Abstract
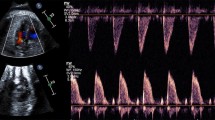
The authors show that pulse transit time and blood pressure are reciprocal in fetal goat models. They applied this technique in clinical settings to correlate changes in pulse transit time with fetal heart rate monitoring patterns and acid-base status. In 18 uncomplicated pregnancies, pulse transit time was obtained from electrocardiograms to pulse oximeter waveform and averaged during each baseline period, defined by the interpretation of fetal heart rate monitoring. According to a > 10% change from the control value, chronological changes were categorized into shortened, unchanged, and prolonged. Pulse transit time was available in 82% ± 11% of the recordings. In 15 fetuses, 2 (13%) showed prolonged, 7 (47%) showed shortened, and 6 (40%) showed unchanged conditions. Comparisons of the shortened and unchanged categories revealed that severe variable deceleration was significantly increased, and half or more fetuses showed hypoxemia in the shortened category. Shortening of pulse transit time, theoretically indicating a hypertensive condition, was more frequently associated with severe variable decelerations, suggesting that the pulse transit time may supplement the interpretation of fetal heart rate monitoring.
Similar content being viewed by others
References
Ikeda T, Murata Y, Quilligan EJ, et al. Physiologic and histologic changes in near-term fetal lambs exposed to asphyxia by partial cord occlusion. Am J Obstet Gynecol. 1998;178:24–32.
Ota A, Ikeda T, Ikenoue T, Toshimori K. Sequence of neuronal responses assessed by immunohistochemistry in the newborn rat brain after hypoxia-ischemia. Am J Obstet Gynecol. 1997; 177:519–526.
Sameshima H, Kawagoe Y, Ikenoue T, Sakamoto H. Continuous systolic blood pressure monitoring by the difference in electrocardiogram and pulse oximetry in near-term, exteriorized goat fetuses.J Soc Gynecol Investig. 2003;10:200–204.
Heard SO, Lisbon A, Toth I, Ramasubramanian R. An evaluation of a new continuous blood pressure monitoring system in critically ill patients. J Clin Anesth. 2000;12:509–518.
Awad AA, Ghobashy MAM, Stout RG, Silberman DG, Shelley KH. How does the plethysmogram derived from the pulse oximeter relate to arterial blood pressure in coronary artery bypass graft patients? Anesth Analg. 2001;93:1466–1471.
National Institute of Child Health and Human Development Research Planning Workshop. Electronic fetal heart rate monitoring: research guidelines for interpretation. Am J Obstet Gynecol. 1997;177:1385–1390.
Vogl SE, Worda C, Egarter C, et al. Mode of delivery is associated with maternal and fetal endocrine stress response. BJOG. 2006;113:441–445.
Gribbin B, Steptoe A, Sleight P. Pulse wave velocity as a measure of blood pressure change. Psychophysiology. 1976; 13:86–90.
Asmar R, Benetos A, Topouchian J, et al. Assessment of arterial distensibility by automatic pulse wave velocity measurement: validation and clinical application studies. Hypertension. 1995; 26:485–490.
Avolio AP, Deng FQ, Li DQ, et al. Effects of aging on arterial distensibility in populations with high and low prevalence of hypertension: comparison between urban and rural communities in China. Circulation. 1985;71:202–210.
Malcus P, Kjellmer I, Lingman G, Marsal K, Thiringer K, Rosen KG. Diameters of the common carotid artery and aorta change in different directions during acute asphyxia in the fetal lamb. J Perinat Med. 1991;19:259–267.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study is supported in part by grant 17591749 (to YK) and grant 18591805 (to HS) from Grant-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science, and Technology, Japan. We are grateful to ATOM Medical Corporation for its help in analyzing the pulse transit time.
Rights and permissions
About this article
Cite this article
Kawagoe, Y., Sameshima, H. & Ikenoue, T. Clinical Application of Pulse Transit Time and Correlation With Intrapartum Fetal Heart Rate Monitoring: A Preliminary Study of 18 Full-Term Infants. Reprod. Sci. 15, 567–571 (2008). https://doi.org/10.1177/1933719107308144
Published:
Issue Date:
DOI: https://doi.org/10.1177/1933719107308144