Abstract
Objective
The study was undertaken to quantify the psychologic and physiologic responses to the stresses of an obstetrics/gynecology residency program.
Methods
Six male residents were studied on four occasions: one day during the first 2 weeks of their residency, one day immediately following a vacation period, one day after a night on call in obstetrics, and one day while in the gynecology clinic. Stress was evaluated by validated psychologic instruments and by levels of plasma testosterone, luteinizing hormone (LH), Cortisol, and prolactin in morning and afternoon blood samples.
Results
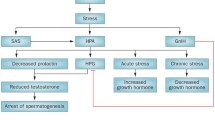
Self-reported stress was significantly elevated during the first 2 weeks of the residency after a night on call. Anxiety scores were significantly elevated after a night on call as were depression subscores for some residents. Plasma testosterone was highly significantly suppressed after the obstetrics night on call and during the first 2 weeks of the residency in comparison with the vacation period. Luteinizing hormone levels were also significantly lower after the obstetrics on-call experience. Plasma Cortisol levels after a night on call were suppressed in the morning and normal or elevated in the afternoon. In comparison, the gynecology rotation was associated with normal levels of testosterone and lower levels of Cortisol.
Conclusion
In this small sample of residents, we observed an inverse relationship between self-reported stress levels and the concentrations of plasma testosterone and LH. The high levels of stress and anxiety expressed after a night on call also disrupted the normal pattern of plasma Cortisol levels.
Similar content being viewed by others
References
Seelig CB, DnPre CT, Adelman HM. Development and validation of a scaled questionnaire for evaluation of residency programs. South Med J 1995;88745–50.
Seelig CB. Quantitating qualitative issues in residency training: development and testing of a scaled program evaluation questionnaire. J Gen Intern Med 1993;8610–3.
del Arco-Galan C, Suarez-Fernandez C, Gabriel-Sanchez R. What happens to blood pressure when on-call? Am J Hypertens 1994;7396–401.
Benbarka MM, Wong GA. Effect of stress of medical residency training on the overnight dexamethasone suppression test. Horm Metab Res 1995;27332–4.
Hudgens GA, Chatterton RT jr, Torre J Jr, et al. Hormonal and psychological profiles in response to a written examination. In: Zmder O, Bresmtz S, eds. Molecular Biology of Stress, UCLA Symposia on Molecular and Cellular Biology, New Series, Vol. 97. New York: Alan R. Liss, 1988;265–75.
Herbert J, Moore GF, de la Riva C, Watts FN. Endocrine responses and examination anxiety. Biol Psychol 1986;22:215– 26.
Chatterton RT Jr. Vogelsong KM, Lu Y-C, Hudgens GA. Hormonal responses to psychological stress in men preparing for skydiving. J Clin Endocrinol Metab 1997;82:2503–9.
Ghanadian R, Puah CM, Williams G, Shah PJR, McWhinney N. Suppressive effects of surgical stress on circulating androgens during and after prostatectomy. Br J Urol 1981;53:147–9.
Fry RW, Morton AR, Garcia-Webb P, Keast D. Monitoring exercise stress by changes in metabolic and hormonal responses over a 24-h period. Eur J Appl Physiol 1991;63:228–34.
Cumming DC, Quigley ME, Yen SS. Acute suppression of circulating testosterone levels by Cortisol in men. J Clin Endocrinol Metab 1983;57:671–3.
Spielberger CD, Gorsuch RL, Lushene R, Vagg PR, Jacobs GA. Manual for the State-Trait Anxiety Inventory (Form Y). Palo Alto, CA: Consulting Psychologists Press, 1983.
Fatkin LT, Hudgens GA, Torre JP Jr, KingJM, Chatterton RT Jr. Psychological responses to competitive marksmanship. In: Torre JP Jr, Wansack S, Hudgens GA, et al, eds. Effects of competition, and mode of fire on physiological responses, psychological stress reactions, and shooting performance. Technical Memorandum 11–91. Aberdeen Proving Ground, MD: U.S. Army Human Engineering Laboratory, 1991;1–10.
Zuckerman M, Lubin B. Manual for the MAACL-R: Multiple Affect Adjective Checklist (Revised). San Diego: Educational and Industrial Testing Service, 1985.
McNair DM, Lorr M, Droppleman LF. Edits Manual for the Profile of Mood States. San Diego: Educational and Industrial Testing Service, 1992.
McCue JD. The distress of internship. Causes and prevention. N Engl J Med 1985;312449–52.
Wheeler GD, Singh M, Pierce WD, Epling WF, Cumming DC. Endurance training decreases serum testosterone levels in men without change in luteinizing hormone pulsatile release. J Clin Endocrinol Metab 1991;72:422–5.
Monden Y, Koshiyama K, Tanaka H, et al. Influence of major surgical stress on plasma testosterone, plasma LH, and urinary steroids. Acta Endocrinol 1972;69542–52.
Johansson GG, Laakso M-L, Peder M, Karonen S-L. Examination stress decreases plasma level luteinizing hormone in male students. Psychosom Med 1988;50:286–94.
Baumgartner A, Riemann D, Berger M. Neuroendocrinological investigations during sleep deprivation in depression. II. Longitudinal measurement of thyrotropin, TH, Cortisol, prolactin, GH, and LH during sleep and sleep deprivation. Biol Psychiat 1990; 28:569–87.
Gonzalez-Santos MR, Gaja-Rodriguez OV, Alonso-Uriate R, Sojo-Aranda I, Cortes-Gallegos V. Sleep deprivation and adaptive hormonal responses of healthy men. Arch Androl 1989;22: 203–7.
Singer F, Zumoff B. Subnormal serum testosterone levels in male medicine residents. Steroids 1990;57:86–9.
Nakashima A, Koshiyama K, Uozumi T, Monden Y, Hamanaka Y. Effects of general anaesthesia and severity of surgical stress on serum LH and testosterone in males. Acta Endocrinol 1975;78: 258–69.
von Treuer K, Norman TR, Armstrong SM. Overnight human plasma melatonin, Cortisol, prolactin. TSH, under conditions of normal sleep, sleep deprivation, and sleep recovery. J Pineal Res 1996;20:7–14.
Weibel L, Follenius M, Spiegel K, Ehrhart J, Brandenberger G. Comparative effect of night and daytime sleep on the 24-hour Cortisol secretory profile. Sleep 1995;18:549–56.
Follenius M, Brandenberger G, Bandesapt JJ, Libert JP, Ehrhart J. Nocturnal Cortisol release in relation to sleep structure. Sleep 1992;15:21–7.
Spath-Schwalbe E, Gofferje M, Kern W, Born J, Fehm HL. Sleep disruption alters nocturnal ACTH and Cortisol secretory patterns. Biol Psychiatry 1991;29:575–84.
Davidson JR, Moldofsky H, Lue FA. Growth hormone and Cortisol secretion in relation to sleep and wakefulness. J Psychiat Neurosci 1991;16:96–102.
Baumgartner A, Graf K-J, Kurten I, Meinhold H, Scholz P. Neuroendocrinological investigations during sleep deprivation in depression. I. Early morning levels of thyrotropin, LH, and Cortisol, prolactin, LH, FSH, estradiol, and testosterone. Biol Psychiat 1990;28:556–68.
Coeck C, Jorens PG, Vandevivere J, Mahler C. ACTH and Cortisol levels during residency training [letter]. N Engl J Med 1991;325:738.
Opstad PK. Androgenic hormones during prolonged physical stress, sleep, and energy deprivation. J Clin Endocrinol Metab 1992;74:1176–83.
Van Cauter E. Diurnal and ultradian rhythms in human endocrine function: a minireview. Horm Res 1990;34:45–53.
Schedlowski M, Wiechert D, Wagner TOF, Tewes U. Acute psychological stress increases plasma levels of Cortisol, prolactin and TSH. Life Sci 1992;50:1201–5.
Jacobs S, Brown SA, Mason J, Wahby V, Kasl S, Ostfeld A. Psychological distress, depression, and prolactin response in stressed persons. J Human Stress 1986;Fall:113–8.
Opstad PK. The hypothalamo-pituitary regulation of androgen secretion in young men after prolonged physicial stress combined with energy and sleep deprivation. Acta Endocrinol 1992;127: 231–6.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chatterton, R.T., Dooley, S.L. Reversal of Diurnal Cortisol Rhythm and Suppression of Plasma Testosterone in Obstetric Residents on Call. Reprod. Sci. 6, 50–54 (1999). https://doi.org/10.1177/107155769900600110
Published:
Issue Date:
DOI: https://doi.org/10.1177/107155769900600110