Interleukin-1 beta regulates human cytotrophoblast metalloproteinase activity and invasion in vitro. J Biol Chem. 1994;269(25):17125–17131.
Librach CL, Werb Z., Fitzgerald ML, et al. 92-kD type IV collagenase mediates invasion of human cytotrophoblasts. J Cell Biol. 1991;113(2):437–449.
Levy BI, Benessiano J., Poitevin P, et al. Endothelium-dependent mechanical properties of the carotid artery in WKY and SHR: role of angiotensin converting enzyme inhibition. Circ Res. 1990;66(2):321–328.
Safar M., Chamiot-Clerc P., Dagher G, et al. Pulse pressure, endothelium function, and arterial stiffness in spontaneously hypertensive rats. Hypertension. 2001;38(6):1416–1421.
Yamamoto K., Yamamoto M., Yamamoto N, et al. Regulation of differentiated properties of vascular smooth muscle cells in atherosclerosis: role of extracellular matrix. Connect Tissue. 2002;34:317–325.
Harris LK, Keogh RJ, Wareing M, et al. Invasive trophoblasts stimulate vascular smooth muscle cell apoptosis by a fas ligand-dependent mechanism. Am J Pathol. 2006;169(5):1863–1874.
Keogh RJ, Harris LK, Freeman A, et al. Fetal-derived trophoblast utilize the apoptotic cytokine TNF-related apoptosis-inducing ligand (TRAIL) to induce smooth muscle cell death. Circ Res. 2007;100(6):834–841.
Nichols WW Clinical measurement of arterial stiffness obtained from noninvasive pressure waveforms. Am J Hypertens. 2005;18(1 pt 2):3S–10S.
Houghton AM, Quintero PA, Perkins DL, et al. Elastin fragments drive disease progression in a murine model of emphysema. J Clin Invest. 2006;116(3):753–759.
Hinek A. Nature and the multiple functions of the 67-kD elastin-/laminin binding protein. Cell Adhes Commun. 1994; 2(3):185–193.
Mochizuki S., Brassart B., Hinek A. Signaling pathways transduced through the elastin receptor facilitate proliferation of arterial smooth muscle cells. J Biol Chem. 2002;277(47): 44854–44863.
Varga Z., Jacob MP, Csongor J, et al. Altered phosphatidylinositol breakdown after K-elastin stimulation in PMNLs of elderly. Mech Ageing Dev. 1990; 52(1):61–70.
Faury G. Role of the elastin-laminin receptor in the cardiovascular system. Pathol Biol (Paris). 1998;46(7):517–526.
Faury G., Ristori MT, Verdetti J., et al. Effect of elastin peptides on vascular tone. J Vasc Res. 1995;32(2):112–119.
Hinek A., Molossi S., Rabinovitch M. Functional interplay between interleukin-1 receptor and elastin binding protein regulates fibronectin production in coronary artery smooth muscle cells. Exp Cell Res. 1996;225(1):122–131.
Ntayi C., Labrousse AL, Debret R, et al. Elastin-derived peptides upregulate matrix metalloproteinase-2-mediated melanoma cell invasion through elastin-binding protein. J Invest Dermatol. 2004;122(2):256–265.
Brassart B., Randoux A., Hornebeck W, et al. Regulation of matrix metalloproteinase-2 (gelatinase A, MMP-2), membrane-type matrix metalloproteinase-1 (MT1-MMP) and tissue inhibitor of metalloproteinases-2 (TIMP-2) expression by elastin-derived peptides in human HT-1080 fibrosarcoma cell line. Clin Exp Metastasis. 1998;16(6):489–500.
Hornebeck W., Derouette JC, Brechemier D, et al. Elastogenesis and elastinolytic activity in human breast cancer. Biomedicine. 1977;26(1):48–52.
Host NB, Hansen SS, Jensen LT, et al. Thrombolytic therapy of acute myocardial infarction alters collagen metabolism. Cardiology. 1994;85(5):323–333.
Jensen LT, Horslev-Petersen K., Toft P, et al. Serum aminoterminal type III procollagen peptide reflects repair after acute myocardial infarction. Circulation. 1990;81(1):52–57.
Peuhkurinen KJ, Risteli L., Melkko JT, et al. Thrombolytic therapy with streptokinase stimulates collagen breakdown. Circulation. 1991;83(6):1969–1975.
Poulsen SH, Host NB, Egstrup K. Long-term changes in collagen formation expressed by serum carboxyterminal propeptide of type-I procollagen and relation to left ventricular function after acute myocardial infarction. Cardiology. 2001;96(1):45–50.
Sund M., Xie L., Kalluri R. The contribution of vascular basement membranes and extracellular matrix to the mechanics of tumor angiogenesis. Apmis. 2004;112(7–8):450–462.
Shapiro SD Matrix metalloproteinase degradation of extracellular matrix: biological consequences. Curr Opin Cell Biol. 1998;10(5):602–608.
Ashworth JL, Murphy G., Rock MJ, et al. Fibrillin degradation by matrix metalloproteinases: implications for connective tissue remodelling. Biochem J. 1999;340 (pt 1):171–181.
Kielty CM, Woolley DE, Whittaker SP, et al. Catabolism of intact fibrillin microfibrils by neutrophil elastase, chymotrypsin and trypsin. FEBS Lett. 1994;351(1):85–89.
Rabinovitch M. EVE and beyond, retro and prospective insights. Am J Physiol. 1999;277(1 pt 1):L5–L12.
Cowan KN, Leung WC, Mar C, et al. Caspases from apoptotic myocytes degrade extracellular matrix: a novel remodeling paradigm. FASEB J. 2005; 19(13):1848–1850.
Chapman HA, Riese RJ, Shi GP Emerging roles for cysteine proteases in human biology. Annu Rev Physiol. 1997;59:63–88.
Hornebeck W., Brechemier D., Bourdillon MC, et al. Isolation and partial characterization of an elastase-like protease from rat aorta smooth muscle cells: possible role in the regulation of elastin biosynthesis. Connect Tissue Res. 1981;8(3–4):245–249.
Campbell EJ, Wald MS Hypoxic injury to human alveolar macrophages accelerates release of previously bound neutrophil elastase: implications for lung connective tissue injury including pulmonary emphysema. Am Rev Respir Dis. 1983; 127(5):631–635.
Werb Z., Banda MJ, Jones PA Degradation of connective tissue matrices by macrophages. I. Proteolysis of elastin, glycoproteins, and collagen by proteinases isolated from macrophages. J Exp Med. 1980;152(5):1340–1357.
Legrand Y., Pignaud G., Caen JP, et al. Separation of human blood platelet elastase and proelastase by affinity chromatography. Biochem Biophys Res Commun. 1975;63(1):224–231.
Yamada E., Hazama F., Kataoka H, et al. Elastase-like enzyme in the aorta of spontaneously hypertensive rats. Virchows Arch B Cell Pathol Incl Mol Pathol. 1983;44(2):241–245.
Staun-Ram E., Goldman S., Gabarin D, et al. Expression and importance of matrix metalloproteinase 2 and 9 (MMP-2 and -9) in human trophoblast invasion. Reprod BiolEndocrinol. 2004; 2:59–71.
Nakanishi T., Ozaki Y., Blomgren K, et al. Role of cathepsins and cystatins in patients with recurrent miscarriage. Mol Hum Reprod. 2005;11(5):351–355.
Shipley JM, Doyle GA, Fliszar CJ, et al. The structural basis for the elastolytic activity of the 92-kDa and 72-kDa gelatinases: role of the fibronectin type II-like repeats. J Biol Chem. 1996;271(8):4335–4341.
Sukhova GK, Shi GP, Simon DI, et al. Expression of the elastolytic cathepsins S and K in human atheroma and regulation of their production in smooth muscle cells. J Clin Invest. 1998;102(3):576–583.
Uzui H., Harpf A., Liu M, et al. Increased expression of membrane type 3-matrix metalloproteinase in human atherosclerotic plaque: role of activated macrophages and inflammatory cytokines. Circulation. 2002;106(24):3024–3030.
Dollery CM, Owen CA, Sukhova GK, et al. Neutrophil elastase in human atherosclerotic plaques: production by macrophages. Circulation. 2003;107(22):2829–2836.
Reister F., Frank HG, Heyl W, et al. The distribution of macrophages in spiral arteries of the placental bed in preeclampsia differs from that in healthy patients. Placenta. 1999; 20(2–3):229–233.
Ashkar AA, Di Santo JP, Croy BA. Interferon gamma contributes to initiation of uterine vascular modification, decidual integrity, and uterine natural killer cell maturation during normal murine pregnancy. J Exp Med. 2000;192(2):259–270.
Esadeg S., He H., Pijnenborg R, et al. Alpha-2 macroglobulin controls trophoblast positioning in mouse implantation sites. Placenta. 2003;24(10):912–921.
Tchougounova E., Forsberg E., Angelborg G, et al. Altered processing of fibronectin in mice lacking heparin: a role for heparin-dependent mast cell chymase in fibronectin degradation. J Biol Chem. 2001; 276(6):3772–3777.
Kofford MW, Schwartz LB, Schechter NM, et al. Cleavage of type I procollagen by human mast cell chymase initiates collagen fibril formation and generates a unique carboxyl-terminal propeptide. J Biol Chem. 1997;272(11):7127–7131.
Szewczyk G., Szewczyk A., Pyzlak M, et al. Mast cells, histamine and development of the placental vascular network in pregnancies complicated by preeclampsia and intrauterine growth retardation [in Polish]. Ginekol Pol. 2005;76(9):727–734.
Noack F., Kruger S., Thorns C, et al. Application of novel tissue microarrays to investigate expression of tryptase, chymase and KIT protein in placental mast cells. Arch Gynecol Obstet. 2005;272(3):223–228.
Mitani R., Maeda K., Fukui R, et al. Production of human mast cell chymase in human myometrium and placenta in cases of normal pregnancy and preeclampsia. Eur J Obstet Gynecol Reprod Biol. 2002;101(2):155–160.
Shapiro RL, Duquette JG, Roses DF, et al. Induction of primary cutaneous melanocytic neoplasms in urokinase-type plasminogen activator (uPA)-deficient and wild-type mice: cellular blue nevi invade but do not progress to malignant melanoma in uPA-deficient animals. Cancer Res. 1996;56(15):3597–3604.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Harris, L.K., Aplin, J.D. Vascular Remodeling and Extracellular Matrix Breakdown in the Uterine Spiral Arteries During Pregnancy. Reprod. Sci. 14 (Suppl 8), 28–34 (2007). https://doi.org/10.1177/1933719107309588
Published:
Issue Date:
DOI: https://doi.org/10.1177/1933719107309588