Abstract
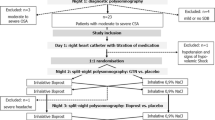
The long-lasting efficacy of the diuretic acetazolamide in the therapy of Cheyne–Stokes respiration (CSR) was assessed in the pilot study in patients with chronic heart failure (СHF) and reduced left ventricular ejection fraction (LVEF). A cohort of 21 patients included in the study had stable CHF II to IV functional class (according to NYHA) and CSR. All patients passed standard clinical-laboratory examinations, the arterial blood gas test, and cardiorespiratory monitoring during sleep. The subjects were randomized into two groups. Patients in the intervention group (n = 10) received a standard medical therapy in combination with a 250-mg dose of acetazolamide once a day while those in the control group (n = 11) received only a standard therapy. The observational period comprised 12 months. The mean apnea-hypopnea index (AHI) in the intervention group decreased significantly after 3 months from 32 to 13 (р = 0.005). No significant changes were observed in AHI in the control group. A statistically significant decrease (from 7.43 to 7.39; p = 0.007) in pH was recorded in the acetazolamide group. During further observation, 1 patient (10%) in the acetazolamide group and 4 patients (36.4%) in the control group died (the difference is nonsignificant). Treatment with acetazolamide at a daily dose of 250 mg significantly reduces the severity of CSR in patients with CHF. Acetazolamide may be recommended for the CSR therapy in patients with CHF.


Similar content being viewed by others
REFERENCES
Russian Society of Cardiology (RSC), 2020 Clinical practice guidelines for chronic heart failure, Ross. Kardiol. Zh., 2020, vol. 25, no. 11, p. 4083.
Driver, H.S., Pereira, E.J., Bjerring, K., et al., Validation of the MediByte type 3 portable monitor compared with polysomnography for screening of obstructive sleep apnea, Can. Respir. J., 2011, vol. 18, no. 3, p. 137.
Javaheri, S., Sleep disorders in systolic heart failure: a prospective study of 100 male patients. The final report, Int. J. Cardiol., 2006, vol. 106, no. 1, p. 21.
Ferrier, K., Campbell, A., Yee, B., et al., Sleep-disordered breathing occurs frequently in stable outpatients with congestive heart failure, Chest, 2005, vol. 128, no. 4, p. 2116.
Eckert, D.J., Jordan, A.S., Merchia, P., and Malhotra, A., Central sleep apnea: pathophysiology and treatment, Chest, 2007, vol. 131, no. 2, p. 595.
Corra, U., Pistono, M., Mezzani, A., et al., Sleep and exertional periodic breathing in chronic heart failure: prognostic importance and interdependence, Circulation, 2006, vol. 113, no. 1, p. 44.
Javaheri, S., Shukla, R., Zeigler, H., and Wexler, L., Central sleep apnea, right ventricular dysfunction, and low diastolic blood pressure are predictors of mortality in systolic heart failure, J. Am. Coll. Cardiol., 2007, vol. 49, no. 20, p. 2028.
Bradley, T.D., Logan, A.G., Kimoff, R.J., et al., Continuous positive airway pressure for central sleep apnea and heart failure, N. Engl. J. Med., 2005, vol. 353, no. 19, p. 2025.
Arzt, M., Floras, J.S., Logan, A.G., et al., Suppression of central sleep apnea by continuous positive airway pressure and transplant-free survival in heart failure: a post hoc analysis of the Canadian Continuous Positive Airway Pressure for Patients with Central Sleep Apnea and Heart Failure Trial (CANPAP), Circulation, 2007, vol. 115, no. 25, p. 3173.
Philippe, C., Stoica-Herman, M., Drouot, X., et al., Compliance with and effectiveness of adaptive servoventilation versus continuous positive airway pressure in the treatment of Cheyne–Stokes respiration in heart failure over a six month period, Heart, 2006, vol. 92, no. 3, p. 337.
Cowie, M.R., Woehrle, H., Wegscheider, K., et al., Adaptive servo-ventilation for central sleep apnea in systolic heart failure, N. Engl. J. Med., 2015, vol. 373, no. 12, p. 1095.
DeBacker, W.A., Verbraecken, J., Willemen, M., et al., Central apnea index decreases after prolonged treatment with acetazolamide, Am. J. Respir. Crit. Care Med., 1995, vol. 151, no. 1, p. 87.
Schmickl, C., Landry, S., Orr, J., et al., Acetazolamide for obstructive and central sleep apnea: a comprehensive systematic review and meta-analysis, Chest, 2020, vol. 158, no. 6, p. 2632.
Wongboonsin, J., Thongprayoon, C., Bathini, T., et al., Acetazolamide therapy in patients with heart failure: a meta-analysis, J. Clin. Med., 2019, vol. 8, no. 3, p. 349.
Aurora, R.N., Chowdhuri, S., Ramar, K., et al., The treatment of central sleep apnea syndromes in adults: practice parameters with an evidence-based literature review and meta-analyses, Sleep, 2012, vol. 35, no. 1, p. 17.
Javaheri, S., Acetazolamide improves central sleep apnea in heart failure: a double-blind, prospecive study, Am. J. Respir. Crit. Care Med., 2006, vol. 173, no. 2, p. 234.
Fontana, M., Emdin, M., Giannoni, A., et al., Effect of acetazolamide on chemosensitivity, Cheyne-Stokes respiration, and response to effort in patients with heart failure, Am. J. Cardiol., 2011, vol. 107, no. 11, p. 1675.
Imiela, T. and Budaj, A., Acetazolamide as an add-on diuretic therapy in patients with chronic heart failure exacerbations: a pilot study, Clin. Drug Investig., 2017, vol. 37, no. 12, p. 1175.
Mullens, W., Damman, K., Harjola, V.-P., et al., The use of diuretics in heart failure with congestion—a position statement from the Heart Failure Association of the European Society of Cardiology, Eur. J. Heart Fail., 2019, vol. 21, no. 2, p. 137.
Mareev, V.Yu., Garganeeva, A.A., Ageev, F.T., et al., The use of diuretics in chronic heart failure: a paper of the Russian Heart Failure Society, Kardiologiya, 2020, vol. 60, no. 12, p. 13.
Ponikowski, P., Voors, A.A., Anker, S.D., et al., 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: the Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) developed with the special contribution of the Heart Failure Association (HFA) of the ESC, Eur. Heart J., 2016, vol. 37, no. 27, p. 2129.
Buzunov, R.V., Palman, A.D., Mel’nikov, A.Yu., et al., Diagnosis and treatment of obstructive sleep apnea syndrome in adults: recommendations of the Russian Society of Somnologists, Eff. Farmakoter., 2018, no. 35, p. 34.
International Classification of Sleep Disorders, Darien, IL: Am. Acad. Sleep Med., 2014, 3rd ed.
Green, C.P., Porter, C.B., Bresnahan, D.R., and Spertus, J.A., Development and evaluation of the Kansas City Cardiomyopathy Questionnaire: a new health status measure for heart failure, J. Am. Coll. Cardiol., 2000, vol. 35, no. 5, p. 1245.
Rector, T.S., Kubo, S.H., and Cohn, J.N., Patients’ self-assessment of their congestive heart failure. Part 2: Content, reliability and validity of a new measure, the Minnesota Living with Heart Failure questionnaire, Heart Failure, 1987, vol. 3, p. 198.
Palman, A.D., Obstructive sleep apnea syndrome, in Aktual’nye problemy pul’monologii (Modern Pulmonology), Moscow: N’yudiamed, 1999.
Mareev, V.Yu., Fomin, I.V., Ageev, F.T., et al., Russian Heart Failure Society, Russian Society of Cardiology. Russian Scientific Medical Society of Internal Medicine Guidelines for Heart failure: chronic (CHF) and acute decompensated (ADHF): diagnostics, prevention, and treatment, Kardiologiya, 2018, vol. 58, no. 6S, p. 8.
Cook, C., Cole, G., Asaria, P., et al., The annual global economic burden of heart failure, Int. J. Cardiol., 2014, vol. 171, no. 3, p. 368.
Grippi, M.A., Pulmonary Pathophysiology, Philadelphia: Lippincott Williams & Wilkins, 1995.
Xie, A., Skatrud, J.B., Puleo, D.S., et al., Apnea-hypopnea threshold for CO2 in patients with congestive heart failure, Am. J. Respir. Crit. Care Med., 2002, vol. 165, no. 9, p. 1245.
Mashkovskii, M.D., Lekarstvennye sredstva (Medical Drugs), Moscow: Novaya Volna, 2019, 16th ed.
Zahedi, K., Barone, S., Xu, J., and Soleimani, M., Potentiation of the effect of thiazide derivatives by carbonic anhydrase inhibitors: molecular mechanisms and potential clinical implications, PLoS One, 2013, vol. 8, no. 11, p. e79327.
Teppema, L.J. and Dahan, A., Acetazolamide and breathing. Does a clinical dose alter peripheral and central CO2 sensitivity? Am. J. Respir. Crit. Care Med., 1999, vol. 160, no. 5, p. 1592.
Bekfani, T. and Abraham, W.T., Current and future developments in the field of central sleep apnoea, Europace, 2016, vol. 18, no. 8, p. 1123.
Nakayama, H., Smith, C.A., Rodman, J.R., et al., Effect of ventilatory drive on CO2 sensitivity below eupnoea during sleep, Am. J. Crit. Care Med., 2002, vol. 165, no. 9, p. 1251.
White, D.P., Zwillich, C.S., Pickett, C.K., et al., Central sleep apnea improvement with acetazolamide therapy, Arch. Int. Med., 1982, vol. 142, no. 10, p. 1816.
Javaheri, S., Sands, S.A., and Edwards, B.A., Acetazolamide attenuates Hunter–Cheyne–Stokes breathing but augments the hypercapnic ventilatory response in patients with heart failure, Ann. Am. Thorac. Soc., 2014, vol. 11, no. 1, p. 80.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
COMPLIANCE WITH ETHICAL STANDARDS
The protocol of the study corresponds to the Helsinki Declaration recommentations and the principles of biomedical ethics and was approved by the local committee on ethics of the Sechenov First Moscow State University of RF Ministry of Health (Sechenov University), Moscow, Russia.
CONFLICT OF INTEREST
The authors declare the absence of evident and potential conflicts of interests associated with the publication of this article.
INFORMED CONSENT
Each participant of the study gave his/her voluntary written informed consent signed after informing him/her about potential risks and advantages, as well as about the nature of the upcoming study .
Additional information
Translated by N. Tarasyuk
Rights and permissions
About this article
Cite this article
Sorokina, K.V., Poltavskaya, M.G., Palman, A.D. et al. Acetazolamide in the Cheyne—Stokes Respiration Therapy in Patients with Chronic Heart Failure: A Pilot Randomized Study. Hum Physiol 48, 78–85 (2022). https://doi.org/10.1134/S0362119721060104
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0362119721060104