Abstract
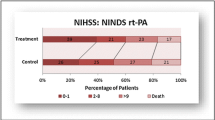
Introduction: Systemic thrombolytic therapy (STLT) with recombinant tissue plasminogen activator (rtPA) is the “gold standard” of reperfusion therapy in certain patients with ischemic stroke during the first 4.5 h after stroke onset. Objective: To assess the clinical (severity of neurological symptoms) and laboratory (complete blood cell count test) factors that affect the disease outcome after STLT. Materials and methods: Seventy patients (48 males and 22 females) aged 61 [54; 69] years with ischemic stroke who received rtPA therapy at a dose of 0.9 mg/kg were prospectively studied. Blood for the complete blood count test including neutrophil and lymphocyte counts was sampled before the thrombolytic therapy. The severity of neurological impairment was assessed using the NIH Stroke Scale (NIHSS). The functional outcome was assessed 3 months after stroke with the modified Rankin scale (mRS). ROC analysis was used to reveal factors of unfavorable outcome in acute phase of ischemic stroke (mRS score ≥ 3). Results: Severity of neurological deficit was assessed according to the NIHSS at admission was 15 [11; 17] points. Time between the manifestation of neurological symptoms and admission to the hospital was 138 [117; 170] min, and time between admission and initiation of STLT (the door-to-needle time), was 40 [30; 55] min. An unfavourable functional outcome of systemic thrombolytic therapy can be predicted according to the results of ROC analysis: the NIHSS score upon admission 12 or higher (sensitivity, 94%; specificity, 57%); neutrophil count, >7.8 × 109/L (sensitivity, 45.5%; specificity, 90.6%); lymphocyte count < 1.8 × 109/L (sensitivity, 81.8%; specificity, 59.4%). Conclusions: Personalized approach to systemic thrombolytic therapy may help to predict its effectiveness and contribute the development of more reliable strategies of patient management. Patients with potentially unfavorable outcome after intravenous thrombolysis can be the target group for mechanical reperfusion techniques such as thrombus extraction.

Similar content being viewed by others
REFERENCES
Powers, W.J., Derdeyn, C.P., Biller, J., et al., 2015 AHA/ASA focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment. A Guideline for healthcare professionals from the American Heart Association/American Stroke Association, Stroke, 2015, vol. 46, no. 10, pp. 3020–3035. PMID 26123479. doi 10.1161/STR.0000000000000074
Skvortsova, V.I., Golukhov, G.N., Gubskii, L.V., et al., Systemic thrombolysis in ischemic stroke, Zh. Nevropatol. Psikhiatr. im. S.S. Korsakova, 2006, vol. 106, no. 12, pp. 24–31.
Domashenko, M.A., Maksimova, M.Yu., Loskutnikov, M.A., et al., Systemic thrombolysis in acute ischemic stroke, Ann. Klin. Eksp. Nevrol., 2008, vol. 2, pp. 5–12.
Domashenko, M.A., Maksimova, M.Yu., Loskutnikov, M.A., et al., Mechanisms of reperfusion with intravenous thrombolytic therapy in patients with ischemic stroke, Nevrol., Neiropsikhiatriya, Psikhosom., 2012, vol. 4, pp. 53–58.
Piradov, M.A., Domashenko, M.A., and Maksimo-va, M.Yu. Reperfusion treatment of ischemic stroke, in Nevrologiya XXI veka: diagnosticheskie, lechebnye i issledovatel’skie tekhnologii. Rukovodstvo dlya vrachei (Neurology of 21 Century: Diagnostics, Medical Course, and Study Technologies. Manual for Physicians), Pira-dov, M.A., Illarioshkin, S.N., and Tanashyan, M.M., Eds., Moscow: ATMO, 2015, vol. 2, pp. 9–45.
Skvortsova, V.I., Stakhovskaya, L.V., Lelyuk, V.G., et al., Development of the care system for stroke patients in Russian Federation, Materialy Vserossiiskoi nauchno-prakticheskoi konferentsii “Sovershenstvovanie okazaniya meditsinskoi pomoshchi bol’nym s sosudistymi zabolevaniyami” (Proc. All-Russ. Sci.-Pract. Conf. “Improvement of Medical Care for Patients with Vascular Diseases”), Yaroslavl, 2011, pp. 13–33.
Shamalov, N.A. Problems and prospects of reperfusion therapy in ischemic stroke in Russia, Farmateka, 2015, vol. 9, pp. 14–19.
Emberson, J., Lees, K.R., Lyden, P., et al., Effect of treatment delay, age, and stroke severity on the effects of intravenous thrombolysis with alteplase for acute ischemic stroke: a meta-analysis of individual patient data from randomized trials, Lancet, 2014, vol. 384, no. 9958, pp. 1929–1935. PMID 25106063. http:// dx.doi.org/10.1016/S0140-6736(14)60584-5.
Lees, K., Bluhmki, E., von Kummer, R., et al., Time to treatment with intravenous alteplase and outcome in stroke: an updated pooled analysis of ECASS, ATLANTIS, NINDS, and EPITHET trials, Lancet, 2010, vol. 375, pp. 1695–1703. PMID 20472172. http://dx. doi.org/10.1016/S0140-6736(10)60491-6.
Sandercock, P., Wardlaw, J.M., Lindley, R.I., et al., The benefits and harms of intravenous thrombolysis with recombinant tissue plasminogen activator within 6 h of acute ischemic stroke (the Third International Stroke Trial [IST-3]): a randomized controlled trial, Lancet, 2012, vol. 379, pp. 2352–2363. PMID 22632908. doi 10.1016/S0140-6736(12)60768-5
Hacke, W., Kaste, M., Bluhmki, E., et al., Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke, N. Engl. J. Med., 2008, vol. 359, pp. 1317–1329. PMID 18815396. http://dx.doi.org/10.1056/NEJMoa0804656.
Shamalov, N.A., Optimization of reperfusion therapy in patients with ischemic stroke, Extended Abstract of Doctoral (Med.) Dissertation, Moscow, 2012.
Lansberg, M.G., Thijs, V.N., Bammer, R., et al., Risk factors of symptomatic intracerebral hemorrhage after tPA therapy for acute stroke, Stroke, 2007, vol. 38, pp. 2275–2278. PMID 17569874. https://doi.org/ 10.1161/STROKEAHA.106.480475.
Urbach, H., Hartmann, A., Pohl, C., et al., Local intra-arterial thrombolysis in the carotid territory: does recanalization depend on the thromboembolus type? Neuroradiology, 2002, vol. 44, pp. 695–699. PMID 12185548. http://dx.doi.org/10.1007/s00234-002-0762-6.
Bhatia, R., Hill, M.D., Shobha, N., et al., Low rates of acute recanalization with intravenous recombinant tissue plasminogen activator in ischemic stroke: real-world experience and a call for action, Stroke, 2010, vol. 41, no. 10, pp. 2254–2258. PMID 20829513. http://dx.doi.org/10.1161/STROKEAHA.110.592535.
Broderick, J.P., Palesch, Y.Y., Demchuk, A.M., et al., Endovascular therapy after intravenous t-PA versus t-PA alone for stroke, N. Engl. J. Med., 2013, vol. 368, no. 10, pp. 893–903. PMID 23390923. http://dx. doi.org/10.1056/NEJMoa1214300.
Riedel, C.H., Zimmermann, P., Jensen-Kondering, U., et al., The importance of size: successful recanalization by intravenous thrombolysis in acute anterior stroke depends on thrombus length, Stroke, 2011, vol. 42, no. 6, pp. 1775–1777. PMID 21474810. http://dx.doi.org/10.1161/STROKEAHA.110.609693
Del Zoppo, C.J., Poeck, K., Pessin, M.S., et al., Recombinant tissue plasminogen activator in acute thrombotic and embolic stroke, Ann. Neurol., 1992, vol. 32, pp. 78–86. PMID 1642475. http://dx.doi.org/ 10.1002/ana.410320113.
Mori, E., Yoneda, Y., Tabuchi, M., et al., Intravenous recombinant tissue plasminogen activator in acute carotid territory stroke, Neurology, 1992, vol. 42, pp. 976–982. PMID 1579252
Adams, H., Del Zoppo, G., Alberts, M., et al., Guidelines for the management of adults with ischemic stroke, Stroke, 2007, vol. 38, pp. 1655–1711. PMID 17431204. doi 10.1161/STROKEAHA.107.181486
Cucchiara, B., Tanne, D., Levine, S.R., et al., A risk score to predict intracranial hemorrhage after recombinant tissue plasminogen activator for acute ischemic stroke, J. Stroke Cerebrovasc. Dis., 2008, vol. 17, pp. 331–333. PMID 18984422. http://dx.doi.org/ 10.1016/j.jstrokecerebrovasdis.2008.03.012.
Saqqur, M., Shuaib, A., Alexandrov, A.V., et al., The correlation between admission blood glucose and intravenous rt-PA-induced arterial recanalization in acute ischemic stroke: a multi-centre TCD study, Int. J. Stroke, 2015, vol. 10, no. 7, pp. 1087–1092. PMID 26332252. doi 10.1111/ijs.12517
Vanacker, P., Heldner, M.R., Seiffge, D., et al., ASTRAL-R score predicts non-recanalisation after intravenous thrombolysis in acute ischemic stroke, Thromb. Haemostasis, 2015, vol. 113, no. 5, pp. 911–917. PMID 25854290. http://dx.doi.org/10.1160/TH14-06-0482.
Demchuk, A.M., Morgenstern, L.B., Krieger, D.W., et al., Serum glucose level, and diabetes predict tissue plasminogen activator-related intracerebral hemorrhage in acute ischemic stroke, Stroke, 1999, vol. 30, no. 1, pp. 34–39. PMID 9880385. http:// dx.doi.org/10.1161/01.STR.30.1.34.
Whiteley, W.N., Slot, K.B., Fernandes, P., et al., Risk factors for intracranial hemorrhage in acute ischemic stroke patients treated with recombinant tissue plasminogen activator: a systematic review and meta-analysis of 55 studies, Stroke, 2012, vol. 43, no. 11, pp. 2904–2909. PMID 22996959. http://dx.doi. org/10.1161/STROKEAHA.112.665331.
Rocco, A., Heuschmann, P.U., Schellinger, P.D., et al., Glycosylated hemoglobin A1 predicts risk for symptomatic hemorrhage after thrombolysis for acute stroke, Stroke, 2013, vol. 44, no. 8, pp. 2134–2138. PMID 23715962. https://doi.org/10.1161/ STROKEAHA.111.675918.
Masrur, S., Cox, M., Bhatt, D.L., et al., Association of acute and chronic hyperglycemia with acute ischemic stroke outcomes post thrombolysis: findings from get with the guidelines stroke, J. Am. Heart Assoc., 2015, vol. 4, no. 10, p. e002193. PMID 26408015. https://doi.org/10.1161/JAHA.115.002193/
Tanashyan, M.M., Suslina, Z.A., Ionova, V.G., et al., Endothelial function in patients with ischemic stroke at different degrees carotid artery atherosclerosis, Nevrol. Vestn. Zh. im. V.M. Bekhtereva, 2007, vol. 29, no. 1, pp. 12–16.
Author information
Authors and Affiliations
Corresponding author
Additional information
The article is published in the original.
Rights and permissions
About this article
Cite this article
Domashenko, M.A., Maksimova, M.Y., Gafarova, M.E. et al. Personified Approaches to Reperfusion Therapy of Ischemic Stroke. Hum Physiol 44, 869–874 (2018). https://doi.org/10.1134/S0362119718080030
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1134/S0362119718080030