Abstract
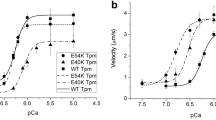
Mutations in the TPM1.1 gene lead to the development of cardiomyopathies. It has been shown that in cardiomyopathies there is a change in the degree of tropomyosin phosphorylation (Tpm). We investigated the molecular mechanisms of the effect of Tpm phosphorylation with mutations associated with dilated (K15N) and hypertrophic (I172T, E180G, and I284V) cardiomyopathies on calcium regulation of actin–myosin interaction using myosin from the atria and ventricles in an in vitro motility assay. Tpm with S283D substitution was used as the phosphorylated form. We found that phosphorylation differently affected regulatory properties of Tpm with mutations depending on their location in the molecule. The phosphorylation did not affect the properties of Tpm with mutations at the N- and C-terminal regions and increased the calcium sensitivity of thin filaments containing Tpm with substitutions in the central part of the molecule. Since hypertrophic cardiomyopathy is accompanied by an increase in the calcium sensitivity, the phosphorylation of the Tpm molecule carrying cardiomyopathic mutations can aggravate the violation of the contractility of the heart chambers.



Similar content being viewed by others
References
Towbin JA (2014) Inherited cardiomyopathies. Circ J 78: 2347–2356. https://doi.org/10.1253/circj.cj-14-0893
Prabhakar R, Boivin GP, Grupp IL, Hoit B, Arteaga G, Solaro JR, Wieczorek DF (2001) A familial hypertrophic cardiomyopathy α-tropomyosin mutation causes severe cardiac hypertrophy and death in mice. J Mol Cell Cardiol 33: 1815–1828. https://doi.org/10.1006/jmcc.2001.1445
Rajan S, Ahmed RP, Jagatheesan G, Petrashevskaya N, Boivin GP, Urboniene D, Arteaga GM, Wolska BM, Solaro RJ, Liggett SB, Wieczorek DF (2007) Dilated cardiomyopathy mutant tropomyosin mice develop cardiac dysfunction with significantly decreased fractional shortening and myofilament calcium sensitivity. Circ Res 101: 205–214. https://doi.org/10.1161/CIRCRESAHA.107.148379
Jagatheesan G, Rajan S, Petrashevskaya N, Schwartz A, Boivin G, Arteaga GM, Solaro RJ, Liggett SB, Wieczorek DF Rescue of tropomyosin-induced familial hypertrophic cardiomyopathy mice by transgenesis. (2007) Am J Physiol Heart Circ Physiol 293: 949–958. https://doi.org/10.1152/ajpheart.01341.2006
Bai F, Wang L, Kawai M (2013) A study of tropomyosin’s role in cardiac function and disease using thin-filament reconstituted myocardium. J Muscle Res Cell Motil 34: 295–310. https://doi.org/10.1007/s10974-013-9343-z
Mahmod M, Raman B, Chan K, Sivalokanathan S, Smillie RW, Samat AHA, Ariga R, Dass S, Ormondroyd E, Watkins H, Neubauer S (2022) Right ventricular function declines prior to left ventricular ejection fraction in hypertrophic cardiomyopathy. J Cardiovasc Magn 24: 36. https://doi.org/10.1186/s12968-022-00868-y
Zhang Y, Zhu Y, Zhang M, Liu J, Wu G, Wang J, Sun X, Wang D, Jiang W, Xu L, Kang L, Song L (2022) Implications of structural right ventricular involvement in patients with hypertrophic cardiomyopathy. Eur Heart J Qual Care Clin Outcomes 9 (1): 34–41. https://doi.org/10.1093/ehjqcco/qcac008
Steen H, Giusca S, Montenbruck M, Patel AR, Pieske B, Florian A, Erley J, Kelle S, Korosoglou G (2021) Left and right ventricular strain using fast strain-encoded cardiovascular magnetic resonance for the diagnostic classification of patients with chronic non-ischemic heart failure due to dilated, hypertrophic cardiomyopathy or cardiac amyloidosis. J Cardiovasc Magn Reson 23: 45. https://doi.org/10.1186/s12968-021-00711-w
Farhad H, Seidelmann SB, Vigneault D, Abbasi SA, Yang E, Day SM, Colan SD, Russell MW, Towbin J, Sherrid MV, Canter CE, Shi L, Jerosch-Herold M, Bluemke DA, Ho C, Neilan TG (2017) Left atrial structure and function in hypertrophic cardiomyopathy sarcomere mutation carriers with and without left ventricular hypertrophy. J Cardiovasc Magn Reson 19: 107. https://doi.org/10.1186/s12968-017-0420-0
Chung H, Kim Y, Park CH, Kim IS, Kim JY, Min PK, Yoon YW, Kim TH, Lee BK, Hong BK, Rim SJ, Kwon HM, Lee KA, Choi EY (2021) Contribution of sarcomere gene mutations to left atrial function in patients with hypertrophic cardiomyopathy. Cardiovasc Ultrasound 19: 4. https://doi.org/10.1186/s12947-020-00233-y
Śpiewak M, Kłopotowski M, Mazurkiewicz Ł, Kowalik E, Petryka-Mazurkiewicz J, Miłosz-Wieczorek B, Klisiewicz A, Witkowski A, Marczak M (2020) Predictors of right ventricular function and size in patients with hypertrophic cardiomyopathy. Sci Rep 10: 21054. https://doi.org/10.1038/s41598-020-78245-x
Prabhakar R, Boivin GP, Grupp IL, Hoit B, Arteaga G, Solaro RJ, Wieczorek DF (2001) A familial hypertrophic cardiomyopathy alpha-tropomyosin mutation causes severe cardiac hypertrophy and death in mice. J Mol Cell Cardiol. 33: 1815–1828. https://doi.org/10.1006/jmcc.2001.1445
Rajan S, Jagatheesan G, Petrashevskaya N, Biesiadecki BJ, Warren CM, Riddle T, Liggett S, Wolska BM, Solaro RJ, Wieczorek DF (2019) Tropomyosin pseudo-phosphorylation results in dilated cardiomyopathy. J Biol Chem 294: 2913–2923. https://doi.org/10.1074/jbc.RA118.004879
Ferrantini C, Coppini R, Pioner JM, Gentile F, Tosi B, Mazzoni L, Scellini B, Piroddi N, Laurino A, Santini L, Spinelli V, Sacconi L, De Tombe P, Moore R, Tardiff J, Mugelli A, Olivotto I, Cerbai E, Tesi C, Poggesi C (2017) Pathogenesis of hypertrophic cardiomyopathy is mutation rather than disease specific: a comparison of the cardiac troponin T E163R and R92Q mouse models. J Am Heart Assoc 6: e005407. https://doi.org/10.1161/JAHA.116.005407
Pioner JM, Vitale G, Gentile F, Scellini B, Piroddi N, Cerbai E, Olivotto I, Tardiff J, Coppini R, Tesi C, Poggesi C, Ferrantini C (2022) Genotype-driven pathogenesis of atrial fibrillation in hypertrophic cardiomyopathy: the case of different TNNT2 mutations. Front Physiol 13: 864547. https://doi.org/10.3389/fphys.2022.864547
Keane S, Fabre A, Keane D (2021) Characterization of atrial histology in a patient with hypertrophic cardiomyopathy: Possible evidence of a primary atrial myopathy. HeartRhythm Case Rep 7: 413–417. https://doi.org/10.1016/j.hrcr.2021.03.017
Kopylova GV, Berg VY, Kochurova AM, Matyushenko AM, Bershitsky SY, Shchepkin DV (2022) The effects of the tropomyosin cardiomyopathy mutations on the calcium regulation of actin-myosin interaction in the atrium and ventricle differ. Biochem Biophys Res Commun 588: 29–33. https://doi.org/10.1016/j.bbrc.2021.12.051
Schulz EM, Correll RN, Sheikh HN, Lofrano-Alves MS, Engel PL, Newman G, Schultz Jel J, Molkentin JD, Wolska BM, Solaro RJ, Wieczorek DF (2012) Tropomyosin dephosphorylation results in compensated cardiac hypertrophy. J Biol Chem 287: 44478–44489. https://doi.org/10.1074/jbc.M112.402040
Schulz EM, Wilder T, Chowdhury SA, Sheikh HN, Wolska BM, Solaro RJ, Wieczorek DF (2013) Decreasing tropomyosin phosphorylation rescues tropomyosin-induced familial hypertrophic cardiomyopathy. J Biol Chem 288: 28925–28935. https://doi.org/10.1074/jbc.M113.466466
Solaro RJ (2002) Modulation of cardiac myofilament activity by protein phosphorylation. In: Page E, Fozzard HA, Solaro RJ (eds) Handbook of Physiology: Section 2; The Cardiovascular System. NY: Oxford University Press, New York, pp 264–300.
Marston S (2022) Recent studies of the molecular mechanism of lusitropy due to phosphorylation of cardiac troponin I by protein kinase A. J Muscle Res Cell Motil 43: 1. https://doi.org/10.1007/s10974-022-09630-4
Ito M, Okamoto R, Ito H, Zhe Y, Dohi K (2022) Regulation of myosin light-chain phosphorylation and its roles in cardiovascular physiology and pathophysiology. Hypertens Res 45: 40–52. https://doi.org/10.1038/s41440-021-00733-y
Markandran K, Yu H, Song W, Lam DTUH, Madathummal MC, Ferenczi MA (2021) Functional and molecular characterisation of heart failure progression in mice and the role of myosin regulatory light chains in the recovery of cardiac muscle function. Int J Mol Sci 23: 88. https://doi.org/10.3390/ijms23010088
Biesiadecki BJ, Westfall MV (2019) Troponin I modulation of cardiac performance: Plasticity in the survival switch. Arch Biochem Biophys 664: 9–14. doi: 10.1016/j.abb.2019.01.025
Westfall MV (2016) Contribution of post-translational phosphorylation to sarcomere-linked cardiomyopathy phenotypes. Front Physiol 7: 407. https://doi.org/10.3389/fphys.2016.00407
Yadav S, Szczesna-Cordary D (2017) Pseudophosphorylation of cardiac myosin regulatory light chain: a promising new tool for treatment of cardiomyopathy. Biophys Rev 9: 57–64. https://doi.org/10.1007/s12551-017-0248-8
Mak A, Smillie LB, Barany M (1978) Specific phosphorylation at serine-283 of alpha tropomyosin from frog skeletal and rabbit skeletal and cardiac muscle. Proc Natl Acad Sci USA 75: 3588–3592. https://doi.org/10.1073/pnas.75.8.3588
Wieczorek DF (2022) Implications of tropomyosin phosphorylation in normal and cardiomyopathic hearts, Medical Research Archives, [online] 10(8) sep. 2022. https://doi.org/10.18103/mra.v10i8.3103
Heeley DH (1994) Investigation of the effects of phosphorylation of rabbit striated muscle alpha alpha-tropomyosin and rabbit skeletal muscle troponin-T. Eur J Biochem 221: 129–137. https://doi.org/10.1111/j.1432-1033.1994.tb18721.x
Heeley DH, Watson MH, Mak AS, Dubord P, Smillie LB (1989) Effect of phosphorylation on the interaction and functional properties of rabbit striated muscle alpha alpha-tropomyosin. J Biol Chem 264: 2424–2430.
Lehman W, Medlock G, Li XE, Suphamungmee W, Tu AY, Schmidtmann A, Ujfalusi Z, Fischer S, Moore JR, Geeves MA, Regnier M (2015) Phosphorylation of Ser283 enhances the stiffness of the tropomyosin head-to-tail overlap domain. Arch Biochem Biophys 571: 10–15. https://doi.org/10.1016/j.abb.2015.02.026
Sano K, Maeda K, Oda T, Maéda Y (2000) The effect of single residue substitutions of serine-283 on the strength of head-to-tail interaction and actin binding properties of rabbit skeletal muscle alpha-tropomyosin. J Biochem 127: 1095–1102. https://doi.org/10.1093/oxfordjournals.jbchem.a022703
Rao VS, Marongelli EN, Guilford WH (2009) Phosphorylation of tropomyosin extends cooperative binding of myosin beyond a single regulatory unit. Cell Motil Cytoskeleton 66: 10–23. https://doi.org/10.1002/cm.20321
Kopylova GV, Matyushenko AM, Berg VY, Levitsky DI, Bershitsky SY, Shchepkin DV (2021) Acidosis modifies effects of phosphorylated tropomyosin on the actin-myosin interaction in the myocardium. J Muscle Res Cell Motil 42: 343–353. https://doi.org/10.1007/s10974-020-09593-4
Nixon BR, Liu B, Scellini B, Tesi C, Piroddi N, Ogut O, Solaro RJ, Ziolo MT, Janssen PM, Davis JP, Poggesi C, Biesiadecki BJ (2013) Tropomyosin Ser-283 pseudo-phosphorylation slows myofibril relaxation. Arch Biochem Biophys 535: 30–38. https://doi.org/10.1016/j.abb.2012.11.010
Nefedova VV, Koubassova NA, Borzova VA, Kleymenov SY, Tsaturyan AK, Matyushenko AM, Levitsky DI (2021) Tropomyosin pseudo-phosphorylation can rescue the effects of cardiomyopathy-associated mutations. Int J Biol Macromol 166: 424–434. https://doi.org/10.1016/j.ijbiomac.2020.10.201.
Margossian SS, Lowey S (1982) Preparation of myosin and its subfragments from rabbit skeletal muscle. Methods Enzymol 85 (Pt B): 55–71. https://doi.org/10.1016/0076-6879(82)85009-x
Reiser PJ, Kline WO (1998) Electrophoretic separation and quantitation of cardiac myosin heavy chain isoforms in eight mammalian species. Am J Physiol 274: 1048–1053. https://doi.org/10.1152/ajpheart.1998.274.3.H1048
Pardee JD, Spudich JA (1982) Purification of muscle actin. Methods Enzymol 85 (Pt B): 164–181. https://doi.org/10.1016/0076-6879(82)85020-9
Potter JD (1982) Preparation of troponin and its subunits. Methods Enzymol 85 (Pt B): 241–263. https://doi.org/10.1016/0076-6879(82)85024-6
Kron SJ, Spudich JA (1986) Fluorescent actin filaments move on myosin fixed to a glass surface. Proc Natl Acad Sci USA 83: 6272–6276. https://doi.org/10.1073/pnas.83.17.6272
Matyushenko AM, Shchepkin DV, Kopylova GV, Popruga KE, Artemova NV, Pivovarova AV, Bershitsky SY, Levitsky DI (2017) structural and functional effects of cardiomyopathy-causing mutations in the troponin T-binding region of cardiac tropomyosin. Biochemistry 56: 250–259. https://doi.org/10.1021/acs.biochem.6b00994
Mashanov GI, Molloy JE (2007) Automatic detection of single fluorophores in live cells. Biophys J 92: 2199–2211. https://doi.org/10.1529/biophysj.106.081117
Schulz EM, Wieczorek DF. Tropomyosin de-phosphorylation in the heart: what are the consequences? J Muscle Res Cell Motil 34: 239–246. doi: 10.1007/s10974-013-9348-7
Warren CM, Arteaga GM, Rajan S, Ahmed RP, Wieczorek DF, Solaro RJ (2008) Use of 2-D DIGE analysis reveals altered phosphorylation in a tropomyosin mutant (Glu54Lys) linked to dilated cardiomyopathy. Proteomics 8: 100–105. https://doi.org/10.1002/pmic.200700772
Huang W, Szczesna-Cordary D (2015) Molecular mechanisms of cardiomyopathy phenotypes associated with myosin light chain mutations. J Muscle Res Cell Motil 36: 433–445. https://doi.org/10.1007/s10974-015-9423-3
Yadav S, Kazmierczak K, Liang J, Sitbon YH, Szczesna-Cordary D (2019) Phosphomimetic-mediated in vitro rescue of hypertrophic cardiomyopathy linked to R58Q mutation in myosin regulatory light chain. FEBS J 286: 151–168. https://doi.org/10.1111/febs.14702
Yuan CC, Muthu P, Kazmierczak K, Liang J, Huang W, Irving TC, Kanashiro-Takeuchi RM, Hare JM, Szczesna-Cordary D (2015) Constitutive phosphorylation of cardiac myosin regulatory light chain prevents development of hypertrophic cardiomyopathy in mice. Proc Natl Acad Sci USA 112: E4138–E4146. https://doi.org/10.1073/pnas.1505819112
Rababa’h A, Singh S, Suryavanshi SV, Altarabsheh SE, Deo SV, McConnell BK (2014) Compartmentalization role of A-kinase anchoring proteins (AKAPs) in mediating protein kinase A (PKA) signaling and cardiomyocyte hypertrophy. Int J Mol Sci 16: 218–229. https://doi.org/10.3390/ijms16010218
Zhang X, Wang BZ, Kim M, Nash TR, Liu B, Rao J, Lock R, Tamargo M, Soni RK, Belov J, Li E, Vunjak-Novakovic G, Fine B (2022) STK25 inhibits PKA signaling by phosphorylating PRKAR1A. Cell Rep 40: 111203. https://doi.org/10.1016/j.celrep.2022.111203
Oliveira-Santos A, Dagda M, Burkin DJ (2022) Sunitinib inhibits STAT3 phosphorylation in cardiac muscle and prevents cardiomyopathy in the mdx mouse model of Duchenne muscular dystrophy. Hum Mol Genet 31: 2358–2369. https://doi.org/10.1093/hmg/ddac042
Dmour BA, Miftode RS, Iliescu Halitchi D, Anton-Paduraru DT, Iliescu Halitchi CO, Miftode IL, Mitu O, Costache AD, Stafie CS, Costache II (2021) Latest insights into mechanisms behind atrial cardiomyopathy: It is not always about ventricular function. Diagnostics (Basel) 11: 449. https://doi.org/10.3390/diagnostics11030449
Packer M (2020) Characterization, pathogenesis, and clinical implications of inflammation-related atrial myopathy as an important cause of atrial fibrillation. J Am Heart Assoc 9: e015343. https://doi.org/10.1161/JAHA.119.015343
Carlisle MA, Fudim M, DeVore AD, Piccini JP (2019) Heart failure and atrial fibrillation, like fire and fury. JACC Heart Fail 7: 447–456. https://doi.org/10.1016/j.jchf.2019.03.005
Thierfelder L, MacRae C, Watkins H, Tomfohrde J, Williams M, McKenna W, Bohm K, Noeske G, Schlepper M, Bowcock A (1993) A familial hypertrophic cardiomyopathy locus maps to chromosome 15q2. Proc Natl Acad Sci USA 90: 6270–6274. https://doi.org/10.1073/pnas.90.13.6270
Van Driest SL, Ellsworth EG, Ommen SR, Tajik AJ, Gersh BJ, Ackerman MJ (2003) Prevalence and spectrum of thin filament mutations in an outpatient referral population with hypertrophic cardiomyopathy. Circulation 108: 445–451. https://doi.org/10.1161/01.CIR.0000080896.52003.DF
Acknowledgments
The authors would like to thank V.Y. Berg for her assistance in the in vitro motility assay experiments.
Funding
This work was funded by the Russian Foundation for Basic Research grants 20-04-00130 (S.B.), State Program 122022200089-4 (S.B.), and State Program 122041100022-3 (A.M.). The work was performed using the equipment of the Shared Research Center of Scientific Equipment of IIP UB RAS and the equipment of the Shared-Access Equipment Centre “Industrial Biotechnology” of Federal Research Center “Fundamentals of Biotechnology” of the RAS.
Author information
Authors and Affiliations
Contributions
G.V.K., A.M.M., S.Y.B., and D.V.S. conceptualized the work; A.M.M. expressed of tropomyosins; G.V.K., A.M.K., and D.V.S. performed in vitro motility experiments and analyzed data; G.V.K., S.Y.B., and D.V.S. wrote the manuscript; all authors read and approved the manuscript.
Corresponding author
Ethics declarations
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Additional information
Translated by A. Polyanovsky
Rights and permissions
About this article
Cite this article
Kopylova, G.V., Matyushenko, A.M., Kochurova, A.M. et al. Effects of Phosphorylation of Tropomyosin with Cardiomyopathic Mutations on Calcium Regulation of Myocardial Contraction. J Evol Biochem Phys 58 (Suppl 1), S82–S91 (2022). https://doi.org/10.1134/S0022093022070092
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0022093022070092